Nanotechnology in Targeted Drug Delivery: Current Platforms, Clinical Translation, and Future Directions
This article provides a comprehensive analysis of the application of nanotechnology in targeted drug delivery systems for a professional audience of researchers and drug development scientists.
Nanotechnology in Targeted Drug Delivery: Current Platforms, Clinical Translation, and Future Directions
Abstract
This article provides a comprehensive analysis of the application of nanotechnology in targeted drug delivery systems for a professional audience of researchers and drug development scientists. It explores the foundational principles of nanocarrier design, including key platforms like lipid nanoparticles, polymeric systems, and inorganic nanoparticles. The scope covers methodological advances in active and passive targeting, tackles critical challenges in manufacturing and translational science, and evaluates the current clinical and regulatory landscape. By synthesizing recent data and future trends, this review serves as a strategic resource for navigating the development of next-generation nanomedicines.
The Foundations of Nanomedicine: Principles and Nanoparticle Platforms
Core Defining Parameters of Nanoscale Drug Delivery Systems
Nanoscale Drug Delivery Systems (NDDS) are engineered materials with at least one dimension between 1 to 100 nanometers, though for biomedical applications, the effective size range often extends to several hundred nanometers. [1] Working at this scale unlocks unique physicochemical properties that are critical for overcoming the limitations of conventional drug delivery.
The table below summarizes the fundamental nanoscale parameters that define a NDDS and their primary roles in drug delivery.
Table 1: Core Defining Parameters of Nanoscale Drug Delivery Systems
| Parameter | Definition & Typical Range | Role in Drug Delivery |
|---|---|---|
| Size | 1–100 nm in at least one dimension; effective intravenous range is up to 5 μm to avoid capillary embolism. Optimal EPR effect is seen with particles of 50–200 nm. [2] [1] | Governs biodistribution, circulation time, cellular uptake, and tumor penetration via the Enhanced Permeability and Retention (EPR) effect. [2] |
| Surface Charge | Measured as Zeta potential; can be cationic (positive), anionic (negative), or neutral. | Influences colloidal stability, interaction with cell membranes (cellular uptake), and protein corona formation. [3] |
| Surface Chemistry | The chemical composition and functional groups present on the nanoparticle surface. | Determines biocompatibility, stealth properties (e.g., via PEGylation), and provides attachment points for active targeting ligands. [4] [5] |
| Shape & Morphology | Includes spherical micelles, cylindrical structures, vesicles (polymersomes/liposomes), and other defined geometries. [4] | Affects flow dynamics, margination toward vessel walls, and internalization efficiency by target cells. [4] |
| Drug Release Profile | The kinetics of API release from the nanocarrier (e.g., burst, sustained, or stimuli-responsive). | Critical for achieving therapeutic drug levels at the target site while minimizing systemic exposure and toxicity. [4] [6] |
Experimental Protocols for Key Characterization assays
Protocol: Determining Nanoparticle Size, Size Distribution, and Surface Charge
This protocol outlines the use of Dynamic Light Scattering (DLS) and Electrophoretic Light Scattering (ELS) to characterize the hydrodynamic diameter, polydispersity (PDI), and zeta potential of NDDS. [4]
- Principle: DLS measures Brownian motion to calculate particle size, while ELS measures particle mobility under an electric field to determine surface charge.
- Materials:
- Nanoparticle suspension
- Disposable folded capillary zeta cells
- Cuvettes for size measurement
- Appropriate dispersion medium (e.g., purified water, phosphate-buffered saline)
- DLS/ELS instrument (e.g., Zetasizer)
- Procedure:
- Sample Preparation: Dilute the nanoparticle suspension with a clear, particle-free dispersion medium to an optimal concentration that avoids signal saturation (multiple scattering) or weak signal. Filter the sample through a 0.45 μm or 0.2 μm syringe filter if necessary to remove dust.
- Equipment Setup: Turn on the instrument and laser, allowing for sufficient warm-up time. Set the measurement temperature to 25°C.
- Size Measurement (DLS):
- Transfer the diluted sample into a disposable sizing cuvette.
- Place the cuvette in the instrument.
- Set the number of runs and measurement duration per run (typically 10-15 runs).
- Initiate measurement. The software will report the Z-average diameter (hydrodynamic size) and the Polydispersity Index (PDI).
- Zeta Potential Measurement (ELS):
- Carefully load the sample into a disposable zeta potential cell using a syringe, avoiding air bubbles.
- Insert the cell into the instrument.
- Set the field voltage and select the appropriate model for Henry's function calculation.
- Perform at least 3-12 measurements per sample and calculate the mean zeta potential and standard deviation.
- Data Interpretation:
- Z-Average: Represents the intensity-weighted mean hydrodynamic size.
- PDI: Values below 0.1 indicate a highly monodisperse sample; values above 0.3 suggest a broad size distribution.
- Zeta Potential: Values greater than +30 mV or less than -30 mV typically indicate good physical stability due to strong electrostatic repulsion.
Protocol: Nuclear Magnetic Resonance (NMR) Analysis of Polymeric Nanoparticles
NMR spectroscopy is a powerful technique for confirming polymer structure, monitoring polymerization conversion, and verifying drug conjugation. [4]
- Principle: NMR detects the magnetic properties of atomic nuclei (e.g., ^1H, ^13C) to provide information on molecular structure, dynamics, and environment.
- Materials:
- Lyophilized or concentrated nanoparticle sample
- Deuterated solvent (e.g., CDCl₃, D₂O)
- NMR tubes
- High-resolution NMR spectrometer
- Procedure:
- Sample Preparation: Dissolve 2-10 mg of the nanoparticle or polymer sample in 0.6-0.7 mL of an appropriate deuterated solvent. Transfer the solution to a clean, dry NMR tube.
- Data Acquisition:
- Insert the sample tube into the magnet.
- For ^1H NMR, standard parameters are used (e.g., 90° pulse, 10-15 sec relaxation delay, 16-64 scans).
- Acquire the spectrum. For more detailed structural analysis, 2D NMR techniques like COSY, HSQC, or HMBC can be employed. [4]
- Diffusion-Ordered NMR Spectroscopy (DOSY) can be used to estimate molecular weights. [4]
- Data Analysis:
- Reference the spectrum to the residual proton signal of the deuterated solvent.
- Identify peaks corresponding to the polymer backbone, functional groups, and conjugated drugs or dyes.
- Calculate monomer conversion by comparing the integral of vinyl proton signals from the monomer to the integral of polymer chain signals.
- Quantify drug loading efficiency by comparing the integrals of characteristic drug peaks to polymer backbone peaks.
The following diagram illustrates the logical workflow for the comprehensive characterization of a NDDS, integrating the protocols described above.
Protocol: Analysis of Protein Corona Formation
Understanding the nano-bio interface is critical, as nanoparticles in biological fluids rapidly adsorb proteins, forming a "corona" that defines their biological identity. [3]
- Principle: Incubate nanoparticles with relevant biological fluid (e.g., human plasma), isolate the nanoparticle-protein corona complex, and identify the adsorbed proteins.
- Materials:
- Nanoparticle suspension
- Human plasma or serum (preferably from relevant disease demographics)
- Ultracentrifuge and rotors
- Phosphate Buffered Saline (PBS)
- SDS-PAGE gel or Mass Spectrometry equipment
- Procedure:
- Corona Formation: Incubate a known concentration of nanoparticles with 1 mL of human plasma (e.g., 1:1 v/v ratio) for a predetermined time (e.g., 0.5 to 60 minutes) at 37°C with gentle agitation.
- Isolation of Hard Corona: Centrifuge the mixture at high speed (e.g., 100,000 × g for 1 hour) to pellet the nanoparticle-corona complex.
- Washing: Carefully remove the supernatant and gently wash the pellet with cold PBS to remove loosely associated proteins (soft corona). Repeat centrifugation.
- Protein Elution and Analysis:
- Re-suspend the final pellet in SDS-PAGE loading buffer to elute proteins.
- Heat the sample and load onto an SDS-PAGE gel for protein separation and Coomassie/silver staining.
- For precise identification, use liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) to characterize the protein composition of the corona.
- Data Interpretation: Analyze the MS data to identify the most abundant proteins in the corona (e.g., albumin, immunoglobulins, apolipoproteins). Correlate the corona composition with changes in nanoparticle physicochemical properties and its impact on cellular uptake and drug release kinetics. [3]
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development and characterization of NDDS rely on a suite of specialized materials and reagents.
Table 2: Key Research Reagent Solutions for NDDS Development
| Reagent / Material | Function & Application |
|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable and FDA-approved polymer used to form nanoparticles for controlled drug release. [7] |
| DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine) | A phospholipid used as a primary component in liposomes and lipid nanoparticles, forming the core bilayer structure. |
| PEG-lipid (e.g., DMG-PEG2000) | Used for surface PEGylation ("stealth" coating) to reduce protein adsorption, prolong circulation time, and improve stability. [7] [5] |
| Ionizable Cationic Lipids (e.g., DLin-MC3-DMA) | Critical for mRNA encapsulation in LNPs; ionizable at low pH to facilitate endosomal escape. [7] |
| Targeting Ligands (e.g., Antibodies, Peptides) | Conjugated to the nanoparticle surface for active targeting of specific cell surface receptors (e.g., PD-L1 antibodies for cancer). [5] |
| Deuterated Solvents (e.g., CDCl₃, D₂O) | Essential for NMR spectroscopy to analyze polymer structure, drug conjugation, and nanoparticle "livingness." [4] |
| Human Plasma (from various demographics) | Used for in vitro protein corona studies to better simulate the complex biological environment encountered in vivo. [3] |
Critical Considerations for Clinical Translation
The journey from a well-characterized NDDS in the lab to a clinically viable product involves navigating several critical hurdles.
- Manufacturing and Scalability: Transitioning from lab-scale synthesis (e.g., nanoprecipitation) to Good Manufacturing Practice (GMP) compliant, large-scale production is a major challenge. Advanced manufacturing technologies like microfluidics and 3D printing are being explored for better control and reproducibility. [2] Maintaining batch-to-batch consistency in Critical Quality Attributes (CQAs) like size, PDI, and drug loading is paramount. [7] [2]
- Biological Hurdles: The Protein Corona significantly alters the nanoparticle's synthetic identity, impacting its targeting capability, immune response, biodistribution, and cargo release profile. [3] A major challenge is evading hepatic uptake to improve extrahepatic targeting. Strategies include modulating size, surface charge, and employing sophisticated surface coatings to avoid rapid clearance by the reticuloendothelial system (RES). [8]
- Regulatory Pathways: The complexity of NDDS presents challenges for regulatory bodies. Demonstrating a robust safety profile, including long-term biodistribution, biodegradation, and nanotoxicology data, is essential for approval. [7] [1] Implementing a Quality-by-Design (QbD) framework and Process Analytical Technology (PAT) for real-time monitoring is increasingly important for regulatory compliance. [1]
Concluding Synthesis
Defining a NDDS requires a multi-faceted approach that integrates precise control over its size, surface properties, and morphology with a deep understanding of its dynamic biological interactions, particularly the protein corona. Rigorous characterization using the outlined protocols is non-negotiable for establishing structure-property-performance relationships. While challenges in manufacturing, scalability, and safety remain significant, the continued evolution of nanoscale fabrication and characterization technologies holds immense promise for bridging the translational gap and realizing the full potential of targeted nanomedicines.
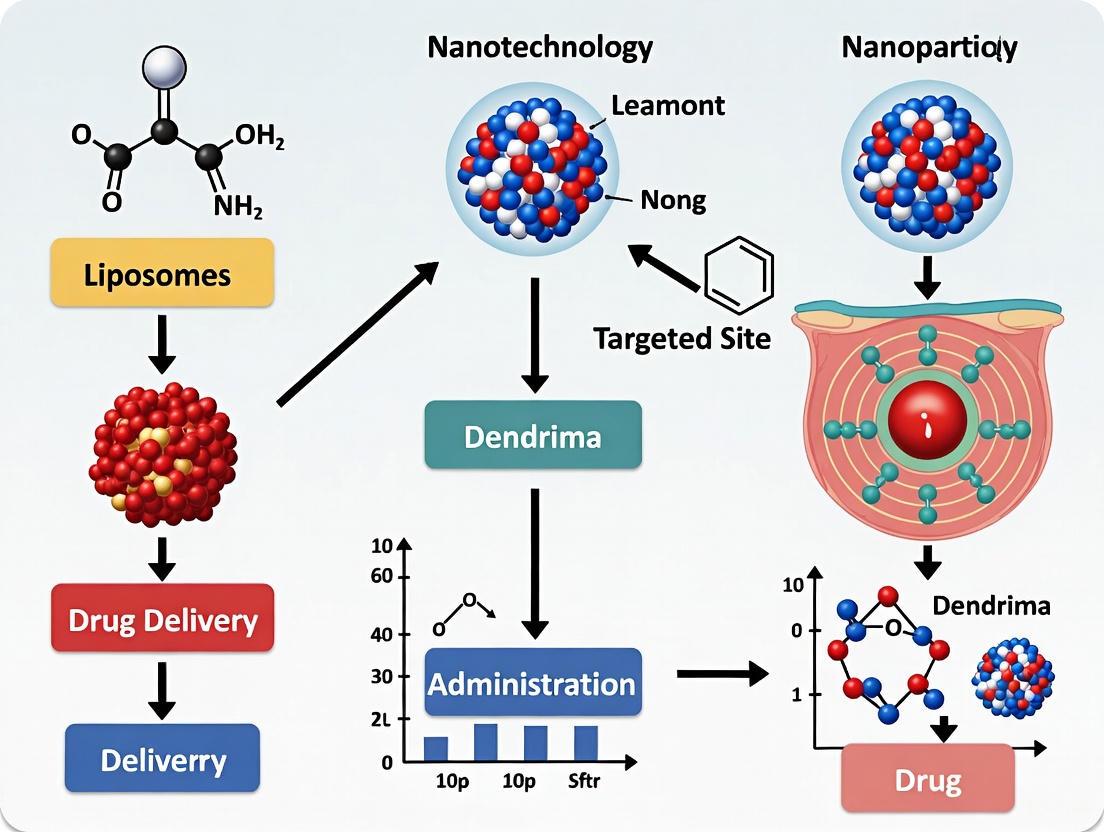
Within the broader scope of applying nanotechnology in targeted drug delivery systems research, three nanoparticle platforms have emerged as foundational: liposomes, lipid nanoparticles (LNPs), and polymeric nanoparticles. These systems offer distinct advantages for encapsulating and delivering therapeutic agents, improving their bioavailability, and enabling targeted delivery to specific tissues while minimizing off-target effects [9] [10] [11]. This document provides detailed application notes and experimental protocols for these core platforms, focusing on their design, characterization, and implementation in pharmaceutical research and development. The content is structured to provide researchers with practical methodologies and comparative data to inform platform selection for specific therapeutic applications.
Liposomes
Application Notes
Liposomes are spherical nanocarriers composed of one or more concentric lipid bilayers enclosing an aqueous core. Their biomimetic architecture, which is structurally similar to cellular membranes, grants them high biocompatibility and the ability to encapsulate both hydrophilic (in the aqueous core) and hydrophobic (within the lipid bilayer) active ingredients [9] [12]. A key clinical feature is their ability to accumulate in malignant or inflamed tissues via the Enhanced Permeability and Retention (EPR) effect, which takes advantage of the leaky vasculature and poor lymphatic drainage typical of these pathological sites [9]. Advances in liposomal engineering, such as PEGylation (the attachment of polyethylene glycol chains), have significantly enhanced their pharmacokinetic profiles by reducing recognition and clearance by the mononuclear phagocyte system, thereby prolonging systemic circulation [9].
Table 1: Key Characteristics of Liposome Structural Types
| Liposome Structure | Number of Bilayers | Typical Size Range | Key Features and Preferred Drug Encapsulation |
|---|---|---|---|
| Unilamellar Vesicles | Single | 50 – 250 nm | Prominent aqueous core; well-suited for hydrophilic drugs [9]. |
| Multilamellar Vesicles | Multiple, concentric | 1 – 5 μm | High lipid content; effective for entrapping lipophilic drugs [9]. |
| Oligolamellar Vesicles | A few | Varies | Intermediate structure [9]. |
Protocol: Preparation of Galloylated Liposomes for Targeted Drug Delivery
This protocol details the synthesis of galloylated liposomes (GA-lipo), a platform enabling stable, non-covalent adsorption of targeting ligands (e.g., antibodies) while preserving their functionality and overcoming the protein corona challenge [13].
1. Synthesis of Gallic Acid-Modified Lipid (GA-Chol):
- React gallic acid with cholesterol derivatives (e.g., using P0 linker) via a carbodiimide-mediated coupling reaction in anhydrous dimethylformamide (DMF) under an inert atmosphere for 24 hours [13].
- Purify the resulting GA-P0-Chol product using silica gel column chromatography and confirm structure via NMR and mass spectrometry [13].
2. Formation of GA-lipo by Thin-Film Hydration and Extrusion:
- Prepare a lipid mixture in chloroform with a molar composition of HSPC:Cholesterol:GA-P0-Chol = 60:30:10 [13].
- Form a thin lipid film by rotary evaporation under reduced pressure at 40°C.
- Hydrate the film with an appropriate aqueous buffer (e.g., phosphate-buffered saline, pH 7.4) to form multilamellar vesicles.
- Size the liposomes by sequentially extruding the suspension through polycarbonate membranes (e.g., 400 nm, 200 nm, and finally 100 nm) at a temperature above the lipid phase transition temperature.
3. Remote Loading of Drug (e.g., Doxorubicin derivative, DXdd):
- Establish a transmembrane gradient (e.g., ammonium sulfate) to drive the active loading of weakly basic drugs into the liposomal aqueous core [13].
- Incubate the drug with the pre-formed, extruded GA-lipo for a specified duration and temperature to achieve high encapsulation efficiency (protocol achieved ~95%) [13].
4. Functionalization with Targeting Ligand (e.g., Trastuzumab):
- Incubate the drug-loaded GA-lipo with the purified antibody (e.g., Trastuzumab) at a molar ratio of approximately 0.025% (protein:lipids) [13].
- Allow adsorption to proceed at 25°C for 1 hour with gentle agitation. The galloyl moieties on the liposome surface will stably adsorb the protein [13].
- Purify the resulting immunoliposomes (Trastuzumab@GA-lipo) from unbound antibody using size exclusion chromatography [13].
Diagram 1: Workflow for preparing targeted galloylated liposomes.
The Researcher's Toolkit: Key Reagents for Liposome Formulation
| Reagent / Material | Function / Application |
|---|---|
| Hydrogenated Soy Phosphatidylcholine (HSPC) | A high-transition-temperature phospholipid providing structural integrity to the liposomal bilayer [13]. |
| Cholesterol | Incorporated into the lipid bilayer to enhance membrane stability and reduce fluidity, decreasing drug leakage [9] [13]. |
| GA-P0-Chol (Gallic Acid-modified Cholesterol) | Enables stable, non-covalent adsorption of protein-based targeting ligands (e.g., antibodies) onto the liposome surface [13]. |
| Polyethylene Glycol (PEG)-Lipid Conjugate | Used to create "stealth" liposomes by forming a hydrophilic corona that reduces opsonization and extends circulation half-life [9]. |
| Ammonium Sulfate Buffer | Used to create a transmembrane pH gradient for the active remote loading of weakly basic drugs into the liposomal core [13]. |
Lipid Nanoparticles (LNPs)
Application Notes
LNPs represent a significant breakthrough in the delivery of nucleic acids (RNA, DNA), enabling gene therapy, vaccine delivery, and personalized medicine [10] [14]. Their effectiveness is highly dependent on optimization for specific routes of administration, which significantly influences organ distribution, expression kinetics, and therapeutic outcomes [10]. Recent advances include tailoring PEGylated lipids to impact mRNA delivery efficiency and stability, incorporating anti-inflammatory lipids to mitigate immune responses, and engineering LNPs capable of traversing the blood-brain barrier for neurological applications [14] [15].
Protocol: Formulation of Brain-Targeting mRNA LNPs
This protocol outlines the engineering and preparation of LNPs for intravenous delivery of mRNA across the blood-brain barrier [14].
1. LNP Lipid Composition Preparation:
- Prepare an ethanol phase containing a ionizable cationic lipid, phospholipid, cholesterol, and a PEGylated lipid at a defined molar ratio. The specific ionizable lipid and PEG-lipid structure are critical for brain targeting and must be optimized [14].
- Prepare an aqueous phase containing the mRNA of interest in a citrate buffer (pH 4.0).
2. Microfluidic Mixing for Nanoparticle Formation:
- Use a microfluidic device (e.g., a staggered herringbone mixer or a comparable chip-based system) to facilitate rapid mixing.
- Set the flow rate ratio (aqueous:ethanol) typically between 3:1 and 5:1 to ensure efficient nanoprecipitation and high mRNA encapsulation efficiency.
- Maintain total flow rates that induce sufficient turbulent mixing to form particles with a size of 60-150 nm, which is suitable for the intended application.
3. Buffer Exchange and Dialysis:
- Collect the LNP formulation and immediately dilute it in a large volume of PBS (pH 7.4) to dilute the ethanol and prevent destabilization.
- Dialyze the resulting suspension against a large volume of PBS (pH 7.4) for 18-24 hours at 4°C to remove residual ethanol and establish a neutral pH.
4. Characterization and Validation:
- Particle Size and PDI: Measure by Dynamic Light Scattering (DLS). Target a polydispersity index (PDI) < 0.2.
- Encapsulation Efficiency: Quantify using a Ribogreen assay. Compare fluorescence with and without a detergent to distinguish encapsulated from free mRNA.
- In Vivo Validation: Administer LNPs intravenously to mice and assess functional protein expression in brain tissues (neurons and glial cells) via immunohistochemistry or Western blot [14].
Diagram 2: LNP formulation via microfluidic mixing.
The Researcher's Toolkit: Key Reagents for LNP Formulation
| Reagent / Material | Function / Application |
|---|---|
| Ionizable Cationic Lipid | Critical for mRNA encapsulation and endosomal escape; its pKa determines efficiency and tolerability [14] [15]. |
| PEGylated Lipid | Modulates LNP size, surface properties, and pharmacokinetics; reduces particle aggregation and improves stability [14]. |
| Nitro-oleic acid (NOA) | An anti-inflammatory lipid that can be incorporated to inhibit the cGAS-STING pathway, reducing inflammation from plasmid DNA delivery [14] [15]. |
| DSPC (Phospholipid) | A structural lipid that contributes to the formation and stability of the LNP bilayer [14]. |
| Microfluidic Mixer | Essential equipment for the reproducible and scalable production of LNPs with narrow size distribution [15]. |
Polymeric Nanoparticles
Application Notes
Polymeric nanoparticles (PNPs) offer superior stability and versatility for the controlled delivery of a wide range of therapeutics, including biologics [11] [16] [17]. Their nanoscale dimensions facilitate targeted cellular uptake and navigation of biological barriers. A key advantage is the ability to engineer "smart" polymers that respond to specific physiological stimuli (e.g., pH, temperature, enzymes), enabling precise drug release at the target site [17]. Surface modification techniques, such as PEGylation and the incorporation of active targeting ligands (antibodies, peptides), further enhance targeting efficiency and penetration into target tissues [17].
Protocol: Preparation of Stimuli-Responsive Polymeric Nanoparticles
This protocol describes the formulation of PNPs using the nano-precipitation method, with a focus on creating particles capable of releasing their payload in response to the acidic tumor microenvironment [17].
1. Polymer and Drug Solution Preparation:
- Select a biodegradable, pH-sensitive polymer (e.g., poly(lactic-co-glycolic acid) with acid-labile side chains or a poly(β-amino ester)).
- Dissolve the polymer and a hydrophobic model drug (e.g., Docetaxel) in a water-miscible organic solvent such as acetone or acetonitrile.
2. Nano-precipitation and Self-Assembly:
- Add the organic solution drop-wise into a stirred aqueous phase (e.g., deionized water or a surfactant solution like polysorbate 80) under constant magnetic stirring.
- The rapid diffusion of the organic solvent into the water phase causes the polymer to precipitate, entrapping the drug and forming nanoparticles.
- Continue stirring for 3-4 hours to allow for complete solvent evaporation.
3. Surface Functionalization for Active Targeting:
- For active targeting, conjugate a targeting ligand (e.g., a folate moiety or an RGD peptide) to the surface of the pre-formed nanoparticles.
- This can be achieved via carbodiimide chemistry, where surface carboxyl groups on the PNPs are activated with EDC/NHS before reacting with primary amine groups on the ligand.
4. Purification and Characterization:
- Purify the PNPs by ultracentrifugation (e.g., at 40,000 rpm for 30 minutes) and resuspend the pellet in PBS.
- Particle Size and Zeta Potential: Characterize using DLS and laser Doppler anemometry.
- Drug Loading and Encapsulation Efficiency: Determine by HPLC after dissolving a known amount of PNPs in organic solvent.
- In Vitro Release Kinetics: Perform a dialysis-based release study in buffers at pH 7.4 and 5.5 to validate the pH-responsive release profile.
Diagram 3: Workflow for preparing stimuli-responsive polymeric nanoparticles.
The Researcher's Toolkit: Key Reagents for PNP Formulation
| Reagent / Material | Function / Application |
|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable and FDA-approved copolymer widely used for sustained and controlled drug release [17]. |
| EDC and NHS | Crosslinking agents used in carbodiimide chemistry to activate carboxyl groups for covalent conjugation of targeting ligands to the nanoparticle surface [17]. |
| Folate or RGD Peptide | Targeting ligands that can be conjugated to PNPs to promote active targeting to folate receptor-overexpressing cancers or integrins in the tumor vasculature, respectively [17]. |
| Polysorbate 80 | A surfactant used in the nano-precipitation process to stabilize the formed nanoparticles and prevent aggregation [17]. |
Comparative Analysis
Table 2: Comparative Overview of Core Nanoparticle Platforms for Drug Delivery
| Parameter | Liposomes | Lipid Nanoparticles (LNPs) | Polymeric Nanoparticles (PNPs) |
|---|---|---|---|
| Primary Composition | Phospholipids, Cholesterol [9] | Ionizable Lipids, Phospholipid, Cholesterol, PEG-lipid [14] | Biodegradable Polymers (e.g., PLGA, Chitosan) [17] |
| Typical Load Cargo | Hydrophilic & Hydrophobic small molecules [9] | Nucleic Acids (mRNA, pDNA, CRISPR) [10] [14] | Small molecules, Proteins, Peptides, Biologics [16] [17] |
| Key Advantage | High biocompatibility, Established clinical use [9] [12] | High efficiency for nucleic acid delivery, Rapidly advancing platform [10] [14] | Superior stability, Controlled & stimuli-responsive release [11] [17] |
| Common Preparation Method | Thin-Film Hydration & Extrusion [12] [13] | Microfluidic Mixing [15] | Nano-precipitation, Emulsion-Solvent Evaporation [17] |
| Targeting Strategy | Passive (EPR), Ligand adsorption/conjugation [9] [13] | Tissue-specific lipid selection, Ligand functionalization [14] [15] | Surface PEGylation, Stimuli-responsive polymers, Ligand conjugation [17] |
Application Notes
The application of nanotechnology in targeted drug delivery is revolutionizing the treatment of complex diseases by enhancing drug solubility, enabling targeted delivery, and improving therapeutic efficacy. Dendrimers, metallic nanoparticles, and drug nanocrystals represent three prominent classes of nanocarriers with distinct advantages for pharmaceutical development.
Dendrimers in Targeted Drug Delivery
Dendrimers are highly branched, monodisperse, tree-like polymeric molecules with three main architectural components: a central core, branching units, and functional surface end groups. Their nanoscopic size (typically 1-15 nm), nearly spherical shape, and highly tunable surface chemistry make them exceptional candidates for drug delivery [18] [19] [20].
Table 1: Key Characteristics and Biomedical Applications of Dendrimers
| Characteristic | Description | Application Impact |
|---|---|---|
| Structure | Three-dimensional, globular, with internal cavities [18] | Allows for encapsulation of hydrophobic drugs and genes [19] |
| Surface Functionalization | High density of tunable terminal groups [20] | Enables conjugation of drugs, targeting ligands (e.g., folates, peptides), and PEG for stealth properties [19] [21] |
| Monodispersity | Uniform size and molecular weight within each generation [19] | Provides predictable pharmacokinetics and reproducible behavior [19] |
| Enhanced Permeability and Retention (EPR) | Nanoscale size and long circulation [19] | Facilitates passive targeting and accumulation in tumor tissues [18] [21] |
| Cationic Surface | Positive charge on amine-terminated dendrimers (e.g., PAMAM) [19] | Allows for complexation with nucleic acids (DNA, siRNA) for gene delivery [19] [21] |
Dendrimers have shown significant promise in oncology. They can deliver chemotherapeutic agents like doxorubicin, methotrexate, and paclitaxel, enhancing water solubility and enabling controlled, stimuli-responsive release in the tumor microenvironment via pH-sensitive or redox-sensitive linkers [18] [19]. In neurodegenerative diseases such as Alzheimer's and Parkinson's, dendrimers can cross the blood-brain barrier (BBB), delivering therapeutic agents to target amyloid-beta plaques and neurofibrillary tangles [22] [23]. Furthermore, their application as antimicrobial and antiviral agents is being explored, with studies demonstrating efficacy against respiratory viruses, HIV, and herpes simplex virus, and more recently, in strategies against COVID-19 [18].
Metallic Nanoparticles as Nanocarriers
Metallic nanoparticles (MNPs), including those made from gold, silver, platinum, and zinc oxide, offer unique mechanical, electromagnetic, and optical properties for drug delivery [24] [25]. Their primary advantages include increased stability and half-life of drug carriers in circulation, required biodistribution, and passive or active targeting to specific sites [25].
Table 2: Applications of Selected Metallic Nanoparticles (MNPs)
| Metal Nanoparticle | Key Properties | Exemplary Drug Delivery Applications |
|---|---|---|
| Gold (Au) | Biocompatibility, tunable surface plasmon resonance, easy functionalization [25] | Photothermal therapy, targeted delivery of anticancer drugs [25] |
| Silver (Ag) | Intrinsic antimicrobial activity [25] | Delivery of antibiotics to treat bone infections; combating multidrug-resistant bacteria [25] |
| Zinc Oxide (ZnO) | Semiconductor properties, ROS generation [25] | Cancer therapy, drug delivery systems [25] |
A significant trend in MNP synthesis is the move toward green synthesis methods, which use biological organisms (e.g., plant extracts, microbes) as reducing and stabilizing agents. This approach provides economic and environmental benefits compared to traditional chemical and physical methods [24] [25].
Drug Nanocrystals for Bioavailability Enhancement
Drug nanocrystals are pure crystalline drug particles with a size in the nanometer range. They represent a versatile platform to overcome the primary challenge of poor water solubility for many new chemical entities [26].
Table 3: Advantages and Applications of Drug Nanocrystals
| Advantage | Mechanism | Therapeutic Outcome |
|---|---|---|
| Enhanced Dissolution Rate | Increased surface area-to-volume ratio [26] | Improved saturation solubility and faster dissolution velocity [26] |
| Improved Bioavailability | Higher dissolution leads to greater absorption [26] | Increased drug concentration in systemic circulation; improved treatment effectiveness [26] |
| Versatile Delivery Platforms | Can be administered via oral, pulmonary, or injectable routes [26] | Broad application across disease areas [26] |
| Surface Functionalization | Coating with ligands for active targeting [26] | Enables targeted delivery, particularly in cancer therapy [26] |
Surface engineering of drug nanocrystals is critical for stabilizing the particles and functionalizing them with targeting ligands, transforming them from simple solubility enhancers into sophisticated targeted delivery systems [26].
Experimental Protocols
Protocol: Synthesis and Drug Loading of PAMAM Dendrimers
This protocol describes the divergent synthesis of a Generation 4 (G4) PAMAM dendrimer and its subsequent loading with an anticancer drug (e.g., Doxorubicin) via a pH-sensitive hydrazone bond [19] [20] [21].
Research Reagent Solutions:
| Reagent/Material | Function/Explanation |
|---|---|
| Ethylenediamine (EDA) Core | Serves as the central initiator core for PAMAM dendrimer growth [20] |
| Methyl Acrylate | Reacts with amine groups via Michael addition to create ester-terminated intermediates [19] [21] |
| Ethylenediamine (EDA) (excess) | Used in the amidation step to convert ester terminals to amine terminals, creating a new generation [19] [21] |
| Methanol | Acts as a solvent for the synthesis reactions [19] |
| Doxorubicin HCl | Model chemotherapeutic drug to be conjugated to the dendrimer [18] [21] |
| Hydrazine Hydrate | Provides the hydrazone linker, which is stable at physiological pH (7.4) but cleaves in the acidic tumor microenvironment (pH ~5-6) [19] |
Procedure:
- Divergent Synthesis of G4 PAMAM Dendrimer:
- Michael Addition (Generation 0.5): Add a large excess of methyl acrylate to the ethylenediamine core in methanol. React under inert atmosphere (N₂) with stirring for 24-48 hours at room temperature. Remove excess methyl acrylate and solvent via vacuum distillation to obtain a half-generation (G0.5) ester-terminated dendrimer [19] [21].
- Amidation (Generation 1.0): Dissolve the G0.5 product in a large excess of ethylenediamine in methanol. React with stirring for 24-48 hours at room temperature. Remove excess EDA and solvent via vacuum distillation to obtain a full-generation (G1.0) amine-terminated dendrimer [19] [21].
- Repetition: Repeat steps a and b three more times to sequentially build Generations 2.0, 3.0, and the target 4.0 (G4) PAMAM dendrimer.
- Purification: Purify the final G4 dendrimer product using dialysis or ultrafiltration. Confirm structure and monodispersity using techniques such as NMR spectroscopy and gel permeation chromatography (GPC) [19].
- Drug Conjugation via pH-Sensitive Linker:
- Activation: React the G4 PAMAM dendrimer with hydrazine hydrate to create hydrazide-terminated groups on the dendrimer surface.
- Conjugation: React the hydrazide-activated dendrimer with doxorubicin in an organic solvent (e.g., DMSO) under inert conditions. The carbonyl group of doxorubicin reacts with the hydrazide to form a pH-sensitive hydrazone bond.
- Purification and Characterization: Purify the final dendrimer-doxorubicin conjugate (Den-Dox) using dialysis. Characterize the conjugate using UV-Vis spectroscopy to determine the drug loading efficiency and dynamic light scattering (DLS) to measure the hydrodynamic size and zeta potential [19] [21].
Protocol: Preparation of Targeted Drug Nanocrystals
This protocol outlines the preparation of drug nanocrystals of a poorly water-soluble drug (e.g., Rapamycin) using anti-solvent precipitation, followed by surface stabilization and functionalization with a targeting ligand (e.g., Folic Acid) for cancer therapy [26].
Research Reagent Solutions:
| Reagent/Material | Function/Explanation |
|---|---|
| Rapamycin | A model poorly water-soluble drug (BCS Class II) with immunosuppressant and anticancer properties. |
| Acetone | A water-miscible organic solvent (good solvent) to dissolve the drug. |
| Poloxamer 407 (Pluronic F127) | A polymeric stabilizer that adsorbs to the nanocrystal surface to prevent aggregation via steric hindrance [26]. |
| DSPE-PEG(2000)-Folate | A phospholipid-PEG conjugate terminated with folic acid. Serves as a co-stabilizer and targeting ligand for cancer cells overexpressing folate receptors [26]. |
| Deionized Water | Acts as the anti-solvent in which the drug has very low solubility. |
Procedure:
- Anti-Solvent Precipitation:
- Drug Solution: Dissolve rapamycin and DSPE-PEG(2000)-Folate in acetone to create an organic phase.
- Aqueous Stabilizer Solution: Dissolve Poloxamer 407 in deionized water to create the aqueous phase.
- Precipitation: Under high-speed homogenization or sonication, rapidly inject the organic drug solution into the aqueous stabilizer solution. The rapid mixing causes immediate supersaturation and precipitation of the drug into nanocrystals. The stabilizers (Poloxamer and DSPE-PEG-Folate) instantly adsorb onto the newly formed crystal surfaces.
- Stabilization and Functionalization:
- The nanocrystal suspension is continuously stirred for several hours to allow for complete stabilizer adsorption and evaporation of the organic solvent.
- The simultaneous presence of DSPE-PEG-Folate during precipitation leads to its incorporation into the stabilizer shell, functionally targeting the nanocrystals.
- Purification and Analysis:
- Purify the nanocrystal suspension by centrifugation or ultrafiltration to remove any non-incorporated drug and free stabilizers.
- Characterize the final product using Dynamic Light Scattering (DLS) for particle size and polydispersity index (PDI), and Scanning Electron Microscopy (SEM) for morphological analysis. Confirm surface functionalization via X-ray Photoelectron Spectroscopy (XPS) or a similar surface analysis technique [26].
Visualizations
Dendrimer Drug Delivery and Release Pathway
Nanocrystal Preparation Workflow
The Enhanced Permeability and Retention (EPR) effect is a universal pathophysiological phenomenon observed in solid tumors, serving as a fundamental principle for the passive targeting of macromolecular drugs and nanomedicines [27]. First described by Hiroshi Maeda and colleagues in 1986, the EPR effect leverages the unique anatomical and physiological abnormalities of tumor vasculature to achieve selective accumulation of therapeutic agents in tumor tissue [27] [28]. This targeting mechanism has become a cornerstone concept in oncology nanomedicine, enabling the design of drug delivery systems that theoretically increase therapeutic efficacy while reducing systemic toxicity.
The EPR effect arises from two key pathological features of solid tumors. First, tumor blood vessels exhibit enhanced permeability due to poorly aligned endothelial cells with wide fenestrations, deficient basement membranes, and reduced pericyte coverage [27] [29]. These structural abnormalities create gaps ranging from 100 to 780 nm in diameter, allowing macromolecules and nanoparticles to extravasate from the bloodstream into tumor tissue [30]. Second, tumors display impaired lymphatic drainage, which limits the clearance of these extravasated molecules, leading to their prolonged retention in the tumor interstitium [27] [28]. This combination of leaky vasculature and poor drainage enables the passive accumulation of nanomedicines in solid tumors.
Table 1: Pathophysiological Characteristics Underpinning the EPR Effect
| Characteristic | Description | Impact on EPR Effect |
|---|---|---|
| Abnormal Tumor Vasculature | Dilated, tortuous vessels with defective endothelial cells, wide fenestrations, and deficient smooth muscle layers [27] [29] | Enables extravasation of macromolecules and nanoparticles into tumor tissue |
| Vascular Hyperpermeability | Gaps between endothelial cells (100-780 nm) and transcellular pathways via vesiculo-vacuolar organelles (VVOs) [27] [30] | Facilitates passive accumulation of nanomedicines in tumor interstitium |
| Lack of Lymphatic Drainage | Impaired or absent lymphatic systems in solid tumor tissue [27] [28] | Prolongs retention of extravasated macromolecules and nanoparticles |
| Inflammatory Mediators | Elevated expression of bradykinin, nitric oxide, prostaglandins, VEGF, and other permeability factors [27] [30] | Sustains and enhances vascular permeability in tumor tissue |
The EPR effect is further sustained by various inflammatory factors and mediators present in the tumor microenvironment, including prostaglandins, bradykinin, nitric oxide, peroxynitrite, and vascular endothelial growth factor (VEGF) [27] [30]. These factors coordinate to maintain the hyperpermeability of tumor vessels, thereby enhancing the EPR effect. The phenomenon has been consistently observed in rodent models, rabbits, canines, and human patients, although with significant heterogeneity in its intensity and effectiveness [27].
Quantitative Analysis of EPR Efficacy
Understanding the quantitative aspects of the EPR effect is crucial for evaluating its therapeutic potential and limitations. While the EPR effect does enhance tumor accumulation of nanomedicines compared to normal tissues, the actual delivery efficiency is often modest. Studies indicate that the EPR effect typically provides less than a 2-fold increase in nano-drug delivery to tumors compared with critical normal organs [29]. This modest enhancement frequently results in drug concentrations that are insufficient for curing most cancers, highlighting a significant challenge in clinical translation.
The percentage of the total administered nanoparticle dose that successfully reaches solid tumors is remarkably low, with a median of only 0.7% accumulating in the target tissue [28]. This low accumulation efficiency is attributed to multiple biological barriers, including rapid clearance by the mononuclear phagocyte system, elevated interstitial fluid pressure in tumors, and heterogeneous tumor blood flow [29]. Despite these limitations, the EPR effect remains clinically relevant as it still enables significantly higher tumor concentrations compared to conventional chemotherapeutic agents, often with reduced side effects due to lower accumulation in healthy tissues.
Table 2: Quantitative Parameters of Nanoparticle Delivery via EPR Effect
| Parameter | Typical Value/Range | Clinical Implications |
|---|---|---|
| Tumor Accumulation Efficiency | Median of 0.7% of injected dose [28] | Low delivery efficiency necessitates high initial dosing or complementary strategies |
| Enhanced Delivery Ratio | Less than 2-fold increase compared to normal organs [29] | Modest targeting effect may be insufficient for curative monotherapies |
| Optimal Size Threshold | >40 kDa molecular weight [27] | Guides design of macromolecular drugs and nanocarriers for EPR-based targeting |
| Vascular Pore Size | 100-780 nm in tumor vasculature [30] | Informs nanoparticle size optimization for extravasation |
| Pegylated Liposomal Doxorubicin Tumor Concentration | 10-15 fold higher in tumor vs. normal tissues [27] | Demonstrates clinical proof-of-concept for EPR-mediated targeting |
The size and physicochemical properties of nanomedicines significantly influence their EPR-mediated tumor accumulation. The molecular size threshold for effective EPR-mediated accumulation is approximately 40 kDa, with larger macromolecules and nanoparticles exhibiting more pronounced tumor retention [27]. Nanoparticle characteristics such as size, surface charge, and spatial configuration are crucial determinants of their circulation half-life, extravasation potential, and tumor retention [27]. For instance, pegylated liposomal doxorubicin achieves about a 10-15 fold higher concentration in tumor tissues compared with surrounding normal tissues, demonstrating the clinical viability of the EPR effect despite its limitations [27].
Experimental Protocols for EPR Evaluation
MRI-Based Quantification of EPR Effect
Objective: To non-invasively quantify the EPR effect in tumor models using dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) with a nano-sized contrast agent [31].
Materials:
- GadoSpin P: A 200 kDa biodegradable polymeric gadolinium-based MRI contrast agent (25 mM concentration after reconstitution) [31]
- Animal Models: Mice with subcutaneously implanted xenograft tumors (e.g., SKOV-3, OVCAR-8, or OVASC-1 ovarian cancer cell lines) [31]
- MRI System: 1.0-tesla ASPECT M2 MRI System with a 35 mm Tx/Rx mouse solenoid whole-body coil [31]
- Anesthesia Equipment: Isoflurane/oxygen delivery system for animal anesthesia [31]
Procedure:
- Animal Preparation: Anesthetize tumor-bearing mice using 4-5% isoflurane/oxygen mixture, maintained with 1-2% isoflurane during scanning [31].
- Pre-contrast Imaging: Position tumor within MRI system using Scout mode scan. Acquire T2-weighted fast spin echo (FSE) sequence for anatomical reference with the following parameters: coronal direction, field of view (FOV) 100 mm × 100 mm, 20 slices, slice thickness 1 mm, flip angle 90 degrees, sampling 256 [31].
- Contrast Administration: Inject 100 μL of reconstituted GadoSpin P solution retro-orbitally at a dosage of 25 μL per gram of mouse body weight [31].
- DCE-MRI Acquisition: Perform dynamic T1-weighted MRI scans pre- and post-contrast injection using a quantitative varied flip-angle (VFA) approach to measure contrast agent concentration kinetics [31].
- Data Analysis: Apply Tofts pharmacokinetic modeling to calculate:
- Parametric Mapping: Generate maps of gadolinium concentration in tumor tissue to visualize spatial heterogeneity of EPR effect [31].
Data Interpretation: Higher Ktrans and Ve values indicate stronger EPR effect. Significant differences in these parameters have been observed among different tumor models, with tumor growth influencing both permeability and retention [31].
Evaluation of Nanoparticle Extravasation and Retention
Objective: To assess the extravasation and retention kinetics of nanoparticles in tumor tissue using intravital microscopy [32].
Materials:
- Fluorescently Labeled Nanoparticles: Various formulations (liposomes, polymeric nanoparticles, etc.) with appropriate fluorophores [32]
- Animal Models: Mice with window chamber tumors or other models suitable for intravital imaging [32]
- Intravital Microscopy System: High-resolution fluorescence microscope with capabilities for in vivo time-lapse imaging [32]
- Image Analysis Software: For quantifying fluorescence intensity and spatial distribution over time [32]
Procedure:
- Nanoparticle Administration: Intravenously inject fluorescent nanoparticles into tumor-bearing animals at therapeutically relevant doses [32].
- Real-time Imaging: Perform time-lapse intravital microscopy at multiple time points post-injection (e.g., 1, 4, 24, 48 hours) to track nanoparticle distribution [32].
- Multi-scale Analysis: Quantify nanoparticles at different biological scales:
- Barrier Assessment: Evaluate alternative pathways beyond passive extravasation, including:
- Kinetic Modeling: Calculate accumulation rates and retention half-lives of nanoparticles in different tumor compartments [32].
Data Interpretation: This protocol enables the differentiation between vascular permeability and cellular uptake, providing insights into both EPR effect and active transport mechanisms that contribute to tumor accumulation of nanomedicines [32].
Figure 1: Nanoparticle Journey via EPR Effect. This workflow illustrates the pathway of nano-sized drugs from administration to tumor accumulation and clearance, highlighting key biological processes that enable passive targeting.
Strategies to Enhance EPR-Based Drug Delivery
Nanocarrier Design Optimization
The design of nanocarriers significantly influences their ability to leverage the EPR effect for tumor targeting. Key parameters include:
Size Optimization: Studies using serial molecular sizes of HPMA copolymers in solid tumor animal models have identified optimal size ranges for tumor accumulation [27]. Nanoparticles between 10-100 nm typically exhibit the most favorable balance between circulation time and extravasation potential, with smaller particles (<20 nm) showing improved penetration but potentially faster clearance [27] [29].
Surface Modification: Polyethylene glycol (PEG) conjugation (PEGylation) prolongs circulation time by reducing opsonization and recognition by the mononuclear phagocyte system [33] [30]. However, excessive PEGylation can compromise cytotoxicity, as demonstrated by pegylated liposomal doxorubicin which showed significantly reduced cytotoxicity compared to free drug (25% vs. 75% at 72 hours) [27].
Material Composition: Different nanocarrier materials offer distinct advantages:
- Lipid nanoparticles (liposomes, SLNs, NLCs) enhance drug bioavailability and can bypass multidrug resistance mechanisms [30] [6]
- Polymeric nanoparticles (PEG, PLGA, PAMAM) enable controlled drug release and high drug loading capacity [30]
- Inorganic nanoparticles (gold, silver, iron oxide) provide additional functionalities for imaging and therapy [30]
- Hybrid nanoparticles combine multiple materials to create theranostic systems with both diagnostic and therapeutic capabilities [30]
Table 3: Nanocarrier Types and Their Applications in EPR-Based Drug Delivery
| Nanocarrier Type | Key Characteristics | Applications in Cancer Therapy |
|---|---|---|
| Liposomes | Phospholipid bilayers encapsulating hydrophilic drugs, modifiable size and surface | Doxil/Caelyx (pegylated liposomal doxorubicin) for various cancers [27] [6] |
| Polymeric Nanoparticles | Biodegradable polymers (PLGA, chitosan) enabling sustained release | Paclitaxel-loaded nanoparticles for localized, prolonged action [30] |
| Solid Lipid Nanoparticles (SLNs) | Lipid matrix solid at room temperature, improved stability | Co-delivery of doxorubicin and curcumin to enhance cytotoxicity [30] |
| Dendrimers | Highly branched, monodisperse structures with multiple surface groups | PAMAM dendrimers for optimized targeted therapy with high drug loading [30] |
| Inorganic Nanoparticles | Unique optical, magnetic, electronic properties | Gold nanoparticles for thermal ablation; iron oxide for MRI and therapy [30] |
| Hybrid Nanoparticles | Combination of organic/inorganic materials for multifunctionality | AGuIX nanoparticles for radiotherapy enhancement and imaging [30] |
EPR Enhancement Through Tumor Microenvironment Modulation
Several strategies have been developed to enhance the EPR effect by modifying the tumor microenvironment:
Vascular Normalization: Anti-VEGF therapies can temporarily "normalize" the abnormal tumor vasculature, reducing hyperpermeability and improving perfusion [27]. This approach increases the uptake of small particles (<20 nm) but may hinder the extravasation of larger particles (>125 nm) [27]. The timing of nanomedicine administration relative to vascular normalization is critical for optimal delivery [27].
Physical Priming Methods:
- Hyperthermia: Mild heating of tumors increases blood flow and vascular permeability, enhancing nanoparticle extravasation [27] [34]
- Sonoporation: Ultrasound, particularly in combination with microbubbles, mechanically untightens vessel walls and the extracellular matrix [34]
- Radiation therapy: Can modify tumor vasculature and increase permeability to nanomedicines [34]
Pharmacological Approaches:
- Angiogenic factors to increase vascular maturity [34]
- Erythropoietin to improve tumor perfusion [34]
- Corticosteroids to remodel vessels and extracellular matrix [34]
- Enzymes such as collagenase or hyaluronidase to degrade dense extracellular matrix and reduce interstitial fluid pressure [30]
Figure 2: Multimodal Strategies to Overcome EPR Limitations. This diagram outlines the four primary approaches to enhance drug delivery efficacy by addressing the inherent limitations of the EPR effect through complementary strategies.
Patient Stratification and Companion Diagnostics
The significant heterogeneity in EPR effect among different tumors and patients necessitates advanced stratification approaches:
Imaging Biomarkers: Quantitative MRI-based approaches, as described in Protocol 3.1, can assess EPR efficacy in individual patients before treatment [31]. Tumors showing sufficient EPR levels can be selected for nanomedicine therapies, while those with poor EPR can be directed to alternative treatments [31] [34].
Histological and Omics Biomarkers: Analysis of tumor specimens for vascular density, pericyte coverage, extracellular matrix composition, and expression of permeability factors can predict EPR efficacy [34].
Companion Diagnostics and Theranostics: The development of nanomedicines with built-in imaging capabilities allows simultaneous diagnosis and treatment, enabling real-time monitoring of drug delivery and accumulation [34].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for EPR Effect Studies
| Reagent/Category | Function/Application | Examples/Specifications |
|---|---|---|
| Nanoparticle Contrast Agents | Enable visualization and quantification of EPR effect using medical imaging | GadoSpin P (200 kDa biodegradable polymeric gadolinium for MRI) [31] |
| Fluorescent Nanoparticles | Permit tracking of nanoparticle distribution using intravital microscopy | Liposomes, polymeric NPs with Cy5.5, DiD, or other fluorophores [32] |
| Tumor Model Systems | Provide biologically relevant platforms for EPR evaluation | Xenograft models (SKOV-3, OVCAR-8, OVASC-1 cell lines) [31] |
| Vascular Permeability Modulators | Experimental manipulation of EPR effect | VEGF inhibitors, bradykinin agonists, nitric oxide donors [27] [34] |
| Lymphatic Function Assays | Assessment of lymphatic drainage impairment in tumors | Fluorescent dextran drainage assays, lymphatic marker staining [27] [30] |
| Image Analysis Software | Quantification of nanoparticle accumulation and distribution | Tofts pharmacokinetic modeling for DCE-MRI data [31] |
The EPR effect remains a fundamental principle in cancer nanomedicine, providing a rational basis for the passive targeting of solid tumors. While clinical translation has been challenged by the effect's heterogeneity and modest delivery efficiency, recent advances in nanocarrier design, tumor microenvironment modulation, and patient stratification offer promising pathways to enhance therapeutic outcomes. The experimental protocols and reagents outlined in this application note provide researchers with robust methodologies to evaluate and optimize EPR-based drug delivery systems. As the field progresses toward personalized nanomedicine, the integration of quantitative EPR assessment with multifunctional nanocarriers and complementary delivery strategies will be essential to fully realize the potential of this cornerstone targeting mechanism in oncology.
In the pursuit of advanced targeted drug delivery systems, nanotechnology provides powerful solutions to three fundamental pharmaceutical challenges: poor solubility, low bioavailability, and short circulation half-life of active therapeutic compounds [35] [36]. By engineering materials at the nanoscale (typically 1-100 nm), researchers can create carriers that fundamentally reshape drug pharmacokinetics and biodistribution [1] [33]. These nanocarriers protect therapeutic agents from degradation, enhance their aqueous solubility, and facilitate targeted delivery to specific tissues while minimizing off-target effects [35] [37]. This document outlines the key advantages, quantitative benchmarks, and experimental protocols for leveraging nanotechnology in pharmaceutical development, providing researchers with practical methodologies for evaluating and optimizing nanocarrier systems.
Quantitative Advantages of Nanocarrier Systems
Nanocarriers significantly enhance drug performance by improving solubility, bioavailability, and circulation time. The tables below summarize key quantitative improvements achieved with various nanocarrier platforms.
Table 1: Solubility and Bioavailability Enhancement of Nano-Formulated Drugs
| Drug/Nanocarrier System | Solubility Enhancement | Bioavailability/ Efficacy Improvement | Reference Application |
|---|---|---|---|
| Paclitaxel in Ionic Co-aggregates (ICAs) | 10-fold solubility increase | Data Not Specified | Intravenous delivery of poorly soluble drug [35] |
| Ivermectin in Mesoporous Silica/Poly(ε-caprolactone) | Significant dissolution rate improvement | ~90% increased drug release (72h) vs. 40% for crystalline drug | Treatment of parasitic infections [35] |
| Polymeric Nanoparticles (General) | Data Not Specified | ~50% increase vs. conventional formulations | Colorectal cancer therapy [37] |
| Mitoxantrone in Carbon Quantum Dots (CQDs) | Data Not Specified | 97% drug loading efficiency; maximal cancer cell growth inhibition | Cancer therapy [35] |
Table 2: Circulation Half-Life Optimization for Gold Nanoparticles (AuNPs)
| AuNP Size | PEG Molecular Weight | Impact on Blood Circulation Half-Life |
|---|---|---|
| < 40 nm | ≥ 5 kDa | Optimal, synergistic effect for significantly prolonged circulation [38] |
| > 40 nm | ≥ 5 kDa | Moderate half-life extension [38] |
| Any size | ≤ 2 kDa | Minimal impact on prolonging circulation, irrespective of GNP size [38] |
Experimental Protocols for Key Evaluations
Protocol: Assessing Drug Solubility and Release Kinetics
This protocol evaluates the efficiency of nanocarriers in improving the solubility and release profile of poorly soluble drugs, using ivermectin as a model compound [35].
1. Key Research Reagent Solutions
- Mesoporous Silica Nanomaterials: Serve as a porous carrier for drug loading via adsorption.
- Poly(ε-caprolactone) Nanocapsules: Biodegradable polymeric shells for drug encapsulation.
- Dialysis Membranes (MWCO appropriate for drug): Allow separation of released drug from nanocarriers.
- Aqueous Buffer (e.g., PBS, pH 7.4): Simulates physiological conditions for release study.
2. Methodology 1. Nanocarrier Preparation and Drug Loading: Synthesize mesoporous silica nanomaterials and poly(ε-caprolactone) nanocapsules using established methods (e.g., sol-gel for silica, nano-precipitation for polymers). Load ivermectin into the nanocarriers. 2. Solubility Measurement: Dispense crystalline ivermectin and each nano-encapsulated ivermectin formulation into separate vessels containing the aqueous buffer. Agitate for a predetermined time. 3. Centrifugation/Filtration: Separate undissolved drug from the solution by centrifugation or filtration using a 0.1 µm filter. 4. Quantification: Analyze the concentration of dissolved ivermectin in the supernatant/filtrate using a validated analytical method such as High-Performance Liquid Chromatography (HPLC). 5. In Vitro Release Study: Place a known quantity of each drug formulation (crystalline, silica-loaded, nanocapsule-loaded) into a dialysis bag. Immerse the bag in a large volume of release buffer (sink condition). 6. Sampling: At fixed time intervals (e.g., 1, 2, 4, 8, 24, 48, 72 hours), withdraw aliquots from the external buffer. 7. Analysis: Quantify the amount of drug released in each sample using HPLC. Replenish the release medium to maintain sink conditions.
3. Data Analysis
- Plot cumulative drug release (%) versus time to generate release profiles.
- Calculate the enhancement factor by comparing the release percentage of nano-formulations versus the crystalline drug at specific time points (e.g., 72 hours).
Protocol: Optimizing Circulation Time via PEGylation
This protocol outlines a method to evaluate how nanoparticle size and polyethylene glycol (PEG) coating molecular weight synergistically impact blood circulation half-life, based on a meta-analysis of gold nanoparticle (GNP) studies [38].
1. Key Research Reagent Solutions
- Gold Nanoparticles (GNPs): Synthesized in a range of sizes (e.g., 2-100 nm) as a model platform.
- Methoxy-PEG-Thiol (mPEG-SH): Thiol-terminated PEG polymers of varying molecular weights (e.g., 0.2, 2, 5, 10, 20 kDa) for covalent surface coating.
- Animal Model (e.g., Mice): For in vivo pharmacokinetic studies.
2. Methodology 1. GNP Synthesis and Characterization: Synthesize GNPs of precise, monodisperse sizes (e.g., 20 nm, 40 nm, 60 nm, 80 nm) using methods like the Turkevich or Brust-Schiffrin synthesis. Characterize the size, shape, and surface charge (zeta potential) of the bare particles. 2. PEG Functionalization: Incubate each GNP size variant with a series of mPEG-SH ligands of different molecular weights. Purify the PEGylated GNPs to remove unbound PEG. 3. Characterization of Coated Particles: Re-measure the hydrodynamic diameter and zeta potential of the PEGylated GNPs to confirm successful coating. Use techniques like FTIR or NMR to verify PEG attachment. 4. In Vivo Pharmacokinetic Study: Administer the library of PEGylated GNPs intravenously to animal cohorts. Collect blood samples at multiple time points post-injection. 5. Sample Analysis: Quantify GNP concentration in blood samples using an appropriate technique, such as Inductively Coupled Plasma Mass Spectrometry (ICP-MS). 6. Pharmacokinetic Modeling: Plot blood concentration versus time for each formulation. Calculate the circulation half-life (t₁/₂) using non-compartmental analysis.
3. Data Analysis
- Use a statistical model (e.g., Generalized Additive Model) to analyze the interaction between GNP size and PEG MW on half-life.
- Identify the optimal parameter combination (e.g., sub-40 nm GNPs with ≥5 kDa PEG) for maximal circulation time.
Visualizing the Nanocarrier Journey and Design Logic
The following diagrams illustrate the in vivo journey of a long-circulating nanocarrier and the decision-making workflow for its design.
Diagram 1: In Vivo Journey of a Long-Circulating Nanocarrier. PEGylation shields the carrier from immune recognition, enabling prolonged circulation and accumulation at the target site via the Enhanced Permeability and Retention (EPR) effect or active targeting, followed by cellular uptake and drug release [38] [39].
Diagram 2: Nanocarrier Design and Evaluation Workflow. A strategic workflow for selecting nanocarrier engineering strategies based on specific therapeutic challenges, leading to synthesis, characterization, and biological evaluation [1] [35] [38].
The strategic application of nanotechnology in drug formulation directly addresses the critical pharmaceutical challenges of solubility, bioavailability, and circulation time. The data and protocols provided herein demonstrate that through rational design—such as selecting appropriate nanocarrier platforms, optimizing particle size, and implementing effective surface engineering like PEGylation—researchers can significantly enhance the therapeutic potential of drug candidates. As the field advances, the integration of these foundational principles with emerging technologies like AI-driven design and biomimetic coatings will further accelerate the development of sophisticated, targeted drug delivery systems, ultimately improving clinical outcomes across a spectrum of diseases.
Engineering Precision: Methodologies for Targeted Delivery and Controlled Release
Targeted drug delivery represents a cornerstone of modern nanomedicine, aiming to maximize therapeutic efficacy while minimizing off-target effects. The two principal strategies for achieving this specificity are passive and active targeting. Passive targeting relies on the inherent physicochemical properties of nanocarriers and the pathological characteristics of tissues, such as the Enhanced Permeability and Retention (EPR) effect in tumors. In contrast, active targeting involves the functionalization of nanocarriers with biological ligands designed to bind specifically to receptors overexpressed on target cells [40] [41]. This document, framed within a broader thesis on applying nanotechnology in targeted drug delivery systems research, provides detailed application notes and experimental protocols for leveraging these strategies. It is intended to serve as a practical guide for researchers, scientists, and drug development professionals working to design and evaluate novel targeted nanotherapeutics.
Core Principles and Key Differences
Understanding the distinct mechanisms of passive and active targeting is fundamental to designing an effective drug delivery system. The following table summarizes their core characteristics.
Table 1: Core Characteristics of Passive and Active Targeting Strategies
| Feature | Passive Targeting | Active Targeting |
|---|---|---|
| Fundamental Mechanism | Exploits the Enhanced Permeability and Retention (EPR) effect of pathological sites like tumors [40]. | Utilizes ligand-receptor interactions for specific cellular binding and internalization [41] [42]. |
| Basis of Specificity | Physiological/pathological features of the tissue (e.g., leaky vasculature, poor lymphatic drainage) [40]. | Molecular recognition between surface ligands and overexpressed cell receptors [43] [42]. |
| Role of Nanocarrier Design | Optimizing size (typically 20-200 nm), surface charge, and composition for long circulation and EPR-based accumulation [44]. | Decorating the nanocarrier surface with targeting ligands (antibodies, peptides, etc.) without compromising stability [41] [42]. |
| Primary Interaction | Non-specific accumulation in tissues with permeable vasculature. | Specific binding to target cells, often leading to receptor-mediated endocytosis [41]. |
| Main Challenge | High heterogeneity of the EPR effect between tumor types and patients [40]. | Potential for immune recognition and off-target ligand interactions, complicating in vivo efficacy [45]. |
The following diagram illustrates the sequential relationship and key mechanisms of these two targeting strategies within a tumor microenvironment.
Application Notes: Ligand Selection and Nanocarrier Design
The choice of ligand is critical for the success of an active targeting strategy. Ligands are selected based on their affinity for receptors that are highly and preferentially expressed on the target cell population.
Table 2: Common Ligands and Their Target Receptors in Oncology
| Ligand Class | Specific Example | Target Receptor | Key Considerations |
|---|---|---|---|
| Peptides | Linear or Cyclic RGD (Arg-Gly-Asp) [45] [42] | αvβ3 Integrin | Overexpressed on tumor endothelial and cancer cells; promotes angiogenesis [45]. |
| Antibodies | Bevacizumab (BVZ) fragment [41] [43] | Vascular Endothelial Growth Factor (VEGF) | Targets tumor vasculature; full antibodies can be immunogenic, fragments are often preferred [43]. |
| Small Molecules | Folic Acid (Folates) [41] [42] | Folate Receptor | Highly overexpressed in many cancers (e.g., ovarian); enables efficient internalization [41]. |
| Polysaccharides | Hyaluronic Acid (HA) [41] [42] | CD44 Receptor | Binds to CD44, overexpressed in cancer stem cells and many metastatic tumors [41]. |
The Scientist's Toolkit: Essential Research Reagents
The following table details essential materials and reagents required for the formulation and evaluation of ligand-decorated nanocarriers.
Table 3: Research Reagent Solutions for Targeted Nanocarrier Development
| Item | Function/Application | Examples / Notes |
|---|---|---|
| Lipids | Form the core matrix of lipid nanocarriers [41] [42]. | Solid Lipids (e.g., Glyceryl dibehenate/Compritol); Liquid Lipids (e.g., Oleic acid, Caprylic/Capric Triglycerides) [41]. |
| Surfactants | Stabilize the nanoparticle dispersion in aqueous media [41]. | Poloxamer 407, Polysorbate 80, Soy phosphatidylcholine (SPC) [41]. |
| Targeting Ligands | Confer specificity to the target cell population. | RGD Peptides [45], Folate [41], Hyaluronic Acid [41], Antibodies (e.g., anti-EGFR) [43]. |
| PEG-Lipid Conjugates | Impart "stealth" properties by reducing opsonization and MPS clearance [45] [44]. | DSPE-PEG(2000)-COOH, DSG-PEG-NHS; also used for ligand conjugation. |
| Characterization Instruments | Determine physicochemical properties of nanocarriers. | Dynamic Light Scattering (DLS), Zeta Potential Analyzer, Transmission Electron Microscopy (TEM) [45]. |
Experimental Protocols
Protocol 1: Preparation of Ligand-Decorated Nanostructured Lipid Carriers (NLCs)
This protocol describes the formulation of NLCs, a second-generation lipid-based platform known for high drug loading and stability, followed by post-insertion ligand functionalization [41] [42].
Workflow Overview:
Detailed Procedure:
NLC Core Formulation:
- Weigh a mixture of solid lipid (e.g., Compritol 888 ATO) and liquid lipid (e.g., Oleic acid) at a ratio between 70:30 and 99.9:0.1 [41].
- Heat the lipid blend to approximately 5-10°C above the solid lipid's melting point until a clear, homogeneous melt is obtained.
- Separately, heat an aqueous surfactant solution (e.g., 0.5-5% w/v Poloxamer 188) to the same temperature.
- Add the hot aqueous phase to the hot lipid melt under high-speed homogenization (e.g., 10,000-15,000 rpm for 5-10 minutes) to form a coarse pre-emulsion.
- Process the pre-emulsion using a high-pressure homogenizer (HPH) for 3-5 cycles at 500-1500 bar to form fine, uniform NLCs [41].
- Allow the resulting NLC dispersion to cool to room temperature under mild stirring.
Purification and Characterization of "Blank" NLCs:
- Purify the cooled NLC dispersion using dialysis or ultrafiltration to remove free surfactants and any unencapsulated drug.
- Characterize the purified NLCs for:
- Size, Polydispersity Index (PDI), and Zeta Potential: Using Dynamic Light Scattering (DLS). Target size: 20-200 nm; PDI < 0.3 indicates a monodisperse population [44].
- Entrapment Efficiency (EE%): Determine by quantifying the unentrapped drug in the supernatant after ultracentrifugation or filtration. Calculate EE% = (Total drug added - Free drug) / Total drug added × 100% [41].
Ligand Conjugation via Post-Insertion:
- Ligand-PEG-Lipid Preparation: Conjugate the selected ligand (e.g., cRGD peptide) to the terminal group of a functionalized PEG-lipid (e.g., DSPE-PEG(2000)-NHS) via covalent coupling in an appropriate buffer.
- Incubation: Incubate the pre-formed, purified NLCs with the ligand-PEG-lipid conjugate (at a predetermined molar ratio) for 1-2 hours at room temperature or 4°C with gentle agitation. This allows the lipid anchor (DSPE) to insert into the NLC's lipid membrane [42].
- Final Purification: Purify the ligand-decorated NLCs using size exclusion chromatography (e.g., Sephadex G-25 column) or dialysis to remove any uninserted ligand-PEG-lipid conjugates.
Protocol 2: In Vitro Evaluation of Targeting Efficacy
This protocol outlines methods to validate the specificity and enhanced cellular uptake of ligand-functionalized nanocarriers using cell culture models.
Workflow Overview:
Detailed Procedure:
Cell Culture:
- Maintain at least two cell lines: a target cell line that overexpresses the receptor of interest (e.g., KPCY murine pancreatic cancer cells for αvβ3 integrin [45]) and a control cell line with low receptor expression.
- Culture cells in appropriate media and passage them at 70-80% confluence.
Cellular Uptake Study (Quantitative):
- Seed cells in 12-well or 24-well plates at a density of 1-2 x 10^5 cells/well and allow them to adhere for 24 hours.
- Treat cells with equivalent doses (e.g., 50-100 µg/mL nanoparticle content) of non-targeted (PEGylated) and ligand-targeted nanocarriers. For gold nanoparticles (GNPs), a concentration of 7.5 µg/mL has been used [45].
- Incubate for predetermined time points (e.g., 1 h, 4 h, 8 h).
- After incubation, wash the cells thoroughly with phosphate-buffered saline (PBS) to remove non-internalized nanoparticles.
- Lyse the cells using a suitable lysis buffer (e.g., RIPA buffer).
- Quantification: Analyze the cell lysates for nanoparticle content.
- For metal-core NPs (e.g., Gold NPs): Use Inductively Coupled Plasma Mass Spectrometry (ICP-MS) to quantify the metal content, which corresponds to the amount of internalized NPs [45].
- For fluorescently-labeled NPs: Use fluorescence spectrometry or flow cytometry.
Cellular Uptake Study (Qualitative - Confocal Microscopy):
- Seed cells on glass-bottom confocal dishes.
- Treat with fluorescently-labeled non-targeted and targeted nanoparticles.
- After incubation, wash with PBS, fix the cells with 4% paraformaldehyde, and stain cell membranes and nuclei with appropriate dyes (e.g., Wheat Germ Agglutinin-Alexa Fluor 488, DAPI).
- Image using a confocal laser scanning microscope to visualize the intracellular localization of the nanoparticles [45].
Cytotoxicity Assessment (MTT Assay):
- Seed cells in 96-well plates.
- Treat with a concentration range of free drug, non-targeted, and targeted nanocarriers.
- After 24-72 hours, add MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) to each well and incubate for 2-4 hours.
- Solubilize the formed formazan crystals with DMSO and measure the absorbance at 570 nm.
- Calculate cell viability relative to untreated control wells. Targeted formulations should demonstrate lower IC50 values in receptor-positive cells compared to non-targeted ones.
Protocol 3: In Vivo Biodistribution and Tumor Targeting
Evaluating performance in an immunocompetent animal model is crucial, as it accounts for immune system interactions that can significantly impact nanoparticle fate [45].
Detailed Procedure:
Animal Model:
- Use an immunocompetent, syngeneic mouse model bearing relevant tumors (e.g., KPCY pancreatic tumor model in C57BL/6 mice) [45]. This provides a more physiologically relevant assessment of the tumor microenvironment and immune interactions than immunodeficient models.
Biodistribution Study:
- Randomize tumor-bearing mice into treatment groups (e.g., non-targeted NPs vs. ligand-targeted NPs).
- Administer a single dose of nanoparticles via intravenous injection (e.g., via the tail vein).
- At predetermined time points post-injection (e.g., 24 h, 48 h), euthanize the animals and collect tissues of interest: tumor, liver, spleen, kidneys, lungs, and blood.
- Homogenize the tissues and digest the samples.
- Quantification: Use ICP-MS (for metal-core NPs) or fluorescence imaging (for fluorescent NPs) to quantify the amount of nanoparticle accumulation in each tissue. Calculate the percentage of injected dose per gram of tissue (%ID/g) [45].
- Key Analysis: Compare the tumor-to-liver and tumor-to-spleen ratios between non-targeted and targeted groups. An effective targeting strategy should show a statistically significant increase in tumor accumulation and/or a decrease in off-target accumulation in clearance organs.
Critical Considerations and Data Interpretation
When interpreting data from these experiments, researchers must be aware of key challenges. The heterogeneity of the EPR effect between different tumor models and human patients is a major limitation for passive targeting [40]. For active targeting, a critical finding from recent research is that enhanced cellular uptake in vitro does not always translate to improved tumor accumulation in vivo. For instance, RGD-functionalized gold nanoparticles showed significantly higher uptake in cancer cells in vitro but reduced tumor accumulation in vivo due to enhanced clearance by the mononuclear phagocyte system (MPS) [45]. This underscores the necessity of using immunocompetent models for preclinical validation. Furthermore, the density of ligands on the nanoparticle surface must be optimized, as high densities can paradoxically lead to increased immune recognition and rapid clearance [45] [44].
Application Notes
Stimuli-responsive nanosystems represent a paradigm shift in targeted drug delivery, moving from passive carriers to intelligent vehicles that release their payload in response to specific pathological cues. By exploiting the distinct biochemical environments of diseased tissues, these systems significantly enhance therapeutic efficacy while minimizing off-target effects [46] [47]. The following application notes detail the mechanisms and uses of three primary triggers: pH, redox potential, and enzymes.
pH-Responsive Nanosystems
Mechanism and Applications: pH-responsive nanoparticles are designed to exploit the pH gradients that exist at the organ, tissue, and subcellular levels [46]. These systems undergo physicochemical changes—such as swelling, dissociation, or surface charge switching—upon exposure to specific pH thresholds, facilitating targeted drug release [46] [47].
A key application is in oral drug delivery, where systems must survive the acidic stomach (pH 1-3) and release drugs in the more neutral intestines (pH ~7.4). Nanoparticles formulated with acrylic-based polymers like poly(methacrylic acid) (PMAA) remain stable and release minimal drug (e.g., ~10% insulin) in gastric acid. Upon intestinal entry, the carboxyl groups ionize, causing the polymer to swell and release the drug cargo (e.g., ~90% insulin release at pH 7.4) [46]. Commercial formulations like Eudragit L100-55 (dissolves at pH >5.5) and Eudragit S100 (dissolves at pH >7.0) allow for targeted release in specific intestinal regions [46].
In oncology, pH-sensitivity targets the acidic tumor microenvironment (pH 6.5-7.8) and even more acidic endosomal/lysosomal compartments (pH <5.0) [46] [48]. For instance, NPs cross-linked with pH-labile protecting groups (e.g., 2,4,6-trimethoxybenzaldehyde) are stable at neutral pH but swell and release nearly all of their paclitaxel payload within 24 hours at pH 5.0 [46]. Similarly, polymers like PEG-poly(β-amino ester) with a pKb of ~6.5 undergo amine protonation and a sharp micellization-demicellization transition in the mildly acidic tumor environment, triggering drug release [46].
Key Polymers and Their Properties: Numerous synthetic and natural polymers exhibit pH-dependent behavior. The table below summarizes polymers commonly used in pH-responsive drug delivery, along with their specific triggers and applications.
Table 1: Key Polymers for pH-Responsive Drug Delivery
| Polymer/Chemical Group | pH Trigger Mechanism | Application Context | Key Characteristics |
|---|---|---|---|
| Poly(methacrylic acid) (PMAA) & copolymers (e.g., Eudragit) | Swelling/dissolution at pH >5.5 or >7.0 [46] | Oral delivery; Intestinal targeting [46] | Swelling ratios of 40-90 fold; pH-dependent dissolution for duodenal/ileal release [46] |
| PEG-poly(β-amino ester) | Micellization-demicellization at pH ~6.5 (pKb) [46] | Tumor microenvironment targeting [46] | Sharp transition due to amine protonation; increased solubility at acidic pH [46] |
| Chitosan | Deprotonation and NP collapse at neutral pH [46] | Gastric epithelium targeting (e.g., H. pylori); Intestinal release [46] | Stable in stomach acid; destabilizes at higher pH for targeted release [46] |
| Poly(acrylic acid) (PAA) | Swelling/protonation in acidic environments [48] | Endo/lysosomal escape; Cancer therapy [48] | Biocompatible; used in dual-sensitive (e.g., redox/pH) systems [48] |
| Trimethylammonium (TA) groups | Charge reversal from positive (pH<3) to partial negative (pH 7.4) [46] | Electrostatic trapping and release of anionic drugs [46] | Sustained release triggered by electrostatic repulsion at physiological pH [46] |
Redox-Responsive Nanosystems
Mechanism and Applications: Redox-responsive systems primarily exploit the significant difference in glutathione (GSH) concentration between the extracellular space (2-20 µM) and the intracellular cytoplasm (2-10 mM), which is further elevated in the cytoplasm of tumor cells [49] [48]. The most common strategy involves incorporating disulfide bonds (-S-S-) into the nanocarrier structure, which remain stable in the extracellular environment but are cleaved by the high intracellular GSH, leading to nanoparticle disassembly and drug release [49] [48].
A prominent example is a drug delivery system based on Mesoporous Silica Nanoparticles (MSNs) [49]. In this system, the anti-carbonic anhydrase IX (CAIX) antibody is attached to the MSN surface via a disulfide linker. The antibody acts as both a targeting agent and a cap, trapping the drug (e.g., Doxorubicin) within the pores. Upon internalization into CAIX-positive cancer cells, the high intracellular GSH concentration cleaves the disulfide bond, releasing the antibody "cap" and triggering drug release [49]. This system demonstrated enhanced internalization and targeted apoptosis in tumor models.
Another innovative material is Poly(acrylic acid)-cystamine-oleic acid (PAA-ss-OA), which combines redox and pH sensitivity [48]. The disulfide bond in the cystamine bridge is cleaved by GSH, while the PAA component provides pH-sensitive swelling. Erlotinib-loaded lipid nanoparticles coated with PAA-ss-OA (PAA-ETB-NPs, size: ~170 nm) showed superior in vitro cytotoxicity and in vivo tumor growth inhibition in lung cancer models compared to non-responsive NPs or free drug, without significant weight loss in mice [48].
Enzyme-Responsive Nanosystems
Mechanism and Applications: Enzyme-responsive nanosystems are engineered to be cleaved or degraded by specific enzymes that are overexpressed at the disease site, such as proteases, phospholipases, or glycosidases in tumor microenvironments or inflammatory zones [47]. While the provided search results offer less specific protocol detail for enzyme-triggered systems compared to pH and redox, they confirm their status as a key category of chemical stimuli for responsive drug delivery [47].
These systems often use enzyme-specific peptide sequences or ester bonds integrated into the nanoparticle's core or shell. Upon encountering the target enzyme, the cleavage of these bonds destabilizes the nanoparticle architecture, leading to controlled drug release [47]. This strategy is particularly promising for targeting tissues with well-defined enzymatic profiles.
Experimental Protocols
Protocol: Synthesis of a Redox-Responsive MSN-Based Delivery System (MSNs-CAIX)
This protocol outlines the synthesis of antibody-targeted, redox-responsive mesoporous silica nanoparticles for targeted drug delivery, based on the work of [49].
Research Reagent Solutions:
- Surfactant Template Solution: 1.04 g of 25 wt% cetyltrimethyl ammonium chloride (CTAC) in 6.4 mL deionized water.
- Silica Precursor: Tetraethylorthosilicate (TEOS).
- Functionalization Agent: 3-mercaptopropyltrimethoxysilane (MPTMS).
- Activation Agent: 2,2'-dipyridyl disulfide (2,2'-dpd) in phosphate buffer saline (PBS, pH 4.6).
- Targeting Ligand: Anti-Carbonic Anhydrase IX (CAIX) antibody.
- Sulfhydryl Activation for Antibody: 2-Iminothiolane hydrochloride (2-IT) in sodium borate buffer.
- Model Drug: Doxorubicin hydrochloric (DOX).
Table 2: Key Research Reagent Solutions and Their Functions
| Reagent/Solution | Function in the Protocol |
|---|---|
| Cetyltrimethyl ammonium chloride (CTAC) | Porogen template for mesoporous silica nanoparticle synthesis [49]. |
| Tetraethylorthosilicate (TEOS) | Silica source for nanoparticle formation [49]. |
| 3-mercaptopropyltrimethoxysilane (MPTMS) | Provides thiol (-SH) groups for surface functionalization [49]. |
| 2,2'-dipyridyl disulfide (2,2'-dpd) | Activates thiolated surfaces for disulfide bond formation [49]. |
| 2-Iminothiolane (2-IT) | Thiolates the primary amines of the antibody for conjugation [49]. |
| Glutathione (GSH) | Reductive stimulus for triggering drug release in vitro and in cells [49]. |
Step-by-Step Procedure:
Synthesis of MSNs:
- Mix CTAC solution, deionized water, diethanolamine (DEA), and ethanol. Stir at 40 °C for 30 min.
- Add TEOS dropwise and stir vigorously for 2 h.
- Recover nanoparticles by centrifugation and remove the surfactant template by refluxing in acidic ethanol (2 mL HCl in 250 mL ethanol) at 80 °C for 8 h.
- Wash the resulting MSNs thoroughly and dry under vacuum [49].
Surface Thiol Functionalization (MSNs-SH):
- Add MPTMS to the reaction mixture of MSNs before the surfactant removal step.
- Stir for 2 h under a nitrogen atmosphere.
- Recover the mercaptopropyl-functionalized MSNs (MSNs-SH) by centrifugation, wash with ethanol, and remove surfactants as in Step 1 [49].
Surface Activation (MSNs-S-S-P):
- Disperse MSNs-SH in PBS (pH 4.6).
- Add 2,2'-dpd and stir for 24 h at room temperature.
- Recover the activated nanoparticles (MSNs-S-S-P) by centrifugation, wash with water, and freeze-dry [49].
Antibody Thiolation (CAIX-SH):
- Dissolve the CAIX antibody in sodium borate buffer.
- Add 2-IT solution and stir for 1 h at room temperature.
- Purify the thiolated antibody (CAIX-SH) using an ultrafiltration centrifuge tube (MWCO 30 kDa) [49].
Antibody Conjugation (MSNs-CAIX):
- Suspend MSNs-S-S-P in PBS (pH 7.4) containing dimethyl sulfoxide (DMSO).
- Add the purified CAIX-SH and stir gently for 24 h at room temperature.
- Wash the resulting antibody-conjugated nanoparticles (MSNs-CAIX) with water and collect by centrifugation [49].
Drug Loading:
- Incubate MSNs-S-S-P (from Step 3) with a solution of DOX.
- Stir to allow the drug to diffuse into the pores.
- Subsequent conjugation of the thiolated antibody (Step 5) will cap the pores, entrapping the drug and creating the final DOX@MSNs-CAIX construct [49].
Characterization:
- Size and Morphology: Analyze using Scanning Electron Microscopy (SEM) and Transmission Electron Microscopy (TEM). Typical MSNs from this protocol are 20-50 nm [49].
- Surface Chemistry: Confirm functionalization steps using Fourier-Transform Infrared Spectroscopy (FTIR) and Raman spectroscopy [49].
- Porosity: Determine surface area and pore volume using N₂ adsorption-desorption isotherms [49].
Protocol: Formulation of Dual Redox/pH-Responsive Lipid Nanoparticles
This protocol describes the preparation of PAA-ss-OA-modified lipid nanoparticles for the delivery of Erlotinib, as described by [48].
Research Reagent Solutions:
- Polymer: Poly(acrylic acid)-cystamine-oleic acid (PAA-ss-OA).
- Drug: Erlotinib (ETB).
- Lipid Components: Oleic acid (OA) and Glyceryl monostearate (GMS).
- Surfactant: Tween 80 in water (1% w/v).
- Solvent: Chloroform.
Step-by-Step Procedure:
Synthesis of PAA-ss-OA:
- Activate OA by mixing with EDC and NHS in DMSO for 1 h.
- Add cystamine to the mixture and stir for 10 h to form ss-OA.
- Add PAA to the ss-OA mixture and stir for 12 h.
- Dialyze the final product (PAA-ss-OA) against water for 3 days using a dialysis membrane (MWCO 3,500 Da) [48].
Preparation of Nanoparticle Core:
- Dissolve ETB, OA, and GMS in chloroform.
- Add this organic phase to an aqueous phase containing 1% Tween 80.
- Homogenize the mixture at 15,000 rpm for 3 minutes to form a coarse emulsion [48].
Surface Modification and Evaporation:
- Dissolve PAA-ss-OA in chloroform and add it to the homogenized emulsion.
- Stir the resulting mixture at 600 rpm for 3 hours to allow the polymer to coat the forming nanoparticles and for complete chloroform evaporation.
- This yields the final PAA-ETB-NPs [48].
- Control particles (ETB-NPs) are prepared using the same method but omitting PAA-ss-OA.
Characterization:
- Size and Zeta Potential: Determine using dynamic light scattering (e.g., Malvern Zetasizer). PAA-ETB-NPs typically have a size of ~170 nm and a zeta potential of ~ -32 mV [48].
- Drug Loading and Encapsulation Efficiency: Quantify using HPLC. This system achieved encapsulation efficiency >85% and drug loading capacity of ~2.6% [48].
- In Vitro Drug Release: Perform release studies in PBS at different pH values (e.g., 7.4 and 5.0) and with/without the reducing agent GSH (e.g., 10 mM) to confirm dual responsiveness [48].
Signaling Pathways and Workflow Diagrams
pH-Responsive Nanoparticle Mechanism
Diagram 1: pH-Triggered Intracellular Drug Release Pathway. This diagram illustrates the journey of a pH-sensitive nanoparticle from systemic circulation to intracellular drug release, leveraging the decreasing pH of the endocytic pathway.
Redox-Responsive MSNs Workflow
Diagram 2: Redox-Responsive MSNs Synthesis. Workflow for synthesizing and loading antibody-capped, redox-responsive mesoporous silica nanoparticles (DOX@MSNs-CAIX).
Multi-Stimuli Responsive Drug Release Logic
Diagram 3: Multi-Stimuli Responsive Release Logic. The decision-making logic of a dual-responsive nanoparticle (e.g., pH and redox), ensuring drug release only when multiple disease-specific stimuli are present.
The efficacy of therapeutic agents is often limited by the body's sophisticated biological barriers. The blood-brain barrier (BBB) and various mucosal layers represent two significant challenges in drug delivery, particularly for the treatment of central nervous system (CNS) disorders and diseases requiring mucosal absorption. The BBB is a highly selective semipermeable border that protects the brain from harmful substances in the blood, while simultaneously restricting the passage of over 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics [50] [51]. Similarly, mucosal barriers found in the respiratory, gastrointestinal, and nasal passages protect underlying tissues through their viscoelastic, selectively permeable properties, which can trap and remove particulate matter, including drug carriers [52].
Nanotechnology offers innovative solutions to overcome these obstacles. This application note provides a detailed overview of the structure and function of these barriers, supported by quantitative data, and presents standardized protocols for developing nanocarriers capable of traversing them. The content is framed within the broader context of applying nanotechnology in targeted drug delivery systems research, with a focus on practical methodologies for researchers, scientists, and drug development professionals.
The Blood-Brain Barrier (BBB)
Structure and Physiological Function
The BBB is a multicellular vascular structure that maintains CNS homeostasis through sophisticated cellular interactions. Its core components include brain microvascular endothelial cells connected by tight junctions (TJs), pericytes embedded in the basement membrane, and astrocytes whose end-feet encase the vasculature [50] [51]. These components collectively form a neurovascular unit that precisely regulates molecular exchange between blood and brain tissue.
The TJs between endothelial cells are primarily composed of proteins such as claudins, occludin, and junctional adhesion molecules (JAMs), which create a physical barrier that eliminates paracellular transport of most molecules [53] [51]. This structure results in high transendothelial electrical resistance (TEER), typically ranging from 1500-2000 Ω·cm² in humans, significantly restricting passive diffusion [51].
Transport Mechanisms Across the BBB
Understanding the natural transport mechanisms of the BBB is crucial for designing effective nanocarriers. The table below summarizes the primary transport pathways and their characteristics.
Table 1: Primary Transport Mechanisms Across the Blood-Brain Barrier
| Transport Mechanism | Description | Substrate Characteristics | Nanocarrier Design Implications |
|---|---|---|---|
| Passive Diffusion | Movement of molecules down concentration gradient without energy expenditure | Small (<400-500 Da), lipophilic (LogP>2), limited hydrogen bonds (<6) [50] [51] | Limited utility for nanocarriers due to size restrictions |
| Carrier-Mediated Transcytosis (CMT) | Uses specific membrane transporters for essential nutrients | Glucose (via GLUT1), amino acids (via LAT1), structurally similar drugs [54] [50] | Surface modification to mimic natural substrates |
| Receptor-Mediated Transcytosis (RMT) | Vesicular transport initiated by ligand-receptor binding | Transferrin, insulin, lipoproteins; specific receptor ligands [22] [54] [50] | Conjugation with targeting ligands (e.g., transferrin, peptides) |
| Adsorptive-Mediated Transcytosis (AMT) | Charge-mediated interactions with membrane components | Cationic proteins and cell-penetrating peptides [22] [50] | Surface cationization with positive charges |
| Cell-Mediated Transcytosis | Utilization of immune cells to cross BBB | Monocytes, macrophages, neutrophils [54] [50] | Cell-based delivery systems or biomimetic approaches |
The following diagram illustrates the primary transport mechanisms utilized by nanocarriers to cross the BBB:
Quantitative Parameters for BBB Penetration
The following table summarizes key physicochemical properties that influence nanoparticle transport across the BBB, as established by current research.
Table 2: Optimal Physicochemical Properties of Nanoparticles for BBB Penetration
| Parameter | Optimal Range | Impact on BBB Penetration | Experimental Measurement Methods |
|---|---|---|---|
| Size | 10-100 nm [55] | Smaller particles (<100 nm) generally show enhanced penetration, but very small particles (<10 nm) may be rapidly cleared | Dynamic light scattering (DLS), transmission electron microscopy (TEM) |
| Surface Charge | Slightly negative to neutral [56] | Cationic surfaces may enhance AMT but increase protein adsorption and toxicity; neutral surfaces prolong circulation | Zeta potential measurement |
| Hydrophobicity/Lipophilicity | Balanced amphiphilicity | Enhances interaction with endothelial cell membranes but must be balanced with circulation time | Log P measurement, contact angle analysis |
| Surface Functionalization | PEGylation, ligand conjugation | PEGylation reduces opsonization and prolongs circulation; targeting ligands enhance specific uptake | Spectroscopy, chromatography, surface plasmon resonance |
| Shape | Spherical preferred | Affects flow dynamics and endothelial interaction | Electron microscopy, atomic force microscopy |
Mucosal Barriers
Structure and Function of Mucosal Layers
Mucosal barriers protect epithelial surfaces throughout the body, including the respiratory, gastrointestinal, and genitourinary tracts. Mucus is a viscoelastic, adhesive hydrogel composed primarily of mucin glycoproteins, water, lipids, enzymes, and electrolytes [52]. This complex matrix forms a selectively permeable barrier that can trap and remove pathogens and particulate matter, presenting a significant challenge for drug delivery.
The structural properties of mucus vary significantly by anatomical location, with differences in thickness, composition, turnover rate, and pH influencing nanoparticle behavior. For instance, nasal mucus has a relatively rapid turnover rate (15-20 minutes), while gastrointestinal mucus may persist for longer periods [52] [53].
Strategies for Mucosal Penetration
Two primary strategies have emerged for enhancing nanoparticle transport across mucosal barriers: mucoadhesion and mucopenetration. Mucoadhesive systems are designed to adhere to the mucus layer, prolonging residence time at the absorption site, while mucopenetrative systems are engineered to rapidly traverse the mucus layer to reach the underlying epithelium [52]. The choice between these strategies depends on the specific therapeutic application and anatomical location.
The following diagram illustrates the key differences in nanoparticle behavior for mucoadhesion versus mucopenetration:
Quantitative Analysis of Mucosal Penetration
The following table outlines key parameters that influence nanoparticle interactions with mucosal barriers.
Table 3: Design Parameters for Mucosal Drug Delivery Systems
| Parameter | Mucoadhesive Strategy | Mucopenetrative Strategy | Measurement Techniques |
|---|---|---|---|
| Surface Chemistry | Cationic, thiolated, or lectin-functionalized surfaces | Neutral, hydrophilic surfaces (e.g., PEG) with dense coating | Zeta potential, fluorescence labeling |
| Size | 50-500 nm (broader range acceptable) | 50-200 nm (smaller preferred) | Dynamic light scattering |
| Diffusion Coefficient | Low (≤10⁻¹¹ cm²/s) | High (≥10⁻⁹ cm²/s) | Single-particle tracking (SPT) |
| Mean Squared Displacement | Confined or subdiffusive motion | Linear or superdiffusive motion | Single-particle tracking (SPT) |
| Mucus Turnover Consideration | Designed to resist clearance | Designed to penetrate before clearance | Site-specific optimization |
Experimental Protocols
Protocol: Preparation of BBB-Targeted Nanoparticles
Objective: Synthesize and characterize polymeric nanoparticles functionalized with transferrin receptor ligands for enhanced BBB penetration.
Materials:
- PLGA (Poly(lactic-co-glycolic acid)): Biodegradable polymer matrix (50:50 LA:GA ratio)
- PEG-b-PLGA block copolymer: For PEGylation and stealth properties
- Transferrin peptide ligand (TfR-binding peptide): For receptor-mediated transcytosis
- Dichloromethane (DCM): Organic solvent for emulsion preparation
- Polyvinyl alcohol (PVA): Surfactant for emulsion stabilization
- Dialysis membrane (MWCO 12-14 kDa): For purification
- Fluorescent dye (DiR or similar): For tracking and visualization
Procedure:
Nanoparticle Formation using Double Emulsion Method:
- Dissolve 50 mg PLGA and 10 mg PEG-b-PLGA in 3 mL DCM
- Add aqueous solution containing the drug payload (50-100 μL) and emulsify using probe sonication (50 W, 30 s) to form primary W/O emulsion
- Add this primary emulsion to 10 mL of 2% PVA solution and homogenize (10,000 rpm, 2 min) to form W/O/W double emulsion
- Stir overnight to evaporate organic solvent
- Collect nanoparticles by centrifugation (15,000 rpm, 30 min) and wash three times with distilled water
Surface Functionalization:
- Resuspend nanoparticles in PBS (pH 7.4) at 10 mg/mL concentration
- Add NHS-PEG-Maleimide linker (molar ratio 5:1 nanoparticle:linker) and incubate for 2 hours at room temperature
- Purify by centrifugation and resuspend in PBS
- Add thiolated transferrin peptide ligand (molar ratio 1:1 with maleimide groups) and incubate for 4 hours at 4°C
- Purify functionalized nanoparticles by centrifugation and store at 4°C
Characterization:
- Size and Zeta Potential: Dilute nanoparticles in PBS (1:100) and measure using dynamic light scattering
- Morphology: Examine using transmission electron microscopy with negative staining
- Ligand Density: Quantify using fluorescence spectroscopy or ELISA-based assays
- Drug Loading Efficiency: Determine by HPLC analysis of supernatant after nanoparticle dissolution
Protocol: Single-Particle Tracking for Mucosal Penetration
Objective: Evaluate nanoparticle diffusion behavior in mucosal layers using single-particle tracking (SPT) to distinguish between mucoadhesive and mucopenetrative properties.
Materials:
- Fresh mucus samples: Human or porcine intestinal/respiratory mucus
- Fluorescently labeled nanoparticles: Test and control formulations
- Glass-bottom culture dishes: For microscopy
- Total Internal Reflection Fluorescence (TIRF) microscope: With high-sensitivity EMCCD camera
- Tracking software: e.g., ImageJ with TrackMate or custom MATLAB scripts
- Reference nanoparticles: Positive and negative controls for diffusion
Procedure:
Sample Preparation:
- Thaw mucus samples slowly on ice and centrifuge at 4,000 × g for 10 min to remove debris
- Dilute fluorescent nanoparticles in PBS to working concentration (~10⁹ particles/mL)
- Mix 10 μL of nanoparticle suspension with 90 μL of mucus and incubate for 15 min at 37°C
- Transfer 30 μL of mixture to glass-bottom dish and create a thin, even layer
Image Acquisition:
- Use TIRF microscope with 100× oil immersion objective
- Acquire videos at 50-100 frames per second for 1-2 minutes
- Maintain temperature at 37°C using environmental chamber
- Ensure appropriate particle density (20-50 particles per frame) for reliable tracking
Data Analysis:
- Identify particle centroids in each frame using appropriate detection algorithms
- Reconstruct trajectories using nearest-neighbor algorithm with maximum displacement constraint
- Calculate mean squared displacement (MSD) for each trajectory: MSD(τ) = ⟨[x(t+τ) - x(t)]² + [y(t+τ) - y(t)]²⟩
- Classify motion types based on MSD scaling with time:
- Directed motion: MSD ~ τ²
- Brownian motion: MSD ~ τ
- Confined motion: MSD ~ τ⁰
- Compute effective diffusion coefficients from MSD plots
Interpretation:
- Mucopenetrative nanoparticles exhibit higher diffusion coefficients (>10⁻⁹ cm²/s) and linear MSD plots
- Mucoadhesive nanoparticles show lower diffusion coefficients (<10⁻¹¹ cm²/s) and confined MSD profiles
- Compare test formulations with appropriate controls for statistical significance
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Nanocarrier Development
| Reagent/Category | Function/Application | Examples/Specific Products |
|---|---|---|
| Polymeric Materials | Nanoparticle matrix formation | PLGA, PLA, PEG, chitosan, gelatin |
| Lipid Components | Liposome and lipid nanoparticle formation | Phosphatidylcholine, cholesterol, DSPE-PEG |
| Targeting Ligands | Receptor-specific binding for RMT | Transferrin, lactoferrin, TfR antibodies, RVG29 peptide |
| Cell-Penetrating Peptides | Enhance cellular uptake and AMT | TAT peptide, penetratin, synthetic CPPs |
| Cationic Modifiers | Promote adsorptive-mediated transcytosis | Poly-L-lysine, PEI, chitosan, cationic lipids |
| Mucus-Penetrating Agents | Surface modification for mucosal penetration | PEG, Pluronics, low MW PEI |
| Characterization Tools | Physicochemical property analysis | Malvern Zetasizer, TEM, HPLC, fluorescence spectroscopy |
| Biological Models | In vitro and in vivo barrier assessment | Transwell models, iPSC-derived BBB models, animal models |
The development of effective nanocarriers capable of overcoming biological barriers requires a comprehensive understanding of both BBB and mucosal physiology. By leveraging specific transport mechanisms and optimizing nanocarrier design parameters, researchers can significantly enhance drug delivery to previously inaccessible targets. The protocols and data presented in this application note provide a foundation for systematic investigation of nanocarrier-barrier interactions, with particular emphasis on quantitative assessment of penetration efficiency. As the field advances, continued refinement of these approaches will be essential for translating nanomedicine from bench to bedside, particularly for neurological disorders where the BBB presents a formidable challenge to conventional therapeutics. Future directions will likely include more sophisticated targeting strategies, responsive materials that adapt to barrier conditions, and personalized approaches based on individual barrier characteristics.
The application of nanotechnology in oncology represents a paradigm shift in cancer treatment, addressing critical limitations of conventional therapies such as systemic toxicity, poor drug bioavailability, and lack of specific targeting [57] [58]. Targeted drug delivery systems (DDS) enhance the therapeutic index of anticancer agents by increasing tumor-specific accumulation, enabling controlled release, and improving intracellular drug uptake [57]. These systems leverage unique tumor pathophysiology, including the enhanced permeability and retention (EPR) effect, aberrant metabolic profiles, and overexpressed receptors, to achieve precise targeting while minimizing off-target effects [59] [60].
Nanoparticle-based platforms provide versatile foundations for co-delivering diverse therapeutic payloads, including small-molecule chemotherapeutics and macromolecular RNA-based drugs [61] [62]. The convergence of material science, biology, and medicine in nanomedicine facilitates the development of multifunctional systems capable of overcoming biological barriers, modulating the tumor microenvironment (TME), and reversing drug resistance mechanisms [63] [64]. This document details current applications, experimental methodologies, and technical protocols for utilizing nanotechnology in oncology drug delivery, providing a practical framework for research and development.
Nanoparticle Platforms for Drug Delivery
Classification and Properties
Nanoparticle (NP) platforms are broadly categorized based on their structural composition and material properties. The design parameters, including size, surface charge, shape, and elasticity, critically influence their in vivo pharmacokinetics, biodistribution, and tumor accumulation [64]. The following table summarizes major NP classes and their characteristics relevant to oncology drug delivery.
Table 1: Major Classes of Nanoparticles for Cancer Drug Delivery
| Nanoparticle Type | Key Components | Therapeutic Payload | Key Advantages | Clinical Examples |
|---|---|---|---|---|
| Lipid-based NPs | Phospholipids, cholesterol, PEG-lipids [62] | siRNA, mRNA, chemotherapeutics [65] [62] | High biocompatibility, efficient intracellular delivery, clinical translation feasibility | Onpattro (siRNA), COVID-19 mRNA Vaccines [62] |
| Polymeric NPs | PLGA, Chitosan, PEG-PLGA copolymers [57] | Chemotherapeutics, proteins, nucleic acids [57] | Controlled release kinetics, tunable degradation, surface functionalization | (Under investigation) [57] |
| Liposomes | Phospholipid bilayers, aqueous core [57] | Hydrophilic & hydrophobic chemotherapeutics [57] | High drug loading, passive targeting via EPR effect, proven clinical track record | Doxil (Pegylated liposomal doxorubicin) [57] [60] |
| Inorganic NPs | Silica, iron oxide, gold [59] [64] | Chemotherapeutics, immunotherapeutics [59] | Unique physicochemical properties (e.g., magnetism, porosity), stimuli-responsiveness | (Under investigation) [64] |
| Hybrid NPs | Polymer-lipid blends, inorganic-core with lipid/polymer shell [57] [61] | Combination therapies (chemo + RNAi) [61] | Synergistic properties, multi-functionality, enhanced stability | (Under investigation) [57] [61] |
Targeting Strategies
Two primary targeting strategies are employed to direct NPs to tumor tissues:
- Passive Targeting: Leverages the EPR effect, where the leaky vasculature and impaired lymphatic drainage of tumors promote the selective accumulation of nanocarriers (typically 10-200 nm) [63] [60]. This is a ubiquitous feature for most nano-delivery systems.
- Active Targeting: Incorporates targeting ligands (e.g., antibodies, peptides, aptamers, small molecules) on the NP surface that bind specifically to receptors overexpressed on cancer cells or within the TME [57] [60]. Examples include targeting the CXCL12/CXCR4 axis in bone metastases or EGFR in various solid tumors [63] [62].
Application Note I: Targeted Delivery of Chemotherapeutics
Lactate-Gated Tumoral Drug Release
Background: The "Warburg effect" describes the propensity of cancer cells to metabolize glucose to lactate, even under normoxic conditions. This leads to a lactate-rich TME, which can be exploited for targeted drug release [59].
Mechanism: A novel silica nanoparticle system utilizes a lactate-specific enzymatic switch. The NP pores are capped with a hydrogen peroxide-sensitive material. The enzyme lactate oxidase, immobilized on the NP, converts lactate to pyruvate, generating hydrogen peroxide. At sufficiently high concentrations (found in the TME), the locally generated hydrogen peroxide degrades the capping material, triggering drug release [59].
Diagram: Mechanism of Lactate-Gated Drug Release
Experimental Validation & Protocol:
In vivo Efficacy Study in Murine Models
- Objective: To evaluate the tumor-targeting efficiency and therapeutic efficacy of lactate-gated doxorubicin-loaded nanoparticles (Lac-NP-Dox) versus free doxorubicin (Free-Dox) and non-gated nanoparticles (NP-Dox) [59].
- Materials:
- Mice bearing subcutaneous tumors (e.g., breast cancer, sarcoma models).
- Lactate-gated silica nanoparticles loaded with doxorubicin (Lac-NP-Dox).
- Control groups: Free-Dox, NP-Dox, saline.
- Procedure:
- Treatment Administration: Inject formulations intravenously via the tail vein at a doxorubicin dose of 5 mg/kg. Repeat weekly for 3-4 weeks [59].
- Biodistribution Analysis: 24 hours post-injection, sacrifice a subset of mice (n=3-5 per group). Harvest tumors and major organs (heart, liver, spleen, lungs, kidneys). Homogenize tissues and quantify doxorubicin fluorescence using HPLC or a fluorescence plate reader. Calculate the percentage of injected dose per gram of tissue (%ID/g) [59].
- Efficacy Monitoring: Measure tumor dimensions with digital calipers 2-3 times weekly. Calculate tumor volume (V = (L × W²)/2). Monitor mouse body weight as an indicator of systemic toxicity. Perform survival analysis [59].
Key Results (Representative Data):
- Table 2: Biodistribution and Efficacy of Lactate-Gated NPs in a Mouse Model [59]
Parameter Free Doxorubicin Non-Gated NP-Dox Lac-NP-Dox Tumor Drug Accumulation (%ID/g) ~2.5 ~5.1 ~25.0 Heart Drug Accumulation (%ID/g) High Moderate Low Tumor Growth Inhibition Moderate Improved Significant Suppression Systemic Toxicity (Weight Loss) Significant Reduced Minimal
Bone-Targeted Delivery for Metastases
Background: Bone metastases are a debilitating consequence of cancers like breast and prostate carcinoma. The bone microenvironment presents a significant barrier to drug delivery [63] [66].
Mechanism: Bisphosphonates (BPs), such as alendronate and zoledronate, exhibit a strong affinity for hydroxyapatite, the mineral component of bone. Conjugating BPs to nanoparticles (e.g., liposomes, polymeric NPs) facilitates active targeting to bone metastatic sites [63] [66]. This strategy enhances drug concentration at the diseased tissue, mitigating systemic side effects.
Experimental Protocol:
- In vivo Targeting Efficacy to Bone Metastases
- Objective: To assess the bone-targeting capability and antitumor effect of BP-conjugated, drug-loaded nanoparticles in a model of breast cancer bone metastasis.
- Materials:
- Mice with established bone metastases (e.g., via intracardiac injection of MDA-MB-231-luc cells).
- BP-conjugated paclitaxel-loaded PLGA nanoparticles (BP-NP-PTX).
- Control: Non-targeted NP-PTX.
- Procedure:
- Model Establishment: Inject luciferase-tagged cancer cells into the left cardiac ventricle of immunodeficient mice. Monitor metastasis weekly via bioluminescent imaging (BLI) [63].
- Treatment: Once BLI signal is confirmed in hind limbs, randomize mice into treatment groups. Administer BP-NP-PTX, NP-PTX, or saline intravenously weekly.
- Analysis: Quantify tumor burden by BLI weekly. Monitor bone lesion formation and progression via micro-CT imaging. At endpoint, perform histomorphometric analysis of tibiae for tumor area and osteoclast activity (TRAP staining) [63] [66].
Application Note II: Targeted Delivery of RNA-based Drugs
RNA Therapeutics and Delivery Challenges
RNA-based therapeutics, including small interfering RNA (siRNA), messenger RNA (mRNA), and microRNA (miRNA), enable precise intervention at the genetic level [65]. However, their clinical translation is hampered by inherent challenges: poor stability in circulation due to rapid enzymatic degradation, inefficient cellular uptake, and immune activation [65] [62]. Lipid nanoparticles (LNPs) have emerged as the leading platform for systemic RNA delivery, offering protection, enhanced cellular uptake, and endosomal escape [65] [62].
Diagram: LNP-mediated RNA Delivery to Cancer Cells
siRNA Delivery for Oncogene Silencing in HCC
Background: Hepatocellular carcinoma (HCC) progression is driven by dysregulated signaling pathways (e.g., VEGF, EGFR, FGF) [62]. siRNA offers a means to silence these oncogenic drivers with high specificity.
Mechanism: LNPs encapsulating siRNA against key oncogenic targets (e.g., VEGFR2, EGFR) are systemically administered. The liver's fenestrated endothelium facilitates LNP accumulation. A critical mechanism involves the adsorption of apolipoprotein E (ApoE) from serum onto LNPs, which then binds to the low-density lipoprotein receptor (LDLR) highly expressed on hepatocytes and hepatoma cells, promoting receptor-mediated uptake [62].
Experimental Protocol:
In vivo Gene Silencing and Anti-Tumor Efficacy
- Objective: To evaluate the potency of EGFR-siRNA loaded LNPs (LNP-EGFR-siRNA) in suppressing tumor growth in an orthotopic HCC model.
- Materials:
- Orthotopic HCC mouse model (e.g., HepG2-luc cells implanted in liver).
- LNP-EGFR-siRNA (ionizable lipid:DSPC:Cholesterol:DMG-PEG2000 at 50:10:38.5:1.5 molar ratio).
- Control: LNP loaded with non-targeting siRNA (LNP-NT-siRNA).
Procedure:
- Formulation: Prepare LNPs using ethanol-drop microfluidics. Mix lipids in ethanol with siRNA in aqueous citrate buffer (pH 4.0) at a fixed flow rate. Dialyze against PBS to remove ethanol and raise pH [62].
- Characterization: Determine particle size and zeta potential using dynamic light scattering. Measure siRNA encapsulation efficiency using a Ribogreen assay.
- Treatment: Randomize mice with established HCC tumors. Inject LNP formulations intravenously at an siRNA dose of 1-3 mg/kg, twice weekly for 3 weeks [62].
- Analysis:
- Gene Silencing: Isolate tumor proteins 48h after the last dose. Analyze EGFR protein levels by Western Blot or ELISA. Normalize to a housekeeping protein (e.g., GAPDH) [62].
- Efficacy: Monitor tumor growth weekly via BLI or ultrasound. At endpoint, harvest livers and measure tumor weight and number. Perform immunohistochemistry for EGFR, Ki67 (proliferation), and TUNEL (apoptosis) [62].
Key Results (Representative Data):
- Table 3: Efficacy of Targeted siRNA-LNPs in an HCC Model [62]
Parameter LNP-NT-siRNA LNP-EGFR-siRNA Tumor EGFR Protein Level (% of Control) ~95% ~25% Final Tumor Volume (mm³) ~450 ~150 Tumor Proliferation Index (Ki67+ %) ~40% ~15% Apoptotic Index (TUNEL+ %) ~5% ~20%
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Nanoparticle Formulation and Testing
| Reagent / Material | Function / Application | Example / Notes |
|---|---|---|
| Ionizable Cationic Lipids | Core component of LNPs for RNA encapsulation; enables endosomal escape [62] | DLin-MC3-DMA, SM-102, ALC-0315 |
| PEG-Lipids | Stabilizes nanoparticles, reduces protein opsonization, modulates pharmacokinetics [62] | DMG-PEG2000, DSG-PEG2000, ALC-0159 |
| Bisphosphonates | Bone-targeting ligand for conjugation to NPs; directs delivery to bone metastases [63] [66] | Alendronate, Zoledronate |
| Lactate Oxidase | Key enzyme for constructing lactate-responsive drug delivery switches [59] | Immobilized on nanoparticle surface |
| siRNA/mRNA | Active pharmaceutical ingredient for RNA-based therapeutics [65] [62] | Target-specific siRNA (e.g., vs. VEGF, EGFR); mRNA for antigen expression |
| PLGA Polymer | Biodegradable polymer core for sustained release of chemotherapeutics [57] [63] | Varies in molecular weight and lactide:glycolide ratio |
| Cell Lines | In vitro and in vivo modeling of cancer | HepG2 (HCC), MDA-MB-231 (Breast Cancer), PANC-1 (Pancreatic Cancer) [62] [63] [64] |
| Animal Models | Preclinical evaluation of biodistribution, efficacy, and safety | Subcutaneous xenografts, orthotopic models, genetically engineered models, metastasis models (e.g., intracardiac injection) [62] [63] [59] |
The convergence of nanotechnology with diagnostics and regenerative medicine is fundamentally reshaping therapeutic development. Nano-based drug delivery systems (NDDS) leverage materials at the 1-100 nanometer scale to exploit unique physicochemical properties, enabling unprecedented control over drug release, targeting precision, and diagnostic capability [67] [1]. These advanced formulations address critical challenges in modern medicine, including biological barrier penetration, therapeutic bioactivity preservation, and spatiotemporal control of drug release. By integrating targeting moieties, imaging agents, and therapeutic payloads into single platforms, these multifunctional nanocarriers are paving the way for personalized treatment approaches across oncology, neurology, and chronic disease management [68] [69]. This document provides application notes and experimental protocols for developing and characterizing these sophisticated systems within a targeted drug delivery research framework.
Application Notes: Key Nanoplatforms and Their Applications
The strategic selection of nanomaterial composition dictates the functionality, biodistribution, and release kinetics of advanced formulations. The following platforms represent the most promising candidates for integrated diagnostic and regenerative applications.
Table 1: Key Nanomaterial Platforms for Diagnostic and Regenerative Applications
| Nanomaterial | Core Composition | Key Applications | Functional Advantages | Representative Formulations |
|---|---|---|---|---|
| Liposomes | Phospholipid bilayer [69] | Drug delivery, Bio-imaging [68] | Biocompatibility; Co-encapsulation of hydrophilic/hydrophobic drugs; Prolonged circulation via PEGylation [69] | Doxil, LipoDox (PEGylated), Myocet (non-PEGylated) [69] |
| Polymeric Nanoparticles | PLGA, PLA, Chitosan [70] [71] | Controlled drug release, Tissue engineering scaffolds [67] [72] | Biodegradability; Tunable release profiles; Sustained drug release; Enhanced BBB penetration [70] [71] | Genexol-PM (Paclitaxel-loaded micelles) [69] |
| Dendrimers | PAMAM, PPI [67] [69] | Targeted drug delivery, Gene therapy [67] [69] | Monodisperse structure; High drug-loading capacity; Multivalent surface functionalization [69] | VivaGel (Anti-HIV microbicide) [69] |
| Metallic Nanoparticles | Gold, Iron Oxide, Silver [68] [69] | Theranostics, Photothermal therapy, MRI contrast [68] [69] | Unique optical/magnetic properties; Surface Plasmon Resonance; Stimuli-responsive release (e.g., NIR, magnetic fields) [69] | Ferumoxytol (Iron oxide-based, MRI contrast) [69] |
| Solid Lipid Nanoparticles (SLNs) | Natural/ synthetic lipids [71] | Intranasal CNS delivery, Antioxidant delivery [71] | Enhanced biocompatibility; Improved drug loading; Scalable production; Bypassing BBB [71] | Green SLNs from natural soaps [71] |
Breaking the Barrier: Nanocarriers for CNS Delivery
The blood-brain barrier (BBB) remains the most significant challenge for neurologic therapeutics. Research demonstrates that ligand-functionalized nanoparticles can exploit endogenous transport mechanisms to achieve CNS delivery. A recent study systematically compared poly(lactide-co-glycolide) (PLGA), albumin (BSA/HSA), and nanolipid carriers (NLC), with and without transferrin (Tf) ligands, for interaction with human BBB cellular components (endothelial cells, pericytes, astrocytes) [70]. Key findings indicate that Tf-conjugated albumin nanoparticles (BSA-Tf, HSA-Tf) exhibited significantly higher uptake in human brain microvascular endothelial cells (hBMECs) in a dose-dependent manner without inducing cytotoxicity at concentrations up to 62.5 µg/mL [70]. Ultrastructural analysis revealed distinct cellular processing pathways, with autophagy emerging as a critical mechanism for nanoparticle handling in pericytes and astrocytes [70].
Integrated Theranostic Platforms
The fusion of diagnostic and therapeutic functions into a single nanoplatform enables real-time treatment monitoring and personalized dosing. Gold nanoparticles (AuNPs) and iron oxide nanoparticles (IONPs) are pioneering this space. AuNPs serve as potent agents for photoacoustic imaging and photothermal therapy due to their surface plasmon resonance, while IONPs function as T2-weighted MRI contrast agents and can mediate magnetothermal therapy [69]. These inorganic cores can be functionalized with targeting ligands (e.g., antibodies, peptides) and loaded with chemotherapeutic drugs, creating an all-in-one system for cancer theranostics [68] [69]. The development of stimuli-responsive linkers that release drugs in response to tumor-specific cues (e.g., low pH, enzymatic activity) further enhances site-specific efficacy [69].
Nanoscaffolds for Regenerative Medicine
In tissue engineering, the objective shifts from mere drug delivery to creating a supportive microenvironment that guides tissue regeneration. Nanofibrous scaffolds, particularly those composed of chitosan, cellulose, and silk fibroin, mimic the native extracellular matrix (ECM) to promote cell adhesion, proliferation, and differentiation [68] [72]. For instance, sprayable peptide amphiphile nanofibers self-assemble into scaffolds at the wound site, delivering cells, drugs, and growth factors directly to accelerate tissue repair [73]. The incorporation of bioactive ingredients (e.g., Rutin) within hyaluronic acid-based nanoparticles has shown significant vasculo-protective effects, countering anthracycline-induced endothelial damage and highlighting their regenerative potential [71].
Experimental Protocols
Protocol 1: Formulation and Characterization of Transferrin-Targeted Albumin Nanoparticles
This protocol details the synthesis and characterization of human serum albumin (HSA) nanoparticles conjugated with transferrin (Tf) for enhanced blood-brain barrier penetration, based on methodologies with demonstrated efficacy in vitro [70].
Materials and Reagents
- Human Serum Albumin (HSA)
- Transferrin (Tf)
- 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) / N-Hydroxysuccinimide (NHS)
- Absolute Ethanol
- Glutaraldehyde (8% w/v)
- Phosphate Buffered Saline (PBS), pH 7.4
- Purified water
Synthesis Procedure
- Desolvation for HSA Nanoparticle Core:
- Dissolve 100 mg of HSA in 1 mL of purified water under constant magnetic stirring (500 rpm).
- Gradually add 4 mL of absolute ethanol at a rate of 1 mL/min using a syringe pump. The solution will become opalescent, indicating nanoparticle formation.
- Crosslink the formed nanoparticles by adding 50 µL of 8% glutaraldehyde and stir for 12 hours at room temperature.
- Transferrin Conjugation:
- Activate carboxyl groups on the purified HSA nanoparticles using EDC (50 mM) and NHS (25 mM) in MES buffer (pH 6.0) for 15 minutes.
- Purify the activated nanoparticles via centrifugation (15,000 rpm, 20 minutes) and resuspend in PBS (pH 7.4).
- Incubate with Transferrin (10 mg/mL in PBS) for 2 hours at room temperature under gentle agitation.
- Purify the final HSA-Tf nanoparticles by centrifugation (15,000 rpm, 20 minutes) three times to remove unconjugated Tf.
Characterization and Quality Control
Critical quality attributes must be assessed to ensure batch-to-batch reproducibility and performance.
Table 2: Characterization Parameters for HSA-Tf Nanoparticles
| Parameter | Target Specification | Analytical Method | Purpose |
|---|---|---|---|
| Particle Size | 150 - 200 nm | Dynamic Light Scattering (DLS) | Influences BBB penetration and biodistribution [70] |
| Polydispersity Index (PDI) | < 0.2 | DLS | Indicates narrow size distribution and formulation homogeneity [70] |
| Zeta Potential | < -20 mV | Laser Doppler Velocimetry | Predicts colloidal stability; high negative charge prevents aggregation |
| Transferrin Conjugation Efficiency | > 80% | BCA Protein Assay (supernatant) | Quantifies successful ligand attachment for targeted delivery [70] |
| Drug Loading Capacity | > 8% w/w | HPLC/UV-Vis after dissolution | Measures efficiency of active ingredient incorporation |
Protocol 2: In Vitro Assessment of BBB Transcytosis
This protocol describes a co-culture model to evaluate the transcytosis potential of developed nanocarriers across a simulated blood-brain barrier.
Materials and Reagents
- Primary Human Brain Microvascular Endothelial Cells (hBMECs)
- Primary Human Astrocytes (hASTROs)
- Primary Human Brain Vascular Pericytes (hBVPs)
- Transwell inserts (3.0 µm pore size)
- Fluorescently-labeled nanoparticles (e.g., Coumarin-6 tagged)
- Cell culture media specific for each cell type
- Confocal microscopy imaging setup
Experimental Setup
- BBB Co-culture Model Establishment:
- Culture hBVPs on the bottom of the Transwell plate. Culture hASTROs on the underside of the Transwell membrane.
- Seed hBMECs on the apical side of the Transwell membrane to create a tri-culture BBB model. Allow the model to mature for 5-7 days until transendothelial electrical resistance (TEER) values stabilize above 150 Ω·cm².
- Transcytosis Assay:
- Apply fluorescent nanoparticles (at a non-toxic dose of 31.25 µg/mL, as established [70]) in serum-free media to the apical (donor) compartment.
- Incubate at 37°C for 3 hours.
- Collect media from the basolateral (receiver) compartment at predetermined time points.
- Quantify the amount of translocated nanoparticles using fluorescence spectroscopy or HPLC.
- Cellular Uptake and Imaging:
- After the assay, wash the Transwell membranes with PBS and fix the cells with 4% paraformaldehyde.
- Stain the cellular actin cytoskeleton (e.g., with Phalloidin) and nuclei (e.g., with DAPI).
- Image using confocal microscopy to visualize the internalization and distribution of nanoparticles within the different cell types of the BBB.
Data Analysis
- Apparent Permeability (Papp): Calculate using the formula: Papp = (dQ/dt) / (A × C₀), where dQ/dt is the transport rate, A is the membrane surface area, and C₀ is the initial donor concentration.
- Cellular Uptake: Quantify fluorescence intensity per cell using image analysis software to compare uptake efficiency between different NP formulations.
Pathway and Workflow Visualizations
Nanoparticle Synthesis and BBB Transcytosis Workflow
Mechanism of Targeted NP Transport Across the BBB
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Nanocarrier Development and Evaluation
| Reagent / Material | Function / Application | Research Context |
|---|---|---|
| Poly(Lactide-co-Glycolide) (PLGA) | Biodegradable polymer for nanoparticle core; enables sustained drug release [70]. | Primary polymeric carrier for CNS drug delivery studies; enhances BBB penetration in vitro/in vivo [70]. |
| Human Serum Albumin (HSA) | Protein-based nanoparticle core; biocompatible, biodegradable, and amenable to surface functionalization [70]. | Used for formulating targeted NPs (e.g., HSA-Tf) for brain delivery; shows enhanced uptake in hBMECs [70]. |
| Transferrin (Tf) | Targeting ligand for the transferrin receptor, highly expressed on the BBB [70]. | Conjugated to NP surface (e.g., Albumin, PLGA) to exploit receptor-mediated transcytosis for CNS delivery [70]. |
| DSPE-PEG(2000)-Carboxylic Acid | PEGylated lipid for surface functionalization; confers "stealth" properties and provides a chemical handle for conjugation [69]. | Used in liposomal and lipid NP formulations to prolong circulation half-life and reduce MPS uptake [69]. |
| EDC / NHS Crosslinkers | Carbodiimide chemistry agents for activating carboxyl groups for covalent conjugation with amine groups [70]. | Standard method for conjugating targeting ligands (e.g., antibodies, peptides, Tf) to nanocarrier surfaces [70]. |
| Primary hBMECs, Pericytes, Astrocytes | Cellular components for constructing a physiologically relevant in vitro Blood-Brain Barrier model [70]. | Critical for evaluating NP interaction, uptake, and transcytosis in a human-cell-based system before animal studies [70]. |
| Coumarin-6 | Lipophilic fluorescent dye used for tracking and quantifying nanoparticle uptake and localization. | Incorporated into NP matrix during synthesis for visualization via confocal microscopy and quantification via fluorescence [70]. |
Bridging the Translational Gap: Overcoming Manufacturing and Toxicity Hurdles
The translational bottleneck represents one of the most significant challenges in modern drug development, particularly in the field of nanotechnology-based targeted drug delivery systems. This phenomenon describes the critical attrition point where promising preclinical research fails to transition successfully into clinical applications. Despite remarkable advances in basic science and preclinical research, a troubling chasm persists between laboratory promise and clinical utility, creating a major roadblock in therapeutic development [74].
In the specific context of nanomedicine, this translational gap is particularly pronounced. While nanotechnology enables the design of sophisticated nanostructures to improve drug delivery by modulating release, enhancing solubility, and increasing bioavailability of poorly soluble active pharmaceutical ingredients (APIs), only a minute fraction of these systems reaches clinical application. Analysis reveals that of the thousands of nanomedicines published in scientific literature, only an estimated 50-80 have achieved global regulatory approval by 2025, representing a conversion rate of less than 0.1% from laboratory to clinic [7]. This discrepancy highlights the critical need to identify the root causes of this bottleneck and develop strategic approaches to overcome these hurdles.
Quantitative Analysis of the Translational Gap
The magnitude of the translational challenge is evident when examining success rates and associated costs across the drug development pipeline. The following table summarizes key quantitative indicators of the translational bottleneck:
Table 1: Quantitative Indicators of the Translational Bottleneck in Drug Development
| Metric | Value | Context/Implication |
|---|---|---|
| Overall Drug Development Success Rate | 0.1% | Only 0.1% of drugs entering preclinical research gain FDA approval [75] |
| Preclinical to Clinical Transition Failure | 80-90% | 80-90% of research projects fail before human testing [75] |
| Clinical Trial Failure Rate | ~95% | Approximately 95% of drugs entering human trials fail [75] |
| Phase III Clinical Trial Failure | ~50% | Nearly half of all experimental drugs fail in Phase III trials [75] |
| Nanomedicine Translation Rate | <0.1% | Less than 0.1% of published nanomedicines reach clinical use [7] |
| Development Cost per Approved Drug | ~$2.6 billion | Represents a 145% cost increase (inflation-adjusted) since 2003 [75] |
| Published Cancer Biomarkers in Clinical Practice | <1% | Less than 1% of published cancer biomarkers enter clinical practice [74] |
The financial implications of these failures are substantial, with the development cost for each newly approved drug estimated at approximately $2.6 billion, representing a 145% increase (inflation-adjusted) over estimates from 2003 [75]. This combination of high attrition rates and escalating costs creates a significant barrier to innovation, particularly in complex fields like targeted drug delivery systems.
Root Causes of Translational Failure in Targeted Drug Delivery
Biological Barriers
The biological complexity of human diseases presents fundamental challenges for nanomedicine translation. The blood-brain barrier (BBB) exemplifies this challenge, particularly for neurological applications. The BBB's selective interface restricts the entry of most therapeutic agents into the brain, with its unique cellular composition and tight junctions maintaining brain homeostasis while limiting drug delivery [22]. This challenge is amplified in conditions like Alzheimer's disease, where BBB integrity varies during disease progression, further complicating treatment timing and efficacy [22].
The tumor microenvironment presents similar challenges in oncology applications. The Enhanced Permeability and Retention (EPR) effect, while often robust in mouse models, demonstrates significant heterogeneity and limitation in human tumors. Factors including vascular heterogeneity, interstitial pressure, and non-EPR entry routes complicate in vivo distribution predictions and require strategies beyond passive EPR reliance to achieve consistent targeting [7]. This translational discrepancy is exemplified by the failure of BIND-014 (targeted docetaxel nanoparticles), which demonstrated favorable preclinical safety and early activity but failed to meet primary efficacy endpoints in Phase II trials, leading to program termination [7].
Model System Limitations
A primary contributor to translational failure lies in the inadequate predictive value of preclinical models. Traditional animal models, including syngeneic mouse models, do not fully recapitulate all aspects of human clinical disease, resulting in treatment responses that poorly predict clinical outcomes [74]. This model disparity is particularly problematic in biomarker validation, where less than 1% of published cancer biomarkers actually enter clinical practice [74].
The problem extends beyond biological relevance to methodological approaches. Preclinical studies typically rely on controlled conditions to ensure clear and reproducible results. However, human diseases like cancer are highly heterogeneous and constantly evolving, varying not just between patients but within individual tumors. Genetic diversity, varying treatment histories, comorbidities, progressive disease stages, and the highly variable nature of tumor microenvironments introduce real-world variables that cannot be fully replicated in controlled preclinical settings [74].
Technical and Manufacturing Challenges
The transition from laboratory-scale production to Good Manufacturing Practice (GMP) scale introduces significant hurdles for nanomedicine translation. The Chemistry, Manufacturing, and Controls (CMC) requirements for nanomedicines present unique challenges, as GMP-scale production requires thorough characterization and stringent process control to ensure inter-batch consistency [7]. This challenge is particularly acute for complex polymer-based platforms, where chemical diversity often leads to significant batch-to-batch variability and scaling difficulties under GMP standards [7].
Additionally, characterization challenges emerge as nanoparticle properties—including size, charge, and amphiphilicity—determine transport efficiency and uptake routes, which may vary with disease progression [22]. The lack of uniformity in toxicity and immune response testing standards further complicates translational efforts, creating regulatory uncertainty and validation challenges [7].
Strategic Framework for Enhancing Translational Success
Advanced Model Systems
Bridging the translational gap requires the implementation of more predictive model systems that better recapitulate human disease biology. The following advanced platforms represent significant improvements over traditional models:
Patient-Derived Xenografts (PDX): These models, derived from patient tumor tissue implanted into immunodeficient mice, more effectively recapitulate the characteristics of human cancer, including tumor progression and evolution. PDX models have demonstrated superior accuracy for biomarker validation compared to conventional cell line-based models and have played key roles in investigating HER2 and BRAF biomarkers [74].
Organoid and 3D Co-culture Systems: Organoids are 3D structures that recapitulate the identity of the organ or tissue being modeled, particularly retaining characteristic biomarker expression better than two-dimensional culture models. These systems have been used to effectively predict therapeutic responses and guide personalized treatment selection. Three-dimensional co-culture systems that incorporate multiple cell types (including immune, stromal, and endothelial cells) provide comprehensive models of the human tissue microenvironment, enabling more physiologically accurate cellular interactions [74].
Organ-on-a-Chip Technologies: These microfluidic devices simulate organ-level physiology and human microenvironments, offering more predictable tools for in vitro evaluation. For instance, liver-on-a-chip 3D models have been developed to evaluate hepatic toxicity and metabolic profiles of drug candidates, providing more human-relevant data than traditional animal studies [76].
Integrated Formulation Strategies
Shifting from nanoparticle design alone to integrated formulation strategies is fundamental to accelerating nanomedicine translation. This approach encompasses fundamental decisions in core particle design, surface engineering, and integration into final dosage forms suitable for clinical administration. The following table outlines key formulation platforms and their translational considerations:
Table 2: Advanced Formulation Platforms for Nanomedicine Translation
| Platform | Key Advantages | Translational Challenges | Clinical Examples |
|---|---|---|---|
| Lipid-Based Systems (Liposomes, LNPs) | Superior pharmacokinetic control; Mature regulatory track record; Versatile payload encapsulation | Heterogeneous EPR in humans; Risk of immunogenicity (anti-PEG antibodies); Formulation stability during storage | Doxil (liposomal doxorubicin); COVID-19 mRNA vaccines [7] [76] |
| Polymer-Based Systems (PLGA, micelles) | Controlled release profiles; Reliable biodegradation; Unparalleled chemical flexibility | Batch-to-batch variability; Scaling challenges under GMP; Weak in vitro-in vivo correlation | Experimental paclitaxel formulations [7] |
| Inorganic Nanoparticles (Mesoporous silica, metal NPs) | Tailorable surface functionality; Enhanced cellular uptake; Potential for theranostics | Long-term toxicity concerns; Biopersistence issues; Complex characterization requirements | Mesoporous silica nanoparticles for cancer therapy [71] |
| Hybrid Systems | Combination of advantages from multiple platforms; Enhanced functionality | Increased manufacturing complexity; Regulatory uncertainty for novel combinations | Chitosan-coated lipid microvesicles [71] |
Data-Driven and AI-Enhanced Approaches
Artificial intelligence (AI) and machine learning (ML) are revolutionizing biomarker discovery and nanomedicine design by identifying patterns in large datasets that cannot be detected using traditional methods. These technologies enable several critical applications:
Translational Outcome Prediction: AI models can be trained on historical compound performance data (including both positive and negative results) to predict clinical success likelihood, enabling better candidate selection and resource allocation [77].
Model Fidelity Assessment: Machine learning algorithms can compare mouse-human molecular profiles (e.g., transcriptomics, metabolomics, proteomics) to evaluate how closely preclinical models mimic human disease biology [77].
Digital Twin Development: Creating computational analogs of animal models or patients enables in silico testing of treatment sequences and resistance mechanisms, potentially reducing the need for extensive animal studies [77].
The successful implementation of AI approaches requires access to large, high-quality datasets that include comprehensive characterization from multiple sources. This necessitates collaboration between AI researchers, clinicians, and regulatory agencies to establish robust validation frameworks [74].
Experimental Protocols for Enhanced Translational Predictivity
Protocol: Clinically-Aligned Efficacy Assessment in Preclinical Models
Background: Traditional preclinical endpoints like percentage tumor growth inhibition (%TGI) fail to reflect how oncologists assess response in patients using RECIST 1.1 criteria. Implementing clinically-aligned metrics enhances comparability between preclinical and clinical outcomes [77].
Materials:
- Animal cancer models (PDX, orthotopic, or humanized mice)
- Tumor volume measurement tools (calipers, ultrasound, MRI)
- Data recording system with longitudinal tracking capability
Procedure:
- Baseline Assessment: Establish baseline tumor measurements before treatment initiation
- Dosing Regimen: Administer test articles using clinically relevant routes and schedules
- Longitudinal Monitoring: Track tumor volumes at least twice weekly throughout study
- Response Categorization: Apply modified RECIST criteria:
- Complete Response (CR): Disappearance of measurable tumor
- Partial Response (PR): ≥50% reduction in tumor volume from baseline
- Stable Disease (SD): Neither sufficient shrinkage to qualify PR nor increase to qualify PD
- Progressive Disease (PD): ≥20% increase in tumor volume or emergence of new lesions
- Durability Assessment: Monitor for tumor regrowth following treatment cessation
- Tumor-Free Survival (TFS) Calculation: Determine duration of complete remission
Validation: Compare response distributions across treatment groups using appropriate statistical methods (e.g., Fisher's exact test for categorical responses)
Protocol: Multi-Omics Model Characterization for Translational Alignment
Background: Comprehensive model characterization using multi-omics approaches identifies context-specific, clinically actionable biomarkers that may be missed with single-platform approaches [74].
Materials:
- Tissue samples from preclinical models and human reference datasets (e.g., TCGA)
- RNA/DNA extraction kits
- Proteomic analysis platform (mass spectrometry)
- Bioinformatics tools for data integration
Procedure:
- Sample Collection: Obtain representative tissue samples from model systems under controlled conditions
- Genomic Profiling: Conduct whole exome or targeted sequencing to identify genetic alterations
- Transcriptomic Analysis: Perform RNA sequencing to characterize gene expression patterns
- Proteomic Characterization: Analyze protein expression and post-translational modifications
- Data Integration: Use bioinformatic approaches to integrate multi-omics datasets
- Cross-Species Comparison: Compare molecular profiles between model systems and human reference data
- Biomarker Identification: Identify conserved pathways and potential predictive biomarkers
Validation: Confirm identified biomarkers using orthogonal methods (e.g., immunohistochemistry, RT-PCR) in independent sample sets
Visualization of Translational Workflows
Integrated Translational Research Framework
Integrated Translational Research Framework
Nanomedicine Translation Pathway
Nanomedicine Translation Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Translational Nanomedicine Research
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Patient-Derived Xenograft (PDX) Models | Recapitulate human tumor characteristics and heterogeneity for more predictive efficacy testing | Maintain molecular features of original tumors; Require immunodeficient hosts [74] |
| Organoid Culture Systems | 3D models that retain tissue-specific architecture and biomarker expression for personalized medicine approaches | Preserve characteristic biomarker expression better than 2D models [74] |
| Ionizable Lipids | Key component of lipid nanoparticles for nucleic acid delivery; Enable endosomal escape and payload release | Critical for mRNA vaccine success; Composition affects reactogenicity and efficacy [7] [71] |
| PEGylated Lipids | Surface modification to enhance circulation time by reducing reticuloendothelial system clearance | Risk of immunogenicity with anti-PEG antibodies; Requires consideration of alternatives [7] |
| Targeting Ligands | Surface functionalization to achieve active targeting to specific tissues or cell types | Includes peptides, antibodies, aptamers; Must balance targeting with opsonization risk [22] |
| Multi-Omics Profiling Platforms | Integrated genomic, transcriptomic, proteomic analysis for comprehensive biomarker identification | Enables identification of context-specific, clinically actionable biomarkers [74] |
| Microfluidic Organ-on-Chip Devices | Human-relevant in vitro models for predictive toxicity and efficacy testing | Simulate organ-level physiology; Reduce animal model reliance [76] |
Overcoming the translational bottleneck in targeted drug delivery systems requires a fundamental shift from traditional research practices to a data-integrated paradigm that is biologically informed and clinically relevant. By adopting clinically-aligned efficacy metrics, deploying AI to model translational risk, and embracing systems-level biology, researchers can design smarter experiments that better reflect human disease complexity.
The integration of advanced model systems, strategic formulation approaches, and predictive analytics represents the most promising path forward for enhancing nanomedicine translation. This multifaceted strategy will not only reduce attrition but also accelerate the journey of effective therapies from bench to bedside, ultimately benefiting the patients who need them most.
Future success will depend on continued collaboration across disciplines and sectors, with shared commitment to addressing the fundamental biological, technical, and methodological challenges that currently limit translational success in targeted drug delivery systems.
The translation of nanomedicines from promising laboratory discoveries to commercially available therapeutics represents a critical hurdle in the field of targeted drug delivery. Despite intensive research efforts and the compelling advantages that nanoparticles offer over their bulk counterparts, fewer than 100 nanomedicines have been approved by the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) since 1989 [78]. This disparity highlights a substantial gap in translational research, reflecting the disconnect between prolific academic research and the limited number of products that successfully reach and sustain themselves in the market. The discontinuation of DepoCyt, an FDA-approved nanomedicine for lymphomatous meningitis, in 2017 due to persistent manufacturing issues underscores the critical importance of robust, scalable production processes [78].
The successful translation of a pharmaceutical drug delivery system depends on its manufacturing feasibility in a quality-controlled Good Manufacturing Practice (GMP) environment at larger scales while preserving critical physicochemical properties during scale-up [79]. Problems arising during scale-up and issues related to regulatory compliance represent the most common challenges for nanomedicine manufacturing [79]. This application note addresses these challenges by providing a structured framework integrating Quality-by-Design (QbD), advanced process control technologies, and GMP principles to advance nanomedicine development.
Quality-by-Design Framework for Nanomedicine Development
QbD Principles and Implementation
The QbD approach represents a systematic, risk-based framework for pharmaceutical development that emphasizes product and process understanding based on sound science and quality risk management [78]. For nanomedicines, QbD implementation begins with defining a Quality Target Product Profile (QTPP) that outlines the desired quality characteristics of the final product. Critical Quality Attributes (CQAs) are then identified as physical, chemical, biological, or microbiological properties that must be controlled within predetermined limits to ensure the final product achieves its QTPP [78].
The QbD framework for nanomedicines depends heavily on Process Analytical Technologies (PATs) to systematically evaluate and regulate production processes [1]. This system enables manufacturers to monitor and control production in real-time to maintain consistent quality and performance standards. Key elements of QbD implementation include:
- Identification of Critical Material Attributes (CMAs) and Critical Process Parameters (CPPs) that significantly impact CQAs [78]
- Establishment of a Design Space where process parameters can be varied without affecting product quality
- Implementation of Control Strategies to ensure consistent product quality throughout scaling
- Continuous Monitoring and Improvement based on process data and product performance
Critical Quality Attributes for Nanomedicines
For nanomedicine products, CQAs typically include parameters such as particle size, size distribution (polydispersity index), zeta potential, drug loading efficiency, encapsulation efficiency, and surface characteristics [80]. These attributes significantly influence the biological behavior, including biodistribution, targeting efficiency, and clearance pathways [80]. The table below summarizes key CQAs and their critical ranges for various nanomedicine types.
Table 1: Critical Quality Attributes (CQAs) for Different Nanomedicine Platforms
| Nanoparticle Type | Size Range (nm) | PDI Limit | Zeta Potential (mV) | Drug Loading Efficiency | Key CQAs | ||
|---|---|---|---|---|---|---|---|
| Liposomes | 80-150 | <0.2 | -30 to -50 | >85% | Lamellarity, phase transition temperature, phospholipid purity | ||
| Polymeric NPs (PLGA) | 100-200 | <0.2 | -20 to -40 | >70% | Molecular weight, lactide:glycolide ratio, residual solvent | ||
| Solid Lipid NPs | 50-200 | <0.25 | > | ±20 | >80% | Crystallinity, polymorphic transitions, lipid composition | |
| Inorganic NPs | 20-100 | <0.15 | Variable | N/A | Crystal structure, surface chemistry, coating uniformity | ||
| Lipid Nanoparticles (LNPs) | 75-90 | <0.2 | ~-2 to -5 | >95% | Ionizable lipid content, PEG-lipid percentage, pKa |
Scalable Manufacturing Technologies for Nanomedicines
Comparative Analysis of Production Methods
Scaling up the production of nanomedicine systems is critical for the successful translation of personalized medicine into clinical practice [81]. A detailed comparative analysis of production methods reveals significant differences in their scalability, cost implications, and impact on nanoparticle characteristics such as size and reproducibility [81]. The selection of an appropriate manufacturing technology must consider both the initial research and development phase and the long-term commercial production requirements.
Table 2: Scalability Assessment of Nanomedicine Manufacturing Technologies
| Manufacturing Method | Scalability | Batch-to-Batch Consistency | Cost Implications | Key Challenges | Suitable Nanocarriers |
|---|---|---|---|---|---|
| Microfluidics | Moderate to High | High | Moderate to High | Clogging, throughput limitations | Liposomes, LNPs, polymeric NPs |
| Supercritical Fluid Technology | High | High | High | High capital investment, process complexity | PLGA NPs, nanocrystals, liposomes |
| Extrusion | High | Moderate to High | Low to Moderate | Membrane integrity, shear stress | Liposomes, solid lipid NPs |
| Nanocrystallization | Moderate | Moderate | Moderate | Crystal growth control, stability | Poorly soluble drug nanocrystals |
| Solvent Evaporation | Moderate | Moderate | Moderate | Residual solvent removal, stability | Polymeric NPs, nanocapsules |
Protocol: Microfluidics-Based Production of Lipid Nanoparticles
Principle: Microfluidics enables precise control over nanoparticle formation through rapid mixing of fluid streams in microscale channels, allowing reproducible production of lipid nanoparticles (LNPs) with narrow size distribution [81] [82].
Materials:
- Lipid Mixture: Ionizable lipid (e.g., DLin-MC3-DMA), DSPC, cholesterol, DMG-PEG2000
- Aqueous Phase: mRNA in citrate buffer (pH 4.0)
- Equipment: Microfluidic mixer (e.g., NanoAssemblr), syringe pumps, temperature control unit
- Buffers: Phosphate-buffered saline (PBS, pH 7.4), tromethamine (Tris) buffer
Procedure:
- Lipid Solution Preparation: Prepare ethanol phase containing ionizable lipid, DSPC, cholesterol, and PEG-lipid at molar ratio 50:10:38.5:1.5 with total lipid concentration 12.5 mM in absolute ethanol.
- Aqueous Phase Preparation: Dilute mRNA in 50 mM citrate buffer (pH 4.0) to concentration of 0.2 mg/mL.
- System Setup: Connect syringes containing lipid and aqueous phases to microfluidic mixer using appropriate tubing. Set temperature control to 25°C.
- Mixing Process: Set total flow rate (TFR) to 12 mL/min with aqueous-to-organic flow rate ratio (FRR) of 3:1.
- Collection: Collect resulting nanoparticles in vessel containing 5 volumes of 50 mM Tris buffer (pH 7.4) to neutralize pH and stabilize particles.
- Dialyzation: Dialyze against PBS (pH 7.4) for 4 hours using 100 kDa molecular weight cutoff membrane to remove ethanol and exchange buffer.
- Characterization: Analyze particle size by dynamic light scattering, encapsulation efficiency by Ribogreen assay, and morphology by transmission electron microscopy.
Critical Process Parameters:
- Total flow rate (TFR): 8-16 mL/min
- Flow rate ratio (FRR): 2:1 to 4:1 (aqueous:organic)
- Total lipid concentration: 10-15 mM
- mRNA concentration in aqueous phase: 0.1-0.3 mg/mL
- Temperature: 20-30°C
Diagram 1: Microfluidics-based LNP Production Workflow
Protocol: Supercritical Fluid Technology for Polymeric Nanoparticles
Principle: Supercritical fluid technology, particularly supercritical carbon dioxide (SC-CO2), serves as an anti-solvent for polymer precipitation, enabling organic solvent-free production of nanoparticles with high purity [81] [79].
Materials:
- Polymer Solution: PLGA (50:50) in dichloromethane or acetone (10-20 mg/mL)
- Drug Compound: Therapeutic agent (e.g., paclitaxel, docetaxel)
- Supercritical Fluid System: CO2 cylinder, cooling bath, high-pressure pump, precipitation vessel
- Stabilizers: Polyvinyl alcohol (PVA), polysorbate 80, or other stabilizers as needed
Procedure:
- Polymer/Drug Solution: Dissolve PLGA and drug in organic solvent at concentration 15 mg/mL with drug loading 10-20% (w/w).
- System Preparation: Pre-equilibrate supercritical fluid system to desired temperature (35-45°C) and pressure (80-150 bar).
- Solution Introduction: Pump polymer/drug solution into precipitation vessel through nozzle at flow rate 1-2 mL/min.
- Anti-Solvent Process: Simultaneously introduce SC-CO2 at flow rate 10-20 g/min to expand solvent and precipitate nanoparticles.
- Washing: Maintain SC-CO2 flow for 30-60 minutes to remove residual organic solvent.
- Depressurization: Slowly depressurize system at rate 5-10 bar/min to atmospheric pressure.
- Collection: Collect nanoparticles from precipitation vessel and suspend in appropriate aqueous buffer containing stabilizer.
- Lyophilization: Freeze-dry nanoparticles with cryoprotectant (e.g., trehalose, sucrose) for long-term storage.
Critical Process Parameters:
- Temperature: 35-45°C
- Pressure: 80-150 bar
- Polymer concentration: 10-20 mg/mL
- Solution flow rate: 1-2 mL/min
- CO2 flow rate: 10-20 g/min
- Nozzle diameter: 100-200 μm
GMP Compliance and Regulatory Considerations
Good Manufacturing Practice Implementation
The implementation of GMP for nanomedicines requires careful consideration of their unique characteristics compared to conventional pharmaceuticals. Manufacturing methods must be easily adaptable to existing facilities and equipment to enable larger production volumes with less energy and material consumption while maintaining stringent control of product quality and safety [79]. Key elements of GMP compliance for nanomedicines include:
- Facility Design: Appropriate classification of cleanrooms with controlled environmental parameters
- Equipment Qualification: Installation qualification (IQ), operational qualification (OQ), and performance qualification (PQ) of specialized nanomanufacturing equipment
- Process Validation: Evidence that manufacturing process consistently produces product meeting predetermined quality attributes
- Quality Control Testing: Comprehensive characterization of nanomedicine CQAs using validated analytical methods
- Documentation: Complete and accurate batch records, standard operating procedures (SOPs), and change control protocols
The complex regulatory landscape, with regional differences in approval requirements from agencies, poses significant challenges for global manufacturers seeking to scale up production while maintaining compliance with diverse standards [81]. Close collaboration with regulatory agencies from the early stages of development is essential to ensure alignment and accelerate the development of future nanomedicines [80].
Analytical Methods for Characterization
Robust analytical methods are essential for GMP-compliant nanomedicine manufacturing. The table below outlines key characterization techniques and their applications in quality control.
Table 3: Essential Analytical Methods for Nanomedicine Characterization
| Analytical Method | Parameters Measured | Application in QC | Method Validation Requirements |
|---|---|---|---|
| Dynamic Light Scattering (DLS) | Hydrodynamic diameter, PDI | Batch release testing | Precision, accuracy, robustness, filter compatibility |
| HPLC with UV/FLD Detection | Drug loading, encapsulation efficiency, chemical stability | Identity, assay, purity | Specificity, linearity, range, accuracy, precision |
| Asymmetric Flow FFF-MALS | Size distribution, molecular weight | In-depth characterization | Method transfer from R&D to QC |
| TEM/SEM | Morphology, internal structure | Product understanding | Sample preparation standardization |
| DSC/XRD | Crystallinity, polymorphic form | Physical stability | Reference standard qualification |
| LC-MS/MS | Impurity profiling, degradation products | Stability indicating method | Specificity, sensitivity (LOQ) |
The Scientist's Toolkit: Research Reagent Solutions
Successful development and scaling of nanomedicines requires carefully selected reagents and materials that meet quality standards and ensure reproducible manufacturing.
Table 4: Essential Research Reagents for Nanomedicine Development
| Reagent Category | Specific Examples | Function | Quality Considerations |
|---|---|---|---|
| Ionizable Lipids | DLin-MC3-DMA, SM-102, ALC-0315 | LNP structure, mRNA encapsulation | Synthetic route, impurity profile, oxidation stability |
| Structural Lipids | DSPC, DPPC, cholesterol | Bilayer stability, rigidity | Phase transition temperature, purity (>99%) |
| PEGylated Lipids | DMG-PEG2000, DSG-PEG2000 | Steric stabilization, circulation time | PEG molecular weight distribution, critical micelle concentration |
| Biodegradable Polymers | PLGA, PLA, PCL | Nanoparticle matrix, controlled release | Lactide:glycolide ratio, molecular weight, polydispersity, end groups |
| Surface Ligands | Peptides, antibodies, aptamers | Active targeting | Conjugation efficiency, binding affinity, orientation |
| Stabilizers/Surfactants | Poloxamer 188, polysorbate 80, PVA | Physical stability, prevention of aggregation | Grade (pharmaceutical vs. laboratory), batch variability |
| Cryoprotectants | Trehalose, sucrose, mannitol | Lyophilization stability | Crystallinity, residual moisture, collapse temperature |
Scale-Up Strategy and Technology Transfer
The transition from laboratory-scale to commercial production represents one of the most challenging aspects of nanomedicine development. A systematic scale-up strategy should be implemented, considering both process parameters and equipment changes.
Diagram 2: Scale-Up Strategy and Critical Decision Points
Critical considerations for successful scale-up include:
- Geometric Similarity: Maintaining similar geometry and flow patterns between different scales
- Dynamic Similarity: Conserving key dimensionless numbers (e.g., Reynolds number for mixing)
- Kinetic Similarity: Ensuring equivalent process kinetics (e.g., mixing time, precipitation rate)
- Raw Material Consistency: Sourcing materials from qualified suppliers with consistent quality
- Process Modeling: Utilizing computational approaches to predict performance at larger scales
The successful scaling of nanomedicine manufacturing requires an integrated approach combining QbD principles, advanced process technologies, and rigorous GMP compliance. The implementation of systematic strategies for process understanding and control enables the translation of promising nanomedicines from laboratory research to commercial products that can benefit patients.
Future developments in nanomedicine manufacturing will likely focus on continuous manufacturing approaches, advanced PAT for real-time release testing, and the integration of artificial intelligence for process optimization [1]. Additionally, the growing emphasis on personalized medicine will drive the development of flexible manufacturing platforms capable of producing patient-specific nanomedicines with appropriate quality attributes.
By addressing the technical and regulatory hurdles through systematic application of QbD, process control, and GMP, nanomedicines hold the potential to revolutionize personalized medicine with more effective, targeted therapies for complex diseases [81]. The frameworks and protocols presented in this application note provide a foundation for researchers and drug development professionals to advance their nanomedicine programs toward successful clinical translation and commercialization.
The application of nanotechnology in targeted drug delivery systems represents a paradigm shift in modern therapeutics, offering enhanced bioavailability, improved targeting specificity, and reduced side effects [82]. However, the very properties that make nanoparticles (NPs) therapeutically advantageous—their small size, large surface area-to-volume ratio, and high reactivity—also contribute to potential toxicological concerns [83] [84]. A comprehensive understanding of nanotoxicity mechanisms is therefore essential for the safe and effective translation of nanomedicines into clinical practice, particularly within the context of a broader thesis on applying nanotechnology in targeted drug delivery systems research.
This document provides detailed application notes and experimental protocols for evaluating the immunological responses, oxidative stress, and long-term safety concerns associated with nanoparticle exposure. By establishing standardized assessment methodologies, researchers can better characterize nanomaterial safety profiles and develop strategies to mitigate adverse effects.
Mechanisms of Nanotoxicity: Application Notes
Oxidative Stress Pathways
The generation of reactive oxygen species (ROS) is considered the foremost mechanism of nanotoxicity [83] [85]. While cells can typically tolerate small, transient increases in ROS, sustained elevated levels result in oxidative stress that can damage cellular macromolecules.
Key Mechanistic Insights:
- ROS Generation: Multiple nanoparticle types, especially metal- and carbon-based NPs, induce significant ROS overproduction [83] [85]. This occurs through Fenton-type reactions (metal oxides), mitochondrial disruption, or activation of inflammatory cells.
- Cellular Consequences: Elevated ROS levels interact with functional proteins and DNA, disrupting signal transduction and causing dysfunction [85]. This leads to unregulated cell signaling, altered cell motility, DNA damage, and ultimately autophagy, apoptosis, necrosis, fibrosis, or carcinogenesis [85].
- Transcription Factor Activation: ROS induction activates redox-sensitive transcription factors, particularly nuclear factor-kappa B (NF-κB), which upregulates pro-inflammatory genes including tumor necrosis factor-α (TNF-α) and interleukins (IL-1, IL-6, IL-8) [83].
Table 1: Nanoparticle Properties Influencing Oxidative Stress Potential
| Property | Impact on Oxidative Stress | Representative NPs |
|---|---|---|
| Size | Smaller particles (<30 nm) exhibit higher ROS generation due to increased surface area | Quantum dots, Ultra-small IONPs |
| Chemical Composition | Metal ions can catalyze Fenton reactions; semiconductor materials generate electron-hole pairs | Fe₃O₄, TiO₂, CdSe |
| Surface Charge | Cationic surfaces show higher ROS production than anionic or neutral surfaces | Aminated polystyrene NPs |
| Solubility/Degradation | Degradable NPs may release toxic ions that enhance ROS (e.g., Cd²⁺ from QDs, Fe²⁺ from IONPs) | Quantum dots, Iron oxide NPs |
Immunological Responses
Nanoparticle exposure often triggers immune perturbation, ranging from elevated to suppressed immune responses, depending on NP characteristics [85]. The immune toxicity of nanoparticles is closely linked to ROS generation and subsequent inflammatory pathway activation.
Key Mechanistic Insights:
- Inflammasome Activation: Mitochondrial ROS production triggers the activation of inflammasomes in phagocytic cells, leading to the maturation and secretion of pro-inflammatory cytokines like IL-1β and IL-18 [85].
- Cytokine Release: Exposure to nanoparticles elevates various pro-inflammatory cytokines (TNF-α, IL-1, IL-6, IL-8), resulting in induced apoptosis and autophagy [83] [85].
- Complement Activation: Lipid-based nanoparticles can activate the complement cascade, potentially leading to hypersensitivity reactions and anaphylaxis [85]. This has particular relevance for the safety of lipid nanoparticle (LNP) formulations used in mRNA vaccines and therapies.
Table 2: Immunological Responses to Select Nanoparticle Types
| Nanoparticle Type | Primary Immune Response | Key Mediators | Potential Consequences |
|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Complement activation; Inflammatory cytokine secretion | IL-8, TNF-α, MCP-1 [82] | Hypersensitivity reactions; Reactogenicity |
| Carbon Nanotubes | Persistent inflammation; Granuloma formation | TNF-α, IL-1β, TGF-β [83] | Pulmonary fibrosis; Chronic inflammation |
| Silver Nanoparticles (AgNP) | Immunosuppression; Cytokine modulation | Reduced IL-6, TNF-α in some models | Increased infection susceptibility |
| Iron Oxide NPs (IONPs) | Oxidative stress in tissues; Chronic inflammation | ROS, ALT, AST elevation [86] | Multi-organ toxicity |
Long-Term Safety and Accumulation Concerns
The degradability of nanoparticles significantly influences their long-term safety profile. Some nanomaterials are non-degradable or slow to degrade, accumulating in organs and cells with potential for unknown long-term toxic effects [85].
Key Mechanistic Insights:
- Organ Accumulation: Studies reveal that intraperitoneally injected TiO₂ nanoparticles (20 mg/kg every two days for 20 days) accumulate in the liver, lung, and brain, with observed increases in aspartate aminotransferase/alanine aminotransferase ratio (AST/ALT) and abnormal neuro-behavioral performance [83].
- Protein Corona Formation: Surface charges on nanoparticles facilitate binding with serum enzymes, forming a "protein corona" that affects enzymatic regulatory mechanisms and alters nanoparticle biodistribution [85] [87].
- Intracellular Destabilization: The acidic environment of endosomes (pH~6) and lysosomes (pH~4.5) can destabilize nanoparticles, leading to coating loss and toxic ion release [85]. For example, iron oxide nanoparticles undergo acid etching in endosomes, generating free ions that impact cell homeostasis [85].
Experimental Protocols for Nanotoxicity Assessment
Protocol 1: In Vitro Assessment of Oxidative Stress
Objective: To quantify nanoparticle-induced reactive oxygen species (ROS) generation and oxidative stress in mammalian cell lines.
Materials:
- Research Reagent Solutions:
- DCFH-DA (2',7'-Dichlorofluorescin diacetate): Cell-permeable ROS-sensitive fluorescent probe
- N-Acetylcysteine (NAC): ROS scavenger for control experiments
- Cell culture medium appropriate for selected cell line
- PBS (Phosphate Buffered Saline), pH 7.4
- LDH (Lactate Dehydrogenase) assay kit for cytotoxicity assessment
- Specific fluorescent probes for superoxide (DHE) and mitochondrial ROS (MitoSOX)
Methodology:
- Cell Culture: Seed appropriate cell line (e.g., A549 lung epithelial cells, THP-1 monocytes, or primary macrophages) in 96-well black-walled plates at 1×10⁴ cells/well. Culture for 24 hours to achieve 70-80% confluence.
- Nanoparticle Preparation: Prepare nanoparticle suspensions in serum-free medium at 2× the highest test concentration. Sonicate using a water bath sonicator (30-60 seconds, 40-80 kHz) to ensure dispersion.
- DCFH-DA Loading: Replace medium with 100 µL of 10 µM DCFH-DA in serum-free medium. Incubate for 30 minutes at 37°C in the dark.
- Nanoparticle Exposure: Remove DCFH-DA solution, wash with PBS, and add 100 µL of nanoparticle suspensions across a concentration range (typically 1-100 µg/mL). Include positive control (e.g., 100 µM H₂O₂) and negative control (nanoparticle-free medium).
- Incubation and Measurement: Incubate plates for 1-24 hours (depending on experimental design). Measure fluorescence at excitation/emission of 485/535 nm using a microplate reader at predetermined time points.
- Parallel Cytotoxicity Assessment: Perform LDH assay following manufacturer's protocol to correlate ROS generation with cytotoxicity.
Data Analysis:
- Express ROS levels as fold-increase over untreated controls.
- Calculate EC₅₀ values for ROS induction using nonlinear regression.
- Determine the therapeutic index by comparing ROS EC₅₀ to therapeutic concentration.
Protocol 2: Assessment of Pro-Inflammatory Cytokine Response
Objective: To evaluate nanoparticle-induced immunotoxicity through quantification of pro-inflammatory cytokine secretion.
Materials:
- Research Reagent Solutions:
- ELISA kits for TNF-α, IL-1β, IL-6, IL-8
- LPS (Lipopolysaccharide) as positive control
- Cell culture medium for immune cells (e.g., RPMI-1640 with 10% FBS)
- Protein extraction buffer (RIPA buffer with protease inhibitors)
- Multiplex cytokine array (optional for high-throughput screening)
Methodology:
- Immune Cell Culture: Seed human peripheral blood mononuclear cells (PBMCs) or THP-1-derived macrophages in 24-well plates at 5×10⁵ cells/well in complete medium.
- Nanoparticle Exposure: Treat cells with nanoparticle suspensions across a concentration range (0.1-100 µg/mL) for 24 hours. Include LPS (100 ng/mL) as positive control and medium alone as negative control.
- Sample Collection: Collect culture supernatants by centrifugation at 300×g for 5 minutes. Store at -80°C until analysis.
- Cytokine Quantification: Perform ELISA according to manufacturer's instructions for target cytokines. Use a standard curve for absolute quantification.
- RNA Extraction and qPCR (Optional): Extract total RNA from cell pellets using TRIzol reagent. Perform reverse transcription and qPCR for cytokine gene expression analysis.
Data Analysis:
- Express cytokine levels as pg/mL normalized to total protein content or cell number.
- Determine statistically significant increases over control using one-way ANOVA with post-hoc testing.
- Establish no-observed-effect-level (NOAEL) and lowest-observed-effect-level (LOAEL) for immunotoxicity.
Protocol 3: In Vivo Biodistribution and Long-Term Toxicity
Objective: To assess nanoparticle accumulation in major organs and evaluate chronic toxicity effects.
Materials:
- Research Reagent Solutions:
- Fluorescently-labeled nanoparticles (e.g., Cy5.5, DiR) or metal-based NPs for ICP-MS
- Anesthetic agents (ketamine/xylazine or isoflurane)
- Perfusion buffer (PBS, pH 7.4) and 4% paraformaldehyde
- Tissue homogenization buffers
- Hematoxylin and Eosin (H&E) staining solutions
- Oxidative stress biomarkers (MDA, 8-OHdG, GSH/GSSG) assay kits
Methodology:
- Animal Dosing: Administer nanoparticles to rodents (typically mice or rats) via relevant route (IV, IP, oral) at therapeutic and supratherapeutic doses (e.g., 1-100 mg/kg). Include vehicle control group.
- In Vivo Imaging: For fluorescent NPs, image animals at predetermined time points (1, 4, 24, 48, 72 hours) using an IVIS imaging system. Quantify fluorescence intensity in regions of interest corresponding to major organs.
- Tissue Collection: Euthanize animals at study endpoint (acute: 7-14 days; chronic: 30-90 days). Collect major organs (liver, spleen, kidney, lung, brain, heart) weighing each organ prior to processing.
- Histopathological Analysis: Fix tissues in 4% PFA, embed in paraffin, section at 5 µm thickness, and stain with H&E. Score pathological changes (inflammation, necrosis, fibrosis) using standardized scoring systems.
- Biochemical Analysis: Homogenize tissues and quantify (a) oxidative stress markers (MDA, 8-OHdG), (b) antioxidant enzymes (SOD, catalase, GPx), and (c) inflammatory cytokines in tissue homogenates.
- Elemental Analysis: For metal-containing NPs, digest tissues in nitric acid and quantify metal content using ICP-MS.
Data Analysis:
- Calculate biodistribution as percentage of injected dose per gram of tissue (%ID/g).
- Correlate organ nanoparticle levels with histopathological and biochemical changes.
- Establish maximum tolerated dose (MTD) and no-observed-adverse-effect-level (NOAEL).
Signaling Pathways in Nanotoxicity
The following diagrams illustrate key signaling pathways involved in nanoparticle-induced toxicity, generated using Graphviz DOT language.
Oxidative Stress and Inflammation Pathway
Oxidative Stress and Inflammation Pathway: This diagram illustrates the central role of ROS generation in triggering oxidative stress, which subsequently activates inflammatory responses through NF-κB and causes direct cellular damage leading to apoptosis and autophagy.
Nanotoxicity Experimental Workflow
Nanotoxicity Assessment Workflow: This workflow diagram outlines the sequential approach for comprehensive nanotoxicity evaluation, progressing from physicochemical characterization through in vitro screening to in vivo validation and integrated safety assessment.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Nanotoxicity Assessment
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| ROS Detection Probes | Quantification of reactive oxygen species | DCFH-DA (general ROS), MitoSOX (mitochondrial superoxide), DHE (superoxide anion) |
| Cell Viability Assays | Assessment of cytotoxicity and cell death mechanisms | MTT/WST-1 (metabolic activity), LDH release (membrane integrity), Annexin V/PI (apoptosis) |
| Cytokine Detection Kits | Measurement of pro-inflammatory immune responses | ELISA kits (TNF-α, IL-1β, IL-6, IL-8), Multiplex bead-based arrays |
| Oxidative Stress Biomarkers | Evaluation of oxidative damage to biomolecules | Malondialdehyde (MDA, lipid peroxidation), 8-OHdG (DNA oxidation), GSH/GSSG ratio (redox status) |
| Protein Corona Analysis | Characterization of NP-protein interactions | SDS-PAGE, Mass spectrometry, Size exclusion chromatography |
| Histopathological Stains | Tissue-level toxicity assessment | H&E (general morphology), TUNEL (apoptosis), Masson's Trichrome (fibrosis) |
Addressing nanotoxicity requires a multidisciplinary approach that integrates materials science, biology, and toxicology. The protocols and application notes outlined herein provide a framework for systematic evaluation of immunological responses, oxidative stress, and long-term safety concerns associated with nanoparticle exposure in drug delivery systems.
Future directions should focus on:
- Advanced Characterization Techniques: Developing more sensitive methods for detecting and quantifying nanomaterials in complex biological matrices [87].
- Alternative Testing Strategies: Implementing 3D tissue models, organ-on-chip systems, and in silico approaches to reduce animal testing while improving predictive value [87].
- AI-Driven Safety Assessment: Leveraging machine learning to analyze complex nanotoxicity data, identify patterns, and predict toxicity based on nanoparticle properties [84].
- Standardized Regulatory Frameworks: Establishing globally harmonized guidelines for nanomaterial safety assessment to ensure safe commercialization [84] [87].
By adopting these comprehensive assessment strategies, researchers can facilitate the development of safer nanomedicines while accelerating their translation into clinical applications that benefit human health.
Polyethylene glycol (PEG) is a synthetic, linear, nonionic polymer composed of repeating ethylene glycol units that has become a cornerstone of nanomedicine development. By creating a hydrophilic shield around drug carriers, PEGylation confers "stealth" properties that reduce opsonization, minimize recognition by the mononuclear phagocyte system (MPS), and significantly prolong circulation half-life [88] [89]. These properties have made PEG an essential component in numerous therapeutic formulations, from protein therapeutics to lipid nanoparticles (LNPs) used in mRNA vaccines [90] [7].
However, the very success of PEGylated therapeutics has revealed a significant dilemma: the potential for PEG to trigger immune responses. Anti-PEG antibodies (APAs), both pre-existing and treatment-induced, can cause accelerated blood clearance (ABC), reduce therapeutic efficacy, and potentially trigger hypersensitivity reactions [88] [91]. This application note examines this critical challenge, providing experimental frameworks and data analysis tools to guide researchers in characterizing and mitigating PEG immunogenicity within targeted drug delivery systems.
Quantitative Characterization of PEG Immunogenicity
Prevalence and Impact of Anti-PEG Antibodies
Table 1: Anti-PEG Antibody Prevalence and Clinical Impact
| Parameter | Reported Values | Biological Consequences | Detection Methods |
|---|---|---|---|
| Pre-existing Anti-PEG Antibodies | 0.2% - 72% in healthy individuals [91] | Accelerated blood clearance (ABC) of subsequent PEGylated doses [88] [91] | Enzyme-Linked Immunosorbent Assay (ELISA) [91] |
| Antibody Classes | IgM, IgG, IgA [91] | IgM: Strong complement activation; IgG: Enhanced opsonization [91] | Isotype-specific ELISA [91] |
| PEG Molecular Weight Impact | Higher immunogenicity with PEG >20,000 Da [91] | Increased antibody titers with higher molecular weight [91] | Size-exclusion chromatography, MALDI-TOF |
| ABC Phenomenon | Up to 90% reduction in circulation half-life upon repeated dosing [88] | Reduced efficacy, altered biodistribution [88] [92] | Pharmacokinetic profiling, imaging studies |
Factors Influencing PEG Immunogenicity
Table 2: Factors Affecting PEG Immunogenicity and Stealth Properties
| Factor | Impact on Stealth Properties | Impact on Immunogenicity | Optimization Strategy |
|---|---|---|---|
| Molecular Weight | Higher MW: Longer circulation; Lower MW: Reduced shielding [91] | Higher MW: Increased immunogenicity [91] | Use lowest MW PEG sufficient for stealth (e.g., 2,000-5,000 Da) [91] |
| Terminal Functional Groups | Methoxy-terminated (mPEG) most common for conjugation [88] | Hydroxyl groups may increase immunogenicity [88] | Prefer mPEG for conjugations |
| Grafting Density | High density: Better steric protection [88] | Very high density may paradoxically increase immune recognition [7] | Optimize for balance between stealth and low immunogenicity |
| Carrier Properties | Protein carriers enhance immunogenicity [88] | Liposomal carriers can trigger T-cell independent responses [91] | Consider carrier contribution to overall immunogenicity |
| Administration Route | Intravenous: Direct systemic exposure [7] | Intramuscular: Potentially lower systemic antibody response [92] | Route influences immune response magnitude |
Experimental Protocols for PEG Immunogenicity Assessment
Protocol: Evaluation of Anti-PEG Antibody Responses
Objective: To quantify and characterize anti-PEG antibody levels in serum samples before and after administration of PEGylated nanomedicines.
Materials:
- PEGylated antigen (e.g., PEG-BSA) for plate coating
- Control non-PEGylated antigen
- Test serum samples (pre- and post-dose)
- Positive control (monoclonal anti-PEG antibody)
- Isotype-specific detection antibodies (anti-human IgM, IgG, IgA)
- ELISA plates, plate washer, and microplate reader
Procedure:
- Coating: Coat ELISA plates with 100 µL/well of PEGylated antigen (2-5 µg/mL) in carbonate buffer. Incubate overnight at 4°C.
- Blocking: Wash plates 3× with PBS-Tween, then block with 200 µL/well of 1% BSA in PBS for 2 hours at room temperature.
- Sample Incubation: Prepare serial dilutions of test serum (typically from 1:50 to 1:10,000). Add 100 µL/well of each dilution in duplicate. Incubate 2 hours at room temperature.
- Detection: Wash plates, add isotype-specific detection antibodies conjugated to horseradish peroxidase. Incubate 1 hour at room temperature.
- Signal Development: Add TMB substrate, incubate 15-30 minutes, then stop with sulfuric acid. Measure absorbance at 450 nm.
- Data Analysis: Calculate antibody titers using a standard curve or determine endpoint titers as the highest dilution giving absorbance >2× background.
Technical Notes: Include appropriate controls for non-specific binding to the carrier protein. Standardize assay conditions using reference anti-PEG antibodies when available. Consider using a bridging ELISA format for improved specificity [91].
Protocol: Assessment of Accelerated Blood Clearance (ABC) Phenomenon
Objective: To evaluate the impact of anti-PEG antibodies on the pharmacokinetics and biodistribution of PEGylated nanoparticles upon repeated administration.
Materials:
- PEGylated nanoparticles (radiolabeled or fluorescently labeled)
- Control non-PEGylated nanoparticles
- Animal model (typically rodent)
- Imaging system (e.g., IVIS, SPECT/CT) or gamma counter
- Blood collection equipment
Procedure:
- Priming Dose: Administer initial dose of PEGylated nanoparticles (0.5-1 mg/kg PEG) intravenously to experimental animals.
- Waiting Period: Allow 7-14 days for immune response development.
- Challenge Dose: Administer second dose of radiolabeled or fluorescently labeled PEGylated nanoparticles at same dose level.
- Sample Collection: Collect blood samples at predetermined timepoints (e.g., 0.5, 2, 6, 12, 24 hours post-injection).
- Analysis: Quantify nanoparticle concentration in blood samples using appropriate method (gamma counting, fluorescence measurement).
- Biodistribution: At terminal timepoint, harvest major organs and quantify nanoparticle accumulation.
- Correlation: Measure anti-PEG antibody levels in terminal serum samples and correlate with pharmacokinetic parameters.
Technical Notes: Include control groups receiving non-PEGylated particles or naive animals. Calculate key pharmacokinetic parameters: elimination half-life, AUC, and clearance. The ABC effect is confirmed when significantly reduced circulation time is observed following the second dose in primed animals [88] [91].
Mechanisms and Pathways of PEG Immunogenicity
The immunogenicity of PEG involves multiple mechanisms that can be categorized as thymus-dependent (TD) and thymus-independent (TI) pathways. Understanding these mechanisms is crucial for developing strategies to mitigate immune responses.
Thymus-Dependent Pathway: PEGylated therapeutics containing protein components can trigger a classical TD immune response. B cells recognize the PEG backbone through B cell receptors (BCRs), while CD4+ T helper cells (particularly follicular helper T cells) respond to the protein carrier. This collaboration leads to class switching and the production of high-affinity anti-PEG IgG antibodies [91].
Thymus-Independent Pathway: Highly repetitive PEG structures on nanoparticles or liposomes can act as TI-2 antigens, directly activating marginal zone B cells without T cell help. This pathway primarily generates anti-PEG IgM antibodies through BCR cross-linking [91].
Both pathways ultimately contribute to the ABC phenomenon, where pre-existing or induced anti-PEG antibodies bind to subsequent doses of PEGylated therapeutics, promoting complement activation and rapid clearance by phagocytic cells in the liver and spleen [88] [91] [92].
Strategic Approaches to Mitigate PEG Immunogenicity
Formulation Strategies and PEG Alternatives
Table 3: Strategies to Overcome PEG Immunogenicity
| Strategy | Mechanism | Examples | Development Status |
|---|---|---|---|
| PEG Optimization | Adjust molecular weight, branching, density | Lower MW PEG (2,000 Da), branched PEG | Clinically implemented [88] [91] |
| Zwitterionic Polymers | Superhydrophilicity with neutral charge | Poly(carboxybetaine) (PCB) lipids | Preclinical validation [90] |
| Biomimetic Coatings | "Self" camouflage | CD47-mimetic peptides, cell membrane coatings | Research phase [93] |
| Alternative Polymers | Different chemistry, reduced immunogenicity | Poly(2-oxazoline), Poly(glycerol) | Early clinical evaluation [7] [91] |
| Dosing Regimen Adjustment | Minimize immune stimulation | Extended dosing intervals, high initial dose | Clinically implemented [93] |
Protocol: Evaluation of PEG Alternatives in LNP Formulations
Objective: To screen and validate alternative polymers for replacing PEG in lipid nanoparticle formulations while maintaining stability and transfection efficiency.
Materials:
- Ionizable lipids, phospholipids, cholesterol
- PEG-lipids (control)
- Alternative polymer-lipids (e.g., PCB-lipids, poly(2-oxazoline)-lipids)
- mRNA (reporter or therapeutic)
- Microfluidic mixing device
- Dynamic light scattering instrument
- Cell culture reagents
- Animal models
Procedure:
- LNP Formulation: Prepare LNP using microfluidic mixing with identical compositions except for the surface-stabilizing polymer (PEG vs. alternatives).
- Characterization: Measure particle size, PDI, zeta potential, and mRNA encapsulation efficiency for all formulations.
- Stability Testing: Assess physical stability in storage buffer and physiological fluids over time.
- In Vitro Transfection: Evaluate transfection efficiency and cell viability in relevant cell lines.
- Anti-PEG Antibody Binding: Assess binding of pre-existing anti-PEG antibodies to alternative formulations using ELISA or surface plasmon resonance.
- In Vivo Performance: Compare pharmacokinetics, biodistribution, and target protein expression between formulations in appropriate animal models.
- Immunogenicity Assessment: Measure antibody responses against the alternative polymers after repeated administration.
Technical Notes: Prioritize polymers with regulatory approval history. Include both efficacy and comprehensive immunogenicity assessment. PCB-lipids have shown enhanced endosomal escape and reduced immunogenicity in preclinical models [90].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for PEG Immunogenicity Research
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| PEGylated Antigens | PEG-BSA, PEG-OVA, PEG-liposomes | Standardized immunogens | Positive controls for antibody detection |
| Detection Antibodies | Anti-PEG IgM/IgG monoclonal antibodies | ELISA development and standardization | Quantification of anti-PEG antibodies |
| Reference Materials | PEGylated therapeutics (Doxil, Onpattro) | Benchmarking studies | Comparative immunogenicity assessment |
| Alternative Polymers | PCB-lipids, POZ-lipids, BPLs | Formulation screening | PEG replacement candidates |
| Animal Models | Mice, rats, non-human primates | In vivo immunogenicity | ABC phenomenon evaluation |
| Assay Kits | Complement activation kits, cytokine panels | Mechanism elucidation | Understanding immune responses |
The PEG dilemma represents a significant challenge in nanomedicine development, requiring careful balancing of stealth properties against potential immunogenicity. Researchers must incorporate rigorous immunogenicity assessment throughout the development pipeline, from early screening to advanced preclinical models. The experimental frameworks provided herein enable systematic evaluation of PEG immune responses, while the emerging strategies for mitigation offer pathways to overcome these challenges. As the field advances, the rational design of next-generation stealth nanomaterials with reduced immunogenicity will be crucial for realizing the full potential of targeted drug delivery systems.
In the field of nanotechnology-based drug delivery, Critical Quality Attributes (CQAs) are fundamental properties that must be controlled within predefined limits to ensure the safety, efficacy, and quality of the final pharmaceutical product [94]. For nanoparticle-based therapeutics, establishing well-defined CQAs is particularly crucial as these parameters directly influence in vivo behavior, including biodistribution, targeting efficiency, and drug release profiles [7]. The identification and control of CQAs form the foundation of the Quality by Design (QbD) framework, a systematic approach to development that emphasizes product and process understanding based on sound science and quality risk management [95] [94].
The transition of nanomedicines from laboratory research to clinical application has been hampered by a significant translational gap, with only an estimated 50–80 nanomedicines achieving global approval by 2025 despite thousands of published candidates [7]. This gap is frequently attributed to insufficient focus on advanced formulation strategies and inconsistent product quality during scale-up. Batch-to-batch consistency remains a formidable challenge in nanomedicine manufacturing, where minor variations in composition or process parameters can significantly alter the physicochemical properties and biological performance of nanoparticles [7] [96]. Within this context, CQAs serve as essential metrics for guiding formulation optimization, manufacturing process control, and regulatory evaluation, ultimately bridging the gap between promising preclinical results and successful clinical translation.
Defining CQAs within the QbD Framework for Nanomedicines
The QbD Paradigm and Its Key Elements
The QbD framework represents a paradigm shift from traditional quality control methods, which primarily rely on end-product testing, toward proactively building quality into the product from the initial development stages [94]. This systematic approach requires thorough scientific understanding and emphasizes control over Critical Material Attributes (CMAs) and Critical Process Parameters (CPPs) that impact the identified CQAs [95]. Studies indicate that implementing QbD can reduce development time by up to 40% and decrease material wastage by up to 50% through the establishment of a robust design space that minimizes batch failures [94].
The core elements of the QbD framework for nanomedicine development include:
- Quality Target Product Profile (QTPP): A prospective summary of the quality characteristics that a drug product should possess to ensure the desired safety, efficacy, and delivery [95] [94]. For a nanoparticle formulation, this typically includes the route of administration, dosage form, pharmacokinetic parameters, and stability criteria.
- Critical Quality Attributes (CQAs): Physical, chemical, biological, or microbiological properties or characteristics that should be within an appropriate limit, range, or distribution to ensure the desired product quality [94].
- Critical Material Attributes (CMAs) and Critical Process Parameters (CPPs): Material characteristics and process parameters that significantly impact the CQAs of the final product and must be carefully controlled [95].
- Design Space: The multidimensional combination and interaction of input variables and process parameters that have been demonstrated to provide assurance of quality [94].
- Control Strategy: A planned set of controls derived from current product and process understanding that ensures process performance and product quality [94].
Table 1: Key Elements of the QbD Framework for Nanomedicine Development
| QbD Element | Definition | Nanomedicine Example |
|---|---|---|
| Quality Target Product Profile (QTPP) | Prospective summary of quality characteristics | Targeted liposome for oncology with reduced systemic toxicity |
| Critical Quality Attributes (CQAs) | Properties within limits to ensure product quality | Particle size, size distribution, drug loading, release rate |
| Critical Material Attributes (CMAs) | Material characteristics affecting CQAs | Lipid purity, polymer molecular weight, excipient quality |
| Critical Process Parameters (CPPs) | Process parameters affecting CQAs | Homogenization pressure, mixing rate, temperature control |
| Design Space | Proven acceptable ranges for CPPs and CMAs | Established ranges for solvent volume and injection rate |
| Control Strategy | Planned controls to ensure quality | In-process monitoring, final product testing, procedures |
Identification and Categorization of CQAs for Nanoparticle Systems
The identification of CQAs for nanoparticle-based drug delivery systems begins with the QTPP and employs a systematic risk assessment process to determine which quality attributes are truly critical to product performance [95] [94]. For nanomedicines, CQAs can be categorized into several key classes:
- Physicochemical CQAs: These include parameters such as particle size, size distribution (polydispersity index), surface charge (zeta potential), drug loading capacity, encapsulation efficiency, and in vitro drug release profile [95].
- Biological CQAs: For advanced nanomedicines, these may include targeting ligand density, surface hydrophobicity, protein corona composition, and immunogenicity potential [7].
- Performance CQAs: These attributes relate to the product's functional behavior, such as stability under various storage conditions, sterility, and endotoxin levels [97].
The relationship between the QTPP and CQAs is hierarchical, with the QTPP guiding the identification of relevant CQAs, which in turn are influenced by specific CMAs and CPPs. This systematic approach ensures that quality considerations are integrated throughout the product lifecycle, from initial development through commercial manufacturing.
Diagram 1: QbD workflow for CQA identification
Essential CQAs for Nanoparticle-Based Drug Delivery Systems
Core Physicochemical CQAs
For nanoparticle-based drug delivery systems, certain physicochemical attributes consistently emerge as critical due to their profound influence on in vivo performance, stability, and therapeutic efficacy. The most fundamental CQAs include:
Particle Size and Size Distribution (PDI): Particle size significantly impacts biodistribution, cellular uptake, and clearance mechanisms. Nanoparticles in the range of 10-200 nm are generally preferred for systemic administration, as they can avoid rapid renal clearance while potentially leveraging the Enhanced Permeability and Retention (EPR) effect in tumor tissues [7] [98]. The polydispersity index (PDI) serves as a measure of particle size heterogeneity, with values below 0.2 generally indicating a monodisperse population essential for predictable behavior in vivo [95].
Zeta Potential: This parameter reflects the surface charge of nanoparticles and influences their colloidal stability, interaction with biological components, and cellular uptake. Highly positive or negative zeta potentials (typically >|20| mV) generally enhance stability by preventing aggregation through electrostatic repulsion [95]. Surface charge also dictates opsonization and clearance by the reticuloendothelial system (RES), with neutral or slightly negative charges often exhibiting longer circulation times [7].
Drug Loading Capacity and Encapsulation Efficiency: Drug loading (expressed as weight percentage of drug in the nanoparticle) and encapsulation efficiency (percentage of incorporated drug relative to the initial amount) directly impact therapeutic efficacy and dosage requirements [95]. High encapsulation efficiency minimizes drug wastage during preparation, while sufficient loading capacity reduces the quantity of carrier material needed for therapeutic doses, potentially reducing carrier-related toxicity [98].
In Vitro Drug Release Profile: The release kinetics of the encapsulated therapeutic agent from the nanoparticle carrier must be carefully controlled to ensure appropriate drug exposure at the target site. Premature release can lead to systemic toxicity, while insufficient release compromises therapeutic efficacy [7]. Release profiles should be evaluated under physiologically relevant conditions that may include pH gradients or enzymatic environments mimicking the target tissue [98].
Table 2: Essential CQAs for Nanoparticle-Based Drug Delivery Systems
| CQA Category | Specific Parameter | Target Range | Impact on Performance | ||
|---|---|---|---|---|---|
| Size & Distribution | Particle Size | 10-200 nm (IV) | Biodistribution, EPR effect, cellular uptake | ||
| Polydispersity Index (PDI) | < 0.2 (monodisperse) | Batch uniformity, predictable pharmacokinetics | |||
| Surface Properties | Zeta Potential | > | 20 | mV (colloidal) | Physical stability, protein corona formation |
| Surface Morphology | Smooth, spherical | Circulation time, biological interactions | |||
| Drug Content | Encapsulation Efficiency | > 80% (preferred) | Process efficiency, cost-effectiveness | ||
| Drug Loading | 5-20% (varies by system) | Dosage requirement, excipient-related toxicity | |||
| Release Profile | Release Kinetics | Sustained/controlled | Therapeutic efficacy, safety profile | ||
| Burst Release | < 40% (initial) | Prevention of rapid drug loss | |||
| Stability | Physical Stability | No aggregation | Shelf-life, administration safety | ||
| Chemical Stability | > 95% drug potency | Efficacy over shelf-life |
Advanced CQAs for Targeted Nanomedicines
For actively targeted nanoparticles bearing specific ligands for enhanced cellular uptake, additional CQAs become critical:
Ligand Density and Orientation: The surface density of targeting ligands (e.g., antibodies, peptides, aptamers) must be optimized to ensure efficient target binding without compromising nanoparticle stability or inducing immunogenicity [7] [98]. Both insufficient and excessive ligand density can diminish targeting efficiency through different mechanisms.
Surface PEGylation Density: Polyethylene glycol (PEG) coating is widely employed to confer "stealth" properties by reducing opsonization and RES clearance. However, the density and molecular weight of PEG chains must be carefully controlled, as these parameters significantly impact circulation half-life and potential immunogenicity [7]. Recent concerns regarding anti-PEG antibodies have heightened the importance of this CQA [7].
Stability Under Storage and In Vivo Conditions: Chemical and physical stability of the nanoparticle formulation under anticipated storage conditions represents a crucial CQA for product shelf-life [97]. Additionally, stability in biological fluids affects drug release kinetics and nanoparticle integrity following administration [7].
Experimental Protocols for CQA Characterization
Protocol 1: Comprehensive Particle Size and Zeta Potential Analysis
Principle: Dynamic Light Scattering (DLS) determines particle size and size distribution by measuring Brownian motion, while Laser Doppler Velocimetry measures zeta potential based on electrophoretic mobility [95].
Materials and Equipment:
- Nanoparticle suspension (appropriately diluted)
- Zeta potential buffer (e.g., 1 mM KCl or physiologically relevant buffer)
- DLS/Zeta potential analyzer (e.g., Malvern Zetasizer)
- Disposable zeta cells and cuvettes
- Syringe filters (0.45 or 0.22 µm)
- Temperature-controlled sample chamber
Procedure:
- Sample Preparation: Dilute the nanoparticle suspension with appropriate buffer (typically 1:10 to 1:100 v/v) to achieve optimal scattering intensity. Filter the diluted sample through a 0.45 µm syringe filter to remove dust particles.
- Instrument Calibration: Perform daily calibration using a standard latex suspension of known size and zeta potential according to manufacturer specifications.
- Particle Size Measurement:
- Transfer 1 mL of filtered sample into a disposable sizing cuvette.
- Equilibrate at 25°C for 2 minutes in the instrument.
- Set measurement parameters: 173° backscatter detection, automatic attenuation selection.
- Perform minimum 3 measurements of 10-15 sub-runs each.
- Record the Z-average diameter and polydispersity index (PDI).
- Zeta Potential Measurement:
- Transfer 0.8 mL of sample into a disposable zeta cell.
- Equilibrate at 25°C for 2 minutes.
- Set voltage to automatic mode and measure 3-5 runs with 10-100 sub-runs.
- Record zeta potential and conductivity.
- Data Analysis: Report mean values ± standard deviation. For regulatory submissions, ensure compliance with appropriate guidelines (e.g., ICH Q2(R1)).
Acceptance Criteria: Size distribution should be unimodal with PDI < 0.2. Zeta potential values should be consistent with historical data with standard deviation < 5%.
Protocol 2: Drug Encapsulation Efficiency and Loading Capacity
Principle: Separation of unencapsulated drug from nanoparticle-associated drug followed by quantitative analysis of drug content [95].
Materials and Equipment:
- Ultracentrifuge with appropriate rotors
- Centrifugal filter devices (MWCO appropriate for nanoparticle retention)
- HPLC system with UV/Vis detector or other validated analytical method
- Appropriate solvents for drug extraction
- Standard drug solutions for calibration curve
Procedure:
- Separation of Unencapsulated Drug:
- Method A (Ultracentrifugation): Centrifuge nanoparticle suspension at 100,000 × g for 1 hour at 4°C. Carefully collect supernatant for free drug analysis.
- Method B (Dialysis): Dialyze nanoparticle suspension against appropriate buffer using membrane with suitable MWCO for 4-6 hours with buffer changes.
- Method C (Size Exclusion Chromatography): Pass sample through Sephadex G-50 or similar column to separate nanoparticles from free drug.
- Drug Extraction from Nanoparticles:
- Lyse the nanoparticle pellet or retained fraction using appropriate solvent (e.g., methanol, acetonitrile, or Triton X-100 solution).
- Vortex vigorously for 1 minute and sonicate for 15 minutes.
- Centrifuge at 15,000 × g for 10 minutes to remove insoluble excipients.
- Quantitative Analysis:
- Analyze both free drug (supernatant) and extracted drug (nanoparticle fraction) using validated HPLC or spectrophotometric method.
- Use standard calibration curve for quantification (typically 5-7 concentration points in triplicate).
- Calculation:
- Encapsulation Efficiency (%) = (Amount of drug in nanoparticle fraction / Total drug amount) × 100
- Drug Loading (%) = (Mass of drug in nanoparticles / Total mass of nanoparticles) × 100
Acceptance Criteria: Encapsulation efficiency should be >80% for most applications with RSD < 5% for triplicate measurements.
Protocol 3:In VitroDrug Release Profile
Principle: Monitoring drug release from nanoparticles under sink conditions using dialysis or continuous flow methods to simulate physiological environments [95].
Materials and Equipment:
- Dialysis membranes with appropriate MWCO
- Dissolution apparatus (USP type I or II)
- Reciprocating shaker water bath
- Sampling system with automated fraction collector
- Analytical instrument for drug quantification (HPLC, UV-Vis)
Procedure:
- Release Media Selection: Prepare physiologically relevant media (e.g., PBS pH 7.4, simulated gastric/intestinal fluids) with added surfactants (0.1-0.5% Tween 80 or SDS) to maintain sink conditions.
- Dialysis Method:
- Place 2-5 mL of nanoparticle suspension in dialysis membrane (MWCO typically 12-14 kDa).
- Immerse membrane in 200-500 mL of release medium with continuous stirring at 100 rpm.
- Maintain temperature at 37±0.5°C.
- Sampling Protocol:
- Withdraw predetermined aliquots (e.g., 1 mL) at scheduled time intervals (0.5, 1, 2, 4, 8, 12, 24, 48, 72 hours).
- Replace with equal volume of fresh pre-warmed medium to maintain sink conditions.
- Filter samples through 0.22 µm filters before analysis.
- Analysis and Kinetics:
- Quantify drug content in samples using validated analytical method.
- Calculate cumulative drug release percentage at each time point.
- Fit release data to appropriate mathematical models (zero-order, first-order, Higuchi, Korsmeyer-Peppas).
- Data Interpretation: Evaluate release mechanism based on model fitting. For nanoparticles, a biphasic release profile is common with initial burst followed by sustained release.
Acceptance Criteria: Sink conditions maintained throughout (concentration < 20% of saturation solubility). Release profile should demonstrate consistency with established specifications for the product.
Statistical Optimization and Design of Experiments (DoE) for CQA Control
DoE Methodology for Nanomedicine Development
Design of Experiments (DoE) represents a powerful statistical approach for systematically evaluating the relationship between multiple input variables (CMAs and CPPs) and output responses (CQAs) while minimizing experimental effort [96]. Unlike traditional trial-and-error methods that vary one factor at a time, DoE enables simultaneous variation of multiple factors, allowing identification of interaction effects and optimal parameter combinations that might otherwise be missed [96].
The application of DoE in nanomedicine development typically follows a structured workflow:
- Screening Designs: Initial experiments to identify which factors from a larger set have significant effects on CQAs. Commonly used designs include Plackett-Burman or fractional factorial designs [96].
- Optimization Designs: Once critical factors are identified, response surface methodology (RSM) designs such as Central Composite Design (CCD) or Box-Behnken Design are employed to model the relationship between factors and responses and identify optimal operating conditions [96].
- Robustness Testing: Final confirmation experiments to verify that the process remains within acceptable limits despite minor variations in input parameters [96].
Diagram 2: DoE approach for CQA optimization
Case Study: DoE Application in Lipid Nanoparticle Formulation
A recent study on oral lipid nanoparticle development demonstrated the effective application of QbD and DoE principles [95]. The researchers implemented a systematic approach:
- QTPP Definition: Established target product profile including gastrointestinal stability, enhanced permeability, and improved oral bioavailability.
- CQA Identification: Identified particle size, PDI, zeta potential, encapsulation efficiency, and drug release as critical quality attributes.
- Risk Assessment: Conducted initial risk analysis to identify potentially influential material attributes and process parameters.
- DoE Implementation: Employed a Central Composite Design to investigate the effects of lipid concentration, surfactant ratio, and homogenization parameters on CQAs.
- Design Space Establishment: Defined the optimal operating ranges for critical parameters that consistently produced LNPs meeting all CQA specifications.
This systematic approach resulted in a robust formulation with improved performance characteristics and enhanced understanding of the relationship between process parameters and product quality [95].
Table 3: DoE Applications in Nanomedicine Optimization
| DoE Design Type | Primary Application | Factors Studied | Responses (CQAs) Monitored |
|---|---|---|---|
| Plackett-Burman | Screening multiple factors | 5-11 factors at 2 levels | Particle size, PDI, zeta potential |
| Full Factorial | Studying interactions | 2-4 factors at 2-3 levels | Encapsulation efficiency, drug loading |
| Central Composite | Response surface modeling | 2-5 factors at 3-5 levels | Particle size, drug release, stability |
| Box-Behnken | Optimization with fewer runs | 3-7 factors at 3 levels | Multiple CQAs simultaneously |
| Mixture Design | Formulation optimization | Component ratios | Physical properties, performance |
The Scientist's Toolkit: Essential Reagents and Materials for CQA Assessment
Table 4: Essential Research Reagents and Materials for CQA Characterization
| Category | Specific Items | Function/Application | Technical Notes |
|---|---|---|---|
| Characterization Standards | Latex size standards (NIST-traceable) | Instrument calibration for DLS | Multiple sizes: 50 nm, 100 nm, 200 nm |
| Zeta potential transfer standard | Zeta potential calibration | -50 mV ± 5 mV (e.g., dispersions in NaCl) | |
| Separation Materials | Dialysis membranes (MWCO 3.5-100 kDa) | Separation of free drug | Regenerate cellulose preferred for compatibility |
| Centrifugal filters (MWCO 10-300 kDa) | Rapid separation of unencapsulated drug | Various membrane materials available | |
| Size exclusion columns (Sephadex G-50, G-100) | Chromatographic separation | Remove free drug without dilution | |
| Analytical Reagents | HPLC-grade solvents (acetonitrile, methanol) | Drug extraction and analysis | LC-MS grade for mass spectrometry |
| Buffers (PBS, HEPES, acetate) | Physiological simulation | Filter through 0.22 µm before use | |
| Surfactants (Tween 80, SDS) | Sink condition maintenance | Critical for release studies | |
| Stability Assessment | Cryoprotectants (trehalose, sucrose) | Lyophilization studies | Prevent particle aggregation during freezing |
| Antioxidants (BHT, ascorbic acid) | Oxidative stability testing | Especially for lipid-based systems | |
| Reference Materials | USP dissolution calibration standards | Dissolution apparatus qualification | Prednisone salicylic acid sets |
| Certified reference materials | Analytical method validation | For regulated laboratory environments |
Regulatory Considerations and Implementation Strategy
The implementation of a CQA-based quality system requires careful consideration of regulatory expectations and practical implementation strategies. Regulatory agencies including the FDA and EMA have increasingly emphasized the importance of QbD principles in pharmaceutical development, with QbD becoming an integral component of new drug applications [94].
A successful CQA implementation strategy includes:
- Early CQA Identification: Begin CQA identification during initial formulation development rather than as a retrospective exercise [94].
- Risk-Based Approach: Utilize formal risk assessment methodologies (e.g., Failure Mode and Effects Analysis) to prioritize CQAs based on their potential impact on safety and efficacy [94].
- Design Space Development: Establish a design space that defines the multidimensional combination of input variables that consistently produce material meeting CQA specifications [95] [94].
- Control Strategy Implementation: Develop a comprehensive control strategy that may include input material controls, process controls, in-process testing, and final product specifications [94].
- Lifecycle Management: Implement continuous verification and improvement processes to maintain product quality throughout the product lifecycle [97].
For nanotechnology-based products specifically, regulatory guidance continues to evolve, with particular attention to characterization complexity, biodistribution assessments, and immunogenicity potential [7] [97]. A well-documented CQA framework provides a solid foundation for regulatory submissions and facilitates meaningful dialogue with health authorities throughout the development process.
Clinical and Commercial Validation: From Regulatory Pathways to Market Analysis
The integration of nanotechnology into medicine has revolutionized targeted drug delivery, offering sophisticated solutions to longstanding challenges in therapeutic efficacy and safety. Nanomedicines, defined as therapeutic agents engineered at the nanoscale (typically 1-300 nm), have demonstrated remarkable potential to alter the pharmacokinetics and biodistribution of active pharmaceutical ingredients [99] [100]. By enhancing drug solubility, prolonging circulation half-life, and enabling targeted delivery to diseased tissues, nanomedicines significantly improve therapeutic indices while reducing off-target toxicity [55] [101]. This application note provides a comprehensive analysis of the current clinical landscape of approved nanomedicines and clinical trial outcomes, framed within the broader context of advancing targeted drug delivery systems. We present structured quantitative data, detailed experimental protocols, and visualization tools to support researchers and drug development professionals in navigating this rapidly evolving field.
Current Clinical Landscape of Approved Nanomedicines
The clinical translation of nanomedicines has accelerated over the past three decades, with numerous formulations receiving regulatory approval across various therapeutic areas, particularly in oncology.
Analysis of FDA-Approved Nanomedicines
Table 1: Recently FDA-Approved Nanomedicines (Since 2016)
| Product Name | Nanoparticle Type | Active Agent | Indication | Key Advancement |
|---|---|---|---|---|
| Onivyde | Liposomal | Irinotecan | Pancreatic cancer | Improved circulation and tumor accumulation [102] |
| Vyxeos | Liposomal | Cytarabine/Daunorubicin | Acute myeloid leukemia | Co-encapsulation of two chemotherapeutic agents [102] |
| Apealea | Polymeric | Paclitaxel | Ovarian cancer | EPR-mediated passive targeting [103] |
| COVID-19 mRNA Vaccines | Lipid-based | mRNA | SARS-CoV-2 prevention | mRNA protection and cellular delivery [102] |
The diversity of approved nanomedicine platforms demonstrates the versatility of nanotechnology in drug delivery. Analysis reveals that among recently approved nanomedicines, polymeric nanoparticles constitute approximately 29%, liposomal formulations 22%, and lipid-based nanoparticles 21% [102]. This distribution highlights the continued dominance of organic nanoparticle platforms in clinical translation, largely attributable to their favorable biocompatibility and biodegradability profiles.
Quantitative Analysis of Clinical Trials
Table 2: Nanomedicine Clinical Trials Analysis (2002-2021, n=486 trials) [102]
| Parameter | Distribution | Key Observations |
|---|---|---|
| Nanoparticle Types | Liposomes (44%), Protein-based (26%), Polymeric (14%), Metal-based (11%), Others (5%) | Liposomes dominate clinical investigation landscape |
| Therapeutic Content | Paclitaxel (23%), Metals (11%), Doxorubicin (9%), Bupivacaine (8%), Vaccines (8%) | Oncology drugs remain primary payload |
| Clinical Trial Phases | Phase I (32%), Phase II (41%), Phase III (18%), Phase IV (9%) | Balanced progression through development pipeline |
| Therapeutic Areas | Oncology (68%), Infectious Diseases (14%), Cardiovascular (8%), Neurology (6%), Others (4%) | Clear focus on cancer applications |
The data reveals several important trends. First, the substantial representation of vaccine platforms (8%) reflects growing application of nanotechnology in immunotherapeutics, further accelerated by the success of COVID-19 mRNA vaccines [102]. Second, the progression of nanomedicines through clinical phases demonstrates viability, with 18% of trials reaching Phase III, indicating strong translation potential.
Analysis of Clinical Trial Outcomes: Successes and Challenges
Efficacy Endpoints in Oncology Trials
Cancer nanomedicines have demonstrated significant improvements in therapeutic outcomes through enhanced drug delivery. The enhanced permeability and retention (EPR) effect, first described in 1986, remains a fundamental principle for passive tumor targeting [103]. This phenomenon exploits the leaky vasculature and impaired lymphatic drainage characteristic of solid tumors, allowing preferential accumulation of nanoscale particles (typically 10-200 nm) in tumor tissue [101] [103].
Clinical evidence confirms that leveraging EPR effect translates to improved efficacy. Liposomal doxorubicin (Doxil) demonstrates reduced cardiotoxicity while maintaining anticancer efficacy compared to free doxorubicin [101]. Similarly, albumin-bound paclitaxel (Abraxane) shows enhanced response rates in metastatic breast cancer (33% vs 19%) compared to solvent-based paclitaxel, attributed to improved tumor targeting and drug delivery [104].
Analysis of Failure Modes in Clinical Development
Despite promising preclinical data, some nanomedicine candidates have encountered challenges in clinical trials. Common limitations include:
- Heterogeneous EPR effect: Significant patient-to-patient variability in tumor vasculature limits consistent nanoparticle accumulation [103]
- Immunological reactions: Accelerated blood clearance, particularly upon repeated administration of PEGylated nanoparticles, can reduce efficacy [105]
- Biological barriers: Tumor stroma, high interstitial pressure, and cellular barriers impede uniform distribution [101]
- Scale-up challenges: Manufacturing inconsistencies between preclinical and clinical batches alter critical quality attributes [106]
Recent approaches address these limitations through multi-stage targeting strategies that incorporate stimuli-responsive elements (pH, enzymes, redox) and active targeting ligands [100] [103].
Experimental Protocols for Nanomedicine Characterization
Rigorous characterization is essential for nanomedicine development. The Nanotechnology Characterization Laboratory (NCL) has established standardized analytical cascades to support regulatory submissions [105].
Physicochemical Characterization Protocol
Objective: Comprehensive analysis of critical quality attributes including size, surface charge, composition, and stability.
Methodology:
- Size and Size Distribution Analysis (PCC-1)
- Utilize batch-mode dynamic light scattering (DLS)
- Perform measurements at 25°C with appropriate viscosity corrections
- Conduct minimum 3 measurements with 10-15 runs each
- Report hydrodynamic diameter (Z-average) and polydispersity index (PDI)
Surface Charge Determination (PCC-2)
- Measure zeta potential via phase analysis light scattering
- Use appropriate electrolyte solution (e.g., 1mM KCl)
- Perform minimum 5 measurements with 10-100 cycles each
Morphological Analysis (PCC-7)
- Prepare samples by negative staining with uranyl acetate
- Image using transmission electron microscopy (TEM) at 75-100 kV
- Analyze multiple fields to ensure representative sampling
Chemical Composition Assessment (PCC-14, PCC-18)
- Quantify active pharmaceutical ingredient using validated HPLC/UV-Vis
- Determine drug loading capacity and encapsulation efficiency
- Assess residual solvents and impurities
Acceptance Criteria: Size PDI <0.3, zeta potential >|±10| mV for colloidal stability, encapsulation efficiency >80%, residual solvents within ICH limits [105].
In Vitro Immunotoxicity Assessment Protocol
Objective: Evaluation of nanoparticle interactions with immune components to predict potential adverse reactions.
Methodology (ITA-1, ITA-5.2, ITA-27):
- Hemocompatibility Testing
- Incubate nanoparticles with fresh human blood at 37°C for 1 hour
- Centrifuge and measure hemoglobin release at 540 nm
- Calculate hemolysis percentage relative to positive control
Complement Activation Assessment
- Incubate nanoparticles with human serum for 1 hour at 37°C
- Quantify SC5b-9 complex via enzyme immunoassay
- Report fold-increase compared to negative control
Cytokine Profiling
- Expose human peripheral blood mononuclear cells (PBMCs) to nanoparticles
- After 24 hours, collect supernatant and analyze using multiplex ELISA
- Quantify key cytokines: IL-1β, IL-6, IL-8, TNF-α, IFN-γ
Acceptance Criteria: Hemolysis <10%, complement activation <2-fold increase, no significant cytokine induction (>2-fold) versus control [105].
Visualization of Nanomedicine Clinical Translation
Diagram 1: Nanomedicine Clinical Translation Cascade illustrates the critical pathway from preclinical development to commercialization, highlighting key decision points and regulatory milestones.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Nanomedicine Development
| Reagent/Category | Function | Application Examples | References |
|---|---|---|---|
| Polyethylene glycol (PEG) | Stealth coating to reduce opsonization and extend circulation half-life | PEGylated liposomes (Doxil), lipid nanoparticles | [102] [101] |
| Phospholipids | Structural components for liposomal and lipid-based nanoparticles | Liposome formation, membrane functionalization | [55] [102] |
| Biodegradable polymers (PLGA, PLA) | Polymeric nanoparticle matrix for controlled drug release | Sustained release formulations, implantable systems | [55] [101] |
| Targeting ligands (peptides, antibodies, aptamers) | Active targeting to specific cellular receptors | Transferrin, folate, EGFR antibodies, RGD peptides | [101] [103] |
| Stimuli-responsive materials (pH-sensitive, redox-sensitive) | Triggered drug release in response to biological cues | pH-sensitive liposomes, glutathione-responsive dendrimers | [100] [103] |
| Characterization standards (NCL protocols) | Standardized assessment of critical quality attributes | Physicochemical characterization, immunotoxicity testing | [105] |
Emerging Trends and Future Perspectives
The nanomedicine field continues to evolve with several emerging trends shaping future development:
- Multi-stage targeting systems: New generation nanomedicines incorporate transformable properties, enabling initial accumulation via EPR followed by size reduction or charge reversal for improved penetration [103]
- Biomimetic approaches: Cell membrane-coated nanoparticles leverage inherent homing capabilities for enhanced targeting [103]
- Integration with immunotherapy: Nanoparticles designed to modulate immune responses show promise in combination therapies [100] [103]
- Artificial intelligence: AI-assisted design and optimization of nanoparticles accelerates development and predicts in vivo performance [103]
- Organelle-specific targeting: Third-generation nanotherapeutics focus on subcellular delivery to mitochondria, nuclei, or lysosomes [103]
The continued translation of nanomedicines from bench to bedside will require multidisciplinary collaborations across academia, pharmaceutical industry, and regulatory agencies. By addressing current challenges in manufacturing scalability, characterization standardization, and patient stratification, the field is poised to deliver increasingly sophisticated targeted therapeutic platforms that maximize efficacy while minimizing adverse effects.
The application of nanotechnology in drug delivery represents a paradigm shift in cancer treatment, offering solutions to enhance therapeutic efficacy while reducing systemic toxicity. By exploiting unique physicochemical properties at the nanoscale (typically 1-100 nm), nanocarriers can improve drug solubility, extend circulation half-life, and enable targeted delivery to tumor tissues through passive and active mechanisms [107] [108]. The Enhanced Permeability and Retention (EPR) effect, a cornerstone of passive targeting, leverages the leaky vasculature and impaired lymphatic drainage of tumors to facilitate nanocarrier accumulation [109] [108]. Active targeting further enhances specificity through surface-functionalized ligands that bind to receptors overexpressed on cancer cells [107] [109].
This application note examines two seminal success stories in nanomedicine—Doxil and Abraxane—and one notable clinical setback, BIND-014. By analyzing their quantitative outcomes, experimental methodologies, and underlying biological mechanisms, this document provides a framework for researchers developing targeted nanotherapeutic systems.
Success Case Study: Doxil (PEGylated Liposomal Doxorubicin)
Background and Formulation Strategy
Doxil was the first FDA-approved nanomedicine, representing a breakthrough in liposomal technology. This PEGylated liposomal formulation encapsulates the anthracycline antibiotic doxorubicin, a natural-product-derived chemotherapeutic agent with potent antitumor activity [110]. The conventional formulation of doxorubicin (Adriamycin) demonstrates efficacy against a broad spectrum of malignancies but causes severe side effects, particularly dose-limiting cardiotoxicity and myelosuppression [110].
The Doxil nanocarrier system addresses these limitations through:
- Stealth Liposome Design: Polyethylene glycol (PEG) coating creates a hydrophilic layer that reduces opsonization and recognition by the mononuclear phagocyte system (MPS), significantly extending plasma half-life [107] [110].
- Stable Drug Encapsulation: An ammonium sulfate gradient enables efficient doxorubicin loading and retention within liposomes until tumor site delivery [110].
- EPR Exploitation: The nanoscale size (approximately 100 nm) facilitates extravasation through leaky tumor vasculature, preferentially accumulating in tumor tissue [109].
Quantitative Clinical Outcomes
Table 1: Clinical Performance Metrics of Doxil vs. Conventional Doxorubicin
| Parameter | Doxil | Conventional Doxorubicin |
|---|---|---|
| Dosing Regimen | 40-75 mg/m² every 4 weeks | 40-75 mg/m² every 3 weeks |
| Maximum Tolerated Dose (Cumulative) | Not established; higher cumulative doses possible | 300-500 mg/m² (due to cardiotoxicity) |
| Plasma Half-Life | Approximately 55-80 hours | 5-10 minutes (initial), 30 hours (terminal) |
| Primary Indications | AIDS-related Kaposi's sarcoma, ovarian cancer, multiple myeloma | Wide spectrum of hematologic and solid tumors |
| Cardiotoxicity Profile | Significantly reduced incidence and severity | Dose-limiting, cumulative cardiotoxicity |
| Hand-Foot Syndrome | Increased incidence (dose-limiting toxicity) | Not typically associated |
Experimental Protocol: Liposomal Formulation and Characterization
Objective: Prepare and characterize PEGylated liposomal doxorubicin for preclinical evaluation.
Materials:
- Hydrogenated soy phosphatidylcholine (HSPC)
- Cholesterol
- Distearoylphosphatidylethanolamine-PEG (DSPE-PEG)
- Doxorubicin hydrochloride
- Ammonium sulfate solution
- Sephadex G-50 column
Methodology:
Lipid Film Formation:
- Dissolve HSPC, cholesterol, and DSPE-PEG (molar ratio 3:2:0.3) in chloroform in a round-bottom flask.
- Remove organic solvent by rotary evaporation at 40°C to form a thin lipid film.
- Maintain under vacuum overnight to ensure complete solvent removal.
Hydration and Extrusion:
- Hydrate lipid film with 250 mM ammonium sulfate solution (pH 5.5) at 65°C with agitation.
- Subject the multilamellar vesicle suspension to 5 freeze-thaw cycles (liquid nitrogen/65°C water bath).
- Extrude sequentially through polycarbonate membranes (0.4 μm, 0.2 μm, 0.1 μm, and 0.08 μm) using a high-pressure extruder.
Remote Loading:
- Create transmembrane ammonium sulfate gradient by dialyzing against iso-osmotic sucrose solution.
- Incubate blank liposomes with doxorubicin solution (drug-to-lipid ratio 0.2:1 w/w) at 60°C for 30 minutes.
- Remove unencapsulated drug by gel filtration (Sephadex G-50) or dialysis.
Quality Control:
- Determine particle size and polydispersity index by dynamic light scattering.
- Measure zeta potential using electrophoretic light scattering.
- Quantify drug encapsulation efficiency via HPLC after liposome disruption with Triton X-100.
- Assess in vitro drug release profile using dialysis against PBS (pH 7.4) at 37°C.
Validation: The formulation should exhibit mean particle size of 80-100 nm, polydispersity index <0.1, encapsulation efficiency >90%, and sustained release profile (<10% release in 24 hours).
Success Case Study: Abraxane (Albumin-Bound Paclitaxel)
Background and Formulation Strategy
Abraxane represents an innovative protein-based nanoparticle approach that overcomes significant limitations of conventional paclitaxel formulation. Paclitaxel, a natural product derived from the Pacific yew tree, promotes microtubule stabilization and cell cycle arrest [110]. The conventional formulation uses Cremophor EL as a solubilizing agent, which causes severe hypersensitivity reactions and necessitates premedication with steroids and antihistamines [110].
The Abraxane platform employs:
- Albumin Nanotechnology: 130-nm nanoparticles created through high-pressure homogenization of paclitaxel with human serum albumin.
- Natural Transport Mechanism: Exploits albumin's natural affinity for gp60 receptors and caveolae-mediated transcytosis across endothelial cells.
- Tumor-Targeting Pathway: Albumin binds to secreted protein acidic and rich in cysteine (SPARC), overexpressed in many tumors, further enhancing drug accumulation [110].
Quantitative Clinical Outcomes
Table 2: Clinical Performance Metrics of Abraxane vs. Conventional Paclitaxel
| Parameter | Abraxane | Conventional Paclitaxel |
|---|---|---|
| Formulation Composition | Albumin-bound paclitaxel nanoparticles | Paclitaxel in Cremophor EL/ethanol |
| Recommended Dose | 260 mg/m² every 3 weeks (monotherapy) | 175 mg/m² every 3 weeks |
| Infusion Time | 30 minutes without premedication | 3 hours with steroid/antihistamine premedication |
| Vehicle-Related Toxicity | No Cremophor EL-related hypersensitivity | Significant hypersensitivity risk |
| Tumor Response Rate (Metastatic Breast Cancer) | 33% (vs. 19% for paclitaxel) | 19% (phase III trial) |
| Neutropenia Incidence | Lower incidence of severe neutropenia | Higher incidence of severe neutropenia |
Experimental Protocol: Albumin-Nanoparticle Preparation and Evaluation
Objective: Develop and characterize albumin-bound paclitaxel nanoparticles for intravenous administration.
Materials:
- Paclitaxel
- Human serum albumin (HSA)
- Saline for injection
- High-pressure homogenizer
- Lyophilizer
- MALDI-TOF mass spectrometer
Methodology:
Nanoparticle Formation:
- Prepare 1-5% (w/v) HSA solution in saline.
- Add paclitaxel to HSA solution (final drug:albumin ratio ~1:9 w/w).
- Subject mixture to high-pressure homogenization (15,000-30,000 psi) for 5-10 cycles.
- Filter sterilize through 0.22 μm filter under aseptic conditions.
Lyophilization:
- Add cryoprotectant (e.g., sucrose or trehalose) to nanoparticle suspension.
- Freeze at -80°C for 2 hours.
- Lyophilize for 24-48 hours until complete moisture removal.
Reconstitution and Characterization:
- Reconstitute lyophilized powder with sterile saline to desired concentration.
- Determine particle size distribution and zeta potential by dynamic light scattering.
- Assess particle morphology by transmission electron microscopy.
- Quantify drug content and encapsulation efficiency by HPLC.
In Vitro Biological Activity:
- Evaluate cytotoxicity against cancer cell lines (e.g., MCF-7, MDA-MB-231) using MTT assay.
- Compare cellular uptake of albumin nanoparticles vs. free drug using fluorescent microscopy.
- Assess tubulin polymerization activity in cell-free systems.
Validation: The final product should have mean particle size of 120-150 nm, >99% drug binding efficiency, and sterility according to USP standards. Reconstitution time should be <15 minutes.
Failure Case Study: BIND-014 (PSMA-Targeted Docetaxel Nanoparticle)
Background and Development Strategy
BIND-014 represents an advanced actively targeted nanotherapeutic that failed to progress beyond phase 2 clinical trials despite promising preclinical data. This docetaxel-encapsulating polymeric nanoparticle incorporated:
- Active Targeting Ligands: Small-molecule inhibitors of prostate-specific membrane antigen (PSMA) for tumor-specific homing.
- Controlled Release Polymer Matrix: Poly(lactic-co-glycolic acid) (PLGA) for sustained drug release.
- Stealth Properties: Polyethylene glycol (PEG) corona to prolong circulation time [111] [112].
The therapeutic rationale focused on PSMA overexpression in prostate cancer cells and tumor neovasculature, hypothesizing that targeted delivery would enhance efficacy while reducing docetaxel's characteristic toxicities (neutropenia, peripheral neuropathy) [111].
Quantitative Clinical Outcomes
Table 3: Clinical Performance Metrics of BIND-014 in mCRPC
| Parameter | BIND-014 Results | Historical Benchmark (Standard Docetaxel) |
|---|---|---|
| Patient Population | Chemotherapy-naive metastatic castration-resistant prostate cancer (mCRPC) | Chemotherapy-naive mCRPC |
| Dosing Regimen | 60 mg/m² every 21 days | 75 mg/m² every 21 days |
| Median Radiographic PFS | 9.9 months | 8-10 months (docetaxel + prednisone) |
| PSA Response (≥50% reduction) | 30% (12/40 patients) | 45-65% |
| Objective Response Rate (Measurable Disease) | 32% (6/19 patients) | 12-48% (varies by study) |
| CTC Conversion (≥5 to <5 cells/7.5 mL) | 50% (13/26 patients) | 27-65% (varies by study) |
| Most Common Adverse Events | Fatigue (69%), nausea (55%), neuropathy (33%) | Neutropenia, fatigue, neuropathy |
Despite meeting its primary endpoint in phase 2 trials (median radiographic progression-free survival of 9.9 months), BIND-014 demonstrated only modest clinical activity that failed to show clear superiority over standard docetaxel in an evolving treatment landscape with new anti-androgen therapies [111] [112]. Development was discontinued due to insufficient competitive advantage.
Experimental Protocol: Targeted Polymeric Nanoparticle Development
Objective: Develop and evaluate PSMA-targeted docetaxel nanoparticles for prostate cancer therapy.
Materials:
- PLGA (50:50, acid-terminated)
- Docetaxel
- PEG-PLGA block copolymer with terminal carboxylic acid groups
- PSMA-targeting small molecule ligand (e.g., DUPA peptide or glutamate-urea-lysine analog)
- N-hydroxysuccinimide (NHS)
- N-(3-Dimethylaminopropyl)-N'-ethylcarbodiimide (EDC)
- Dichloromethane
Methodology:
Nanoparticle Preparation:
- Dissolve PLGA, PEG-PLGA, and docetaxel (10-15% w/w) in dichloromethane.
- Emulsify in aqueous polyvinyl alcohol solution using probe sonication.
- Evaporate organic solvent under reduced pressure with stirring.
- Collect nanoparticles by ultracentrifugation and wash to remove stabilizer.
Surface Functionalization:
- Activate terminal carboxylic acids on PEG-PLGA with EDC/NHS chemistry.
- Incubate with PSMA-targeting ligand (amine-terminated) at pH 8.5 for 4 hours.
- Purify by centrifugation and characterize conjugation efficiency.
In Vitro Characterization:
- Determine particle size, PDI, and zeta potential by dynamic light scattering.
- Quantify drug loading and encapsulation efficiency by HPLC.
- Assess in vitro drug release profile in PBS (pH 7.4) with 0.1% Tween 80.
- Evaluate targeting specificity using PSMA-positive (LNCaP) vs. PSMA-negative (PC-3) prostate cancer cells.
In Vivo Evaluation:
- Establish prostate cancer xenograft models (LNCaP and PC-3).
- Administer fluorescently labeled targeted vs. non-targeted nanoparticles.
- Quantify biodistribution and tumor accumulation using fluorescence imaging.
- Evaluate antitumor efficacy by monitoring tumor volume and survival.
Validation: Targeted nanoparticles should show ≥2-fold higher cellular uptake in PSMA-positive cells vs. non-targeted controls and ≥3-fold higher tumor accumulation in xenograft models compared to non-targeted nanoparticles.
Comparative Analysis and Mechanistic Insights
Critical Success Factors in Nanomedicine Development
The contrasting outcomes of Doxil/Abraxane versus BIND-014 reveal key determinants of nanomedicine success:
- Robust Passive Targeting Foundation: Both Doxil and Abraxane primarily rely on EPR effect and physiological targeting, whereas BIND-014's active targeting required prior passive accumulation for optimal function [107] [109].
- Formulation-Driven Toxicity Mitigation: Doxil and Abraxane successfully addressed specific, severe toxicities of their parent drugs (cardiotoxicity and hypersensitivity, respectively), providing clear clinical advantages [110].
- Patient Selection and Biomarker Strategy: BIND-014 development highlighted the importance of patient stratification based on target expression (PSMA on circulating tumor cells), though this approach proved insufficient for clinical success [111].
Visualization of Nanocarrier Targeting Mechanisms
Diagram 1: Nanocarrier Targeting Mechanisms. Passive targeting exploits the Enhanced Permeability and Retention (EPR) effect in tumor vasculature, while active targeting utilizes surface ligands for specific receptor binding and cellular internalization [107] [109] [108].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Nanomedicine Development
| Reagent Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Polymer Materials | PLGA, PEG-PLGA, HPMA | Nanoparticle matrix providing controlled release and stealth properties | Varying molecular weights and block compositions modulate degradation kinetics and drug release profiles |
| Lipid Components | HSPC, DSPE-PEG, Cholesterol | Liposome formation and stabilization | PEG-lipids confer stealth properties; cholesterol enhances membrane stability |
| Targeting Ligands | Folate, DUPA peptide, RGD peptide, Transferrin | Surface functionalization for active targeting | Selection based on receptor expression profile in target disease; consideration of ligand density and orientation |
| Characterization Tools | Dynamic Light Scattering, HPLC, TEM, MALDI-TOF | Physicochemical characterization of nanocarriers | Comprehensive characterization essential for regulatory compliance and batch-to-batch consistency |
| Biological Assays | Cell viability assays, Flow cytometry, Confocal microscopy | In vitro evaluation of targeting and efficacy | Use of relevant cell lines with target receptor expression; inclusion of appropriate controls |
| Animal Models | Xenograft models, Orthotopic models, Patient-derived xenografts | In vivo efficacy and biodistribution studies | Consideration of model relevance to human disease and EPR effect representation |
The case studies presented herein demonstrate that successful clinical translation of nanomedicines requires addressing clear clinical limitations of existing therapies, leveraging robust passive targeting mechanisms, and establishing straightforward, scalable manufacturing processes. While active targeting strategies hold theoretical promise, their clinical implementation faces significant barriers including tumor heterogeneity, biological complexity, and manufacturing challenges [109].
Future nanomedicine development should focus on:
- Patient stratification strategies based on target expression and EPR effect potential
- Multifunctional systems that combine sequential targeting mechanisms
- Advanced characterization techniques to better understand nano-bio interactions
- Scalable manufacturing processes that ensure batch-to-batch consistency
These case studies provide valuable frameworks for researchers designing next-generation nanotherapeutic systems with enhanced potential for clinical translation and impact.
The integration of nanotechnology into pharmaceutical development has introduced transformative advancements in targeted drug delivery systems, enabling precision medicine through enhanced bioavailability, controlled release, and reduced systemic toxicity. These Nanotechnology-Enabled Health Products (NHPs) present unique regulatory challenges due to their complex physicochemical properties and novel mechanisms of action. Regulatory agencies including the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) have established evolving frameworks to ensure the safety, efficacy, and quality of these innovative therapeutics while fostering scientific advancement [113]. The global nanotechnology drug delivery market, valued at $97.98 billion in 2024, is projected to reach $231.7 billion by 2035, reflecting the significant growth and investment in this sector [114].
Regulatory navigation for NHPs remains complex, often creating barriers to clinical application despite their revolutionary potential. This document provides detailed application notes and experimental protocols structured within the context of targeted drug delivery research, specifically addressing the regulatory requirements for nanotechnology-enabled products. The frameworks emphasize a product-focused, science-based approach that necessitates comprehensive characterization and evidence generation throughout the development lifecycle [115] [113]. Understanding these pathways is essential for researchers and drug development professionals aiming to translate nanomedicine innovations from laboratory research to clinical applications.
Comparative Regulatory Frameworks: FDA vs. EMA
Foundational Regulatory Approaches
The FDA and EMA approach NHP regulation through distinct yet complementary frameworks designed to address the unique challenges posed by nanoscale materials. Both agencies participate in international harmonization efforts while maintaining region-specific requirements that reflect their legal mandates and public health priorities.
The FDA regulates nanotechnology products through a flexible, product-focused framework based on existing statutory authorities. The agency participates in the National Nanotechnology Initiative (NNI), coordinating multi-agency efforts in nanoscale science, engineering, and technology [115]. The FDA's approach emphasizes regulatory science research to build knowledge and facilitate innovation while ensuring product safety. The agency has issued several guidance documents covering nanotechnology products across various categories, including drugs, devices, and combination products, with the goal of providing transparent and predictable regulatory pathways [116].
The EMA operates under a more centralized framework for medicinal products, with nanomedicines falling under specific scientific guidelines. The definition of a nanomedicine according to EMA requires systems to be manufactured for clinical applications with at least one component at the nanoscale, possessing properties that provide clinical advantages related to nanoengineering and size [117]. The European regulatory landscape is further shaped by the Nanotechnology-based Medicinal Products for Human Use EU Innovation Network (EU-IN) Horizon Scanning Report, which identifies emerging trends and helps regulators prepare for technological developments [118].
Table 1: Comparative Analysis of FDA and EMA Regulatory Frameworks for Nanotechnology-Enabled Drug Products
| Aspect | U.S. FDA Approach | EU EMA Approach |
|---|---|---|
| Legal Basis | Existing statutory authorities; product-specific guidance | Directive 2001/83/EC; nanomedicine-specific guidelines |
| Definition | Flexible, science-based; considers dimension 1-100nm and nanoscale properties/appearance | Engineered systems with at least one nanoscale component; specific properties conferring clinical advantage |
| Guidance Documents | Multiple product-specific guidances; "case-by-case" basis encouraged | Scientific guidelines on nanomedicines for marketing authorization applications |
| Quality Assessment | Pharmaceutical quality assessment requiring extensive characterization | Quality-by-design approaches; emphasis on critical quality attributes |
| Non-Clinical Requirements | Conventional toxicology approach with adaptations for nanomaterial properties | Conventional toxicology with special attention to immunotoxicity and distribution |
| Clinical Assessment | Standard clinical trials with focus on immunotoxicological effects (e.g., CARPA syndrome) | Benefit-risk balance assessment with vigilance for pseudo-allergic responses |
Regulatory Classification and Pathways
NHPs are primarily categorized as either medicinal products or medical devices based on their principal mechanism of action. Medicinal products achieve their intended purpose through pharmacological, immunological, or metabolic (PIM) mechanisms, while medical devices function predominantly through physical or mechanical means [113]. This distinction is critical for determining the appropriate regulatory pathway and data requirements.
In the EU, obtaining marketing authorization is mandatory for all medicinal products containing nanomaterials, with applications submitted through centralized, decentralized, or national procedures depending on the product characteristics [119]. The FDA maintains a product-specific, risk-based approach where nanotechnology products are regulated according to their primary mode of action, with combination products assigned to lead centers based on their primary therapeutic effect [115].
Characterization Protocols for Nanotechnology-Enabled Drug Products
Physicochemical Characterization Methodology
Comprehensive physicochemical characterization forms the foundation of quality assessment for NHPs. Regulatory agencies require extensive data on critical quality attributes (CQAs) that may influence the product's safety and performance profile. The following experimental protocol outlines the essential characterization workflow for nanotechnology-enabled drug products.
Protocol 1: Comprehensive Physicochemical Characterization of Nanomaterials
Objective: To systematically characterize the physicochemical properties of nanotechnology-enabled drug products according to regulatory requirements.
Materials and Equipment:
- Nanomaterial sample (lyophilized or in suspension)
- Dynamic Light Scattering (DLS) instrument
- Nanoparticle Tracking Analysis (NTA) system
- Scanning Electron Microscope (SEM)
- Transmission Electron Microscope (TEM)
- Zeta potential analyzer
- Fourier-Transform Infrared Spectroscopy (FTIR) instrument
- X-ray Photoelectron Spectroscopy (XPS) system
- X-ray Diffractometer (XRD)
- Surface area analyzer (BET method)
Procedure:
Sample Preparation
- Prepare nanomaterial suspensions using standardized dispersion protocols in relevant biological buffers.
- Include sonication steps where appropriate to minimize aggregation (e.g., probe sonication at specific energy inputs).
- Document all preparation parameters including temperature, pH, and buffer composition.
Size Distribution Analysis
- Perform DLS measurements at multiple angles (e.g., 90° and 173°) to determine hydrodynamic diameter and polydispersity index.
- Conduct NTA to obtain particle concentration and size distribution based on Brownian motion.
- Validate results using SEM/TEM imaging to confirm primary particle size and identify morphological features.
Surface Characterization
- Measure zeta potential using electrophoretic light scattering across physiological pH range (pH 5.0-8.0).
- Perform FTIR spectroscopy to identify surface functional groups and coating materials.
- Conduct XPS analysis to determine elemental composition and chemical states at the material surface.
Structural Analysis
- Use XRD to determine crystalline structure, phase composition, and crystallite size.
- Perform SAXS for additional structural information on particle size distribution and shape.
Stability Assessment
- Monitor size, zeta potential, and appearance over time under various storage conditions (accelerated stability studies).
- Assess aggregation propensity in biologically relevant media (e.g., plasma, PBS).
- Characterize protein corona formation by incubating with plasma and analyzing adsorbed proteins via SDS-PAGE or LC-MS.
Data Interpretation and Regulatory Considerations:
- Establish acceptance criteria for CQAs based on quality-by-design principles.
- Document all method validation parameters including precision, accuracy, and robustness.
- Provide justification for the selection of characterization methods relative to the nanomaterial properties.
- Include orthogonal methods where appropriate to confirm key attributes.
Table 2: Essential Characterization Techniques for Nanotechnology-Enabled Drug Products
| Characterization Parameter | Recommended Techniques | Regulatory Purpose | Acceptance Criteria Considerations |
|---|---|---|---|
| Size Distribution | DLS, NTA, SEM, TEM | Batch consistency, biodistribution prediction | PDI < 0.3 (monodisperse), size range appropriate for intended application |
| Surface Charge | Zeta potential | Stability prediction, interaction with biological systems | ±30 mV for colloidal stability, charge appropriate for targeting |
| Morphology | TEM, SEM, AFM | Structure-function relationship, manufacturing control | Consistent shape, absence of aggregates, defined architecture |
| Surface Chemistry | XPS, FTIR, Raman | Batch consistency, functional group quantification | Confirmation of surface modifications, quantification of ligands |
| Crystalline Structure | XRD, SAXS | Stability, dissolution rate, toxicity assessment | Phase identification, crystallite size calculation |
| Surface Area | BET method | Reactivity, drug loading capacity | Correlation with particle size, internal structure assessment |
Research Reagent Solutions for Nanomaterial Characterization
Table 3: Essential Research Reagents for Nanomaterial Characterization
| Reagent/Material | Function | Application Context |
|---|---|---|
| Phosphate Buffered Saline (PBS) | Dispersion medium | Provides physiological ionic strength for stability testing |
| Fetal Bovine Serum (FBS) | Protein source | Protein corona formation studies in biological fluids |
| Polysorbate 80 (Tween 80) | Surfactant | Prevents aggregation during dispersion and storage |
| Dialysis Membranes | Separation | Studies of drug release kinetics under sink conditions |
| Size Exclusion Chromatography Columns | Purification | Separation of free drug from encapsulated formulations |
| Cryo-EM Grids | Sample preparation | Preservation of native state for morphological analysis |
| FTIR Calibration Standards | Instrument calibration | Ensures accuracy of chemical identification |
| Zeta Potential Transfer Standards | Method validation | Verifies instrument performance for surface charge measurements |
Safety and Efficacy Assessment Protocols
Immunotoxicity Evaluation
Immunotoxicity represents a critical safety consideration for NHPs due to their potential interaction with immune system components. Regulatory agencies require comprehensive assessment of immunotoxicological effects, particularly complement activation-related pseudoallergy (CARPA syndrome), which has been reported with various nanomaterial systems [117].
Protocol 2: Immunotoxicity Assessment for Nanotechnology-Enabled Drug Products
Objective: To evaluate potential immunotoxic effects of nanotechnology-enabled drug products, including complement activation and cytokine release.
Materials and Equipment:
- Human whole blood or primary immune cells (PBMCs)
- Complement activation assay kits (C3a, C5a, SC5b-9)
- Cytokine multiplex assay (TNF-α, IL-1β, IL-6, IL-8)
- Flow cytometer with appropriate antibodies
- Animal models (e.g., porcine CARPA model)
- Hematology analyzer
- Histopathology equipment
Procedure:
In Vitro Complement Activation
- Incubate NHP with fresh human serum (pooled from multiple donors) at 37°C for 60 minutes.
- Use zymosan as positive control and PBS as negative control.
- Measure complement activation products (C3a, C5a, SC5b-9) using ELISA according to manufacturer protocols.
- Express results as percentage activation relative to positive control.
Cytokine Release Profiling
- Isolate human PBMCs from healthy donors using density gradient centrifugation.
- Expose PBMCs to NHP at concentrations reflecting anticipated clinical exposure.
- Collect supernatant at 6, 24, and 48 hours for cytokine analysis.
- Quantify pro-inflammatory cytokines (TNF-α, IL-1β, IL-6, IL-8) using multiplex immunoassays.
- Compare against reference standards and positive controls (LPS).
Cellular Uptake and Phagocytosis
- Differentiate THP-1 cells to macrophage-like state using PMA treatment.
- Incubate with fluorescently labeled NHP for predetermined time points.
- Analyze cellular internalization using flow cytometry and confocal microscopy.
- Quantify mean fluorescence intensity and percentage of positive cells.
In Vivo Immunotoxicity Assessment
- Administer NHP to appropriate animal models (rodent and non-rodent where indicated).
- Monitor acute physiological responses indicative of CARPA syndrome (pulmonary hypertension, leukopenia, thrombocytopenia).
- Collect blood samples for hematological analysis and complement activation markers.
- Perform histopathological examination of lymphoid tissues (spleen, lymph nodes, bone marrow).
Data Interpretation and Regulatory Considerations:
- Establish dose-response relationships for immunotoxic effects.
- Compare against comparator products where available.
- Provide justification for selected models and endpoints based on product characteristics.
- Include positive and negative controls in all assay systems.
Pharmacokinetics and Biodistribution Studies
The pharmacokinetic profile of NHPs often differs significantly from conventional formulations due to altered absorption, distribution, metabolism, and excretion (ADME) properties. Regulatory agencies require comprehensive ADME studies that account for the unique characteristics of nanoscale materials [113].
Protocol 3: Biodistribution and Pharmacokinetic Assessment of NHPs
Objective: To characterize the in vivo fate of nanotechnology-enabled drug products, including tissue distribution, clearance pathways, and persistence.
Materials and Equipment:
- Radiolabeled or fluorescently labeled NHP (e.g., 14C, 125I, DiR dyes)
- Animal models relevant to disease indication
- IVIS imaging system or gamma counter
- LC-MS/MS system for quantitative analysis
- Tissue homogenization equipment
Procedure:
Labeling and Tracer Selection
- Incorporate radiolabels during manufacturing (preferred) or use surface labeling methods.
- Validate that labeling does not alter physicochemical properties or biological behavior.
- Include both drug substance and carrier labels where appropriate to distinguish carrier and active moiety.
Tissue Distribution Study
- Administer labeled NHP to animals via intended clinical route.
- Euthanize animals at predetermined time points (e.g., 0.5, 2, 8, 24, 72, 168 hours).
- Collect tissues of interest (liver, spleen, kidneys, lungs, heart, brain, tumor).
- Quantify radioactivity or fluorescent signal in tissues using appropriate methods.
- Express results as percentage of injected dose per gram of tissue.
Pharmacokinetic Profiling
- Collect blood samples at multiple time points following administration.
- Process samples to separate plasma and cellular components.
- Measure concentration of both encapsulated and released drug using validated bioanalytical methods.
- Calculate standard pharmacokinetic parameters (AUC, Cmax, Tmax, t1/2, clearance).
Clearance and Metabolism Studies
- Collect excreta (urine, feces) over specified time periods.
- Analyze for parent compound and metabolites.
- Assess potential for organ accumulation with extended dosing regimens.
Data Interpretation and Regulatory Considerations:
- Correlate biodistribution data with efficacy and toxicity observations.
- Identify potential sites of accumulation that may inform clinical monitoring strategies.
- Compare pharmacokinetic parameters against non-nanoformulated counterparts.
- Provide justification for dose selection and sampling time points.
Regulatory Submission Strategy
Chemistry, Manufacturing, and Controls (CMC) Requirements
The CMC section for nanotechnology-enabled drug products requires extensive documentation of manufacturing processes, quality control measures, and comprehensive characterization data. Regulatory agencies emphasize quality-by-design approaches and thorough understanding of critical process parameters that influence critical quality attributes [117].
Key CMC Documentation Elements:
- Manufacturing Process Description
- Detailed synthesis/purification methods with defined critical process parameters
- Scale-up considerations and process validation data
- Control strategies for batch-to-batch consistency
Quality Control Testing
- Release specifications with justified acceptance criteria
- Stability data under recommended storage conditions
- Characterization of drug product in its intended delivery vehicle
Comparability Protocols
- Strategies for managing manufacturing changes
- Analytical similarity assessments for post-change product
- Justification for waiving additional non-clinical or clinical studies
Non-Clinical and Clinical Development Considerations
The non-clinical development of NHPs should address potential nano-specific toxicity concerns while generating robust efficacy data. Regulatory agencies recommend a case-by-case approach based on product characteristics, route of administration, and intended patient population [117] [119].
Integrated Non-Clinical Testing Strategy:
- Safety Pharmacology - Core battery tests with emphasis on cardiovascular and pulmonary systems
- Repeat-Dose Toxicity - Studies in relevant species with extended observation periods
- Genotoxicity - Standard battery with consideration of nano-specific interactions
- Reproductive Toxicity - Based on product distribution and clinical indication
- Carcinogenicity - Typically required for chronic-use products with tissue persistence
Clinical Development Considerations:
- First-in-human dosing strategies based on minimum anticipated biological effect level (MABEL) approach
- Special safety monitoring for infusion-related reactions
- Pharmacodynamic biomarkers to demonstrate proof-of-concept
- Comparative bioavailability studies for products with reference formulations
The regulatory pathways for nanotechnology-enabled drug products require meticulous attention to quality-by-design principles, comprehensive physicochemical characterization, and tailored safety assessment strategies. Both FDA and EMA have established frameworks that emphasize the unique properties of nanomedicines while maintaining flexibility for innovative approaches. Successful navigation of these pathways demands early regulatory engagement, robust scientific justification for development decisions, and thorough documentation of product attributes throughout the development lifecycle. As the field evolves, regulatory science continues to advance with new guidelines and standards emerging to address the challenges posed by these complex therapeutic products.
The nanotechnology drug delivery market is experiencing robust growth, driven by the need for more precise and effective therapeutic solutions for chronic diseases. This market encompasses the application of nanoscale materials, typically within the 1 to 100 nanometer range, to develop advanced systems for delivering therapeutic agents [1] [55]. These systems are engineered to improve drug solubility, stability, and bioavailability, while enabling targeted delivery and controlled release, thereby enhancing treatment efficacy and reducing side effects [120] [55].
The global market is on a strong upward trajectory, as detailed in Table 1: Nanotechnology Drug Delivery Market Size and Growth Projections. The market is characterized by significant investments in research and development, successful clinical validation of platforms like lipid nanoparticles (LNPs) in mRNA vaccines, and a growing pipeline of nano-enabled biologics and gene therapies [121] [7].
Table 1: Nanotechnology Drug Delivery Market Size and Growth Projections
| Source | Base Year Market Size (USD Billion) | Projected Year Market Size (USD Billion) | Forecast Period | CAGR (%) |
|---|---|---|---|---|
| SNS Insider [122] | 96.39 (2024) | 200.77 (2032) | 2025-2032 | 9.56 |
| Transparency Market Research [123] | 97.8 (2024) | 315.9 (2035) | 2025-2035 | 11.3 |
| Allied Market Research [120] | 87.5 (2022) | 209.5 (2032) | 2023-2032 | 9.1 |
| Precedence Research [124] | 97.98 (2024) | 209.73 (2034) | 2025-2034 | 7.91 |
| Research Nester [125] | 107.65 (2025) | 261.95 (2035) | 2026-2035 | 9.3 |
Analysis of Dominant Market Segments
Segmentation by Technology
Nanotechnology drug delivery platforms are diverse, each offering distinct advantages for different therapeutic applications. The market is led by nanoparticles and lipid-based systems, which have been instrumental in the success of recent therapies, including mRNA vaccines [121] [7].
Table 2: Dominant Segments by Technology and Application (2024 Market Share)
| Segmentation | Dominant Segment | 2024 Market Share | Key Growth Drivers |
|---|---|---|---|
| By Technology | Nanoparticles | ~49.1% [122] / 35.6% [123] | Versatility, ease of functionalization, improved PK/PD profiles [122]. |
| Lipid Nanoparticles (LNPs) | 32.33% of revenue [121] | Clinical validation via mRNA vaccines; scalable manufacturing [121] [7]. | |
| By Application | Oncology & Hematology | ~33.5% [122] / 43.54% [121] | High global cancer burden; need for targeted, less-toxic therapies [122] [125]. |
| Neurology | Fastest Growing [122] | Rising burden of neurodegenerative diseases; research on crossing the blood-brain barrier [122] [120]. |
The nanoparticles segment holds the largest market share, valued for its versatility, ease of surface functionalization, and ability to improve pharmacokinetics and targeted delivery [122]. Meanwhile, lipid nanoparticles (LNPs) have become a commercial anchor, generating significant revenue due to their proven success in delivering mRNA and siRNA, which has normalized their use across broader therapeutic categories [121].
Segmentation by Application and End-User
On the application front, oncology and hematology constitute the largest segment. The high global cancer burden, with projections of 35 million new cases by 2050, fuels the demand for targeted therapies that minimize the toxic side effects of conventional chemotherapy [125]. Nanoparticles can be engineered to leverage the Enhanced Permeability and Retention (EPR) effect in tumors for passive targeting or be functionalized with ligands for active targeting of cancer cells [7] [55].
The neurology segment is anticipated to be the fastest-growing application area [122]. This growth is driven by the increasing prevalence of neurodegenerative diseases like Alzheimer's and Parkinson's, coupled with groundbreaking research into nanocarriers capable of crossing the formidable blood-brain barrier for targeted drug delivery to the brain [122] [120].
Regarding end-users, biopharmaceutical companies dominated the market in 2024, holding a 42.25% share, as they are central to the development and commercialization of nano-therapeutics [122]. However, the research institutes & laboratories segment is expected to grow the fastest, indicating a vibrant pipeline of innovation originating from academic and translational research environments [122].
Regional Market Analysis
The global landscape for nanotechnology drug delivery is dominated by North America, but the Asia-Pacific region is emerging as the growth epicenter for the future.
Table 3: Regional Market Analysis and Growth Outlook
| Region | Market Share (2024) | Growth Outlook (CAGR) | Key Growth Drivers |
|---|---|---|---|
| North America | 41.03% [122] - 43.5% [125] | ~9.24% (U.S.) [122] | Sophisticated healthcare infrastructure, strong federal funding (e.g., National Nanotechnology Initiative), high pharma R&D concentration [122] [124]. |
| Europe | Significant Market | -- | Horizon Europe grants, national co-funding, strong chemical clusters (Germany), clinical trial infrastructure (Benelux) [121]. |
| Asia Pacific (APAC) | -- | 9.81% [122] - 13.03% [121] (Fastest) | Increasing healthcare expenditure, developing pharma manufacturing, vast patient pool, government initiatives, growing outsourcing hub [122] [123]. |
| Latin America, Middle East & Africa | Modest Revenue | Growing Demand | Localization efforts for vaccine and nano-therapeutic production (e.g., Brazil, Saudi Arabia) [121]. |
North America's dominance is anchored by the United States, which boasts a sophisticated healthcare infrastructure, significant government investment through programs like the National Nanotechnology Initiative (NNI), and a high concentration of pharmaceutical and biotechnology key players driving R&D and commercialization [122] [124].
The Asia Pacific region is poised to register the highest CAGR during the forecast period [122] [121]. This growth is fueled by increasing healthcare expenditure, rapidly developing pharmaceutical manufacturing infrastructure, a vast patient base, and supportive government initiatives in countries like China and India, which are also becoming enormous research outsourcing hubs [123] [121].
Experimental Protocols for Nanoparticle Characterization
Robust characterization is paramount in nanomedicine development. The following protocols outline key experiments for evaluating nanoparticle physicochemical properties and safety.
Protocol: Physicochemical Characterization of Nanoparticles
Objective: To determine the critical quality attributes (CQAs) of synthesized nanoparticles, including size, surface charge (zeta potential), and morphology.
Materials:
- Nanoparticle suspension: Purified and appropriately diluted.
- Electrophoretic light scatterer: For zeta potential measurement.
- Dynamic Light Scattering (DLS) instrument: For size and distribution analysis.
- Transmission Electron Microscopy (TEM) or Scanning Electron Microscopy (SEM): For morphological analysis.
Methodology:
- Sample Preparation: Dilute the nanoparticle suspension in an appropriate buffer (e.g., 1mM KCl for zeta potential) to achieve a concentration suitable for the instrument, ensuring the scattering intensity is within the linear range [126].
- Dynamic Light Scattering (DLS):
- Transfer the diluted sample into a disposable sizing cuvette.
- Place the cuvette in the DLS instrument and set the temperature to 25°C.
- Perform a minimum of 10 measurement runs.
- Record the hydrodynamic diameter (Z-average), and the polydispersity index (PDI) as a measure of size distribution. A PDI <0.2 is generally considered monodisperse [126].
- Zeta Potential Measurement:
- Load the diluted sample into a folded capillary zeta cell.
- Insert the cell into the instrument and apply a voltage (e.g., 150 V).
- Measure the electrophoretic mobility, which is converted to zeta potential by the instrument's software using the Henry equation.
- Report the average and standard deviation from at least 3 measurements. A zeta potential >|±30| mV typically indicates good colloidal stability [126].
- Electron Microscopy (TEM/SEM):
- For TEM, deposit a drop of diluted nanoparticle suspension onto a carbon-coated copper grid and blot away excess liquid.
- Negative staining with 1-2% uranyl acetate may be applied for contrast.
- Allow the grid to air-dry completely before loading into the microscope.
- Image the nanoparticles at appropriate magnifications to assess morphology, size, and confirm DLS data.
Data Analysis: Correlate DLS size data with TEM images. The PDI from DLS indicates batch homogeneity, while zeta potential is a key predictor of physical stability and interaction with biological membranes [126].
Protocol: In Vitro Cytotoxicity Assessment (MTT Assay)
Objective: To evaluate the potential cytotoxicity of nanoparticle formulations on mammalian cell lines.
Materials:
- Cell line: Relevant to the application (e.g., Caco-2 for intestinal, HepG2 for liver).
- Culture media: Appropriate for the cell line, with serum.
- Nanoparticle formulations: Sterile, at various concentrations.
- MTT reagent: (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide).
- Solubilization solution: (e.g., DMSO or SDS with HCl).
- 96-well tissue culture plate.
- CO₂ incubator.
- Microplate reader.
Methodology:
- Cell Seeding: Harvest and seed cells in a 96-well plate at a density of 1x10⁴ cells/well in 100 µL of complete medium. Incubate for 24 hours at 37°C and 5% CO₂ to allow cell attachment.
- Treatment: Prepare a serial dilution of the nanoparticle stock in culture medium. Remove the medium from the 96-well plate and add 100 µL of each nanoparticle concentration to the wells. Include wells with culture medium only (blank) and cells with medium only (untreated control). Incubate for 24-72 hours.
- MTT Assay:
- After treatment, carefully remove the medium.
- Add 100 µL of fresh medium containing 0.5 mg/mL MTT to each well. Incubate for 2-4 hours at 37°C.
- Carefully remove the MTT-containing medium without disturbing the formed formazan crystals.
- Add 100 µL of solubilization solution (e.g., DMSO) to each well to dissolve the formazan crystals. Shake the plate gently for 10 minutes.
- Absorbance Measurement: Use a microplate reader to measure the absorbance of each well at a wavelength of 570 nm, with a reference wavelength of 630-690 nm.
Data Analysis:
- Calculate the cell viability percentage:
(Absorbance of treated sample - Absorbance of blank) / (Absorbance of untreated control - Absorbance of blank) * 100. - Generate a dose-response curve and calculate the half-maximal inhibitory concentration (IC₅₀). This assay measures mitochondrial activity as a marker of cell viability and is a standard first step in assessing nanoparticle biocompatibility [126].
Visualizing the Nanomedicine Workflow and Challenges
The journey from nanoparticle design to a clinically viable drug product involves multiple critical stages and challenges. The following diagram illustrates this complex workflow and the key "translational gaps" that must be bridged.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful development of nanotechnology-based drug delivery systems relies on a suite of critical materials and technologies.
Table 4: Essential Research Reagent Solutions for Nanotechnology Drug Delivery
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| Lipids (Ionizable, Phospholipids, Cholesterol) | Core components of LNPs and liposomes; encapsulate and protect payload (mRNA, siRNA, small molecules); enable endosomal escape [126] [7]. | Key to COVID-19 mRNA vaccines. Ionizable lipids (e.g., DLin-MC3-DMA) are critical for efficiency [7]. |
| Biodegradable Polymers (PLGA, PLA, Chitosan) | Form polymeric nanoparticles and micelles; provide controlled drug release profiles; improve stability [7] [55]. | PLGA is widely used with established safety. Chitosan offers mucoadhesive properties [7]. |
| PEGylated Lipids/Polymers | Impart "stealth" properties by reducing opsonization and clearance by the immune system; prolong circulation half-life [7]. | Concern over anti-PEG antibodies driving research into non-PEG alternatives (e.g., zwitterionic polymers) [7]. |
| Microfluidic Mixers | Enable precise, reproducible, and scalable synthesis of nanoparticles (LNPs, liposomes); control particle size and PDI [121]. | Essential for translating lab-scale synthesis to GMP production. Systems from Precision Nanosystems, NanoCalibur [123] [121]. |
| Targeting Ligands (Peptides, Antibodies, Aptamers) | Conjugated to nanoparticle surface for active targeting to specific cells/tissues (e.g., cancer cells); enhance therapeutic index [7] [55]. | |
| Process Analytical Technologies (PAT) | In-line monitoring of Critical Process Parameters (CPPs) during manufacturing; ensures consistent product quality and batch-to-batch reproducibility [1]. | A core component of Quality by Design (QbD) for nanomedicine [1]. |
Comparative Analysis of Platform Efficacy, Safety, and Commercial Viability
Targeted drug delivery represents a paradigm shift in therapeutic interventions, aiming to maximize drug efficacy at disease sites while minimizing systemic side effects. Within this field, nanotechnology has emerged as a transformative force, enabling the design of sophisticated carriers that navigate biological complexities with unprecedented precision. This document provides a comparative analysis of major nanotechnology platforms—lipid-based, polymeric, and inorganic nanoparticles—evaluating their efficacy, safety, and commercial potential. Framed within a broader research thesis on advanced drug delivery systems, these application notes and protocols are designed to equip researchers and drug development professionals with the data and methodologies necessary to critically assess and implement these technologies. The analysis integrates current market trajectories, with the global nanotechnology drug delivery market projected to grow from $107.65 billion in 2025 to $261.95 billion by 2035, reflecting a compound annual growth rate (CAGR) of 9.3% [125] [123]. This growth is propelled by the rising prevalence of chronic diseases, advancements in nanomedicine research, and the proven success of platforms like lipid nanoparticles in mRNA vaccine delivery [121] [123].
The following tables provide a consolidated overview of key quantitative data for the major nanotechnology drug delivery platforms, covering market positioning, therapeutic performance, and physicochemical characteristics.
Table 1: Market Position and Commercial Viability of Nanotechnology Platforms
| Platform | Market Share (2024) | Projected CAGR (%) | Dominant Application(s) | Key Commercial Advantage | Primary Manufacturing Challenge |
|---|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | 32.33% [121] | 13.23% to 2030 [121] | mRNA Vaccines, Gene Therapy [121] | Clinical validation from COVID-19 vaccines; turnkey GMP solutions available [121] | Scale-up of microfluidic-based production [121] |
| Polymeric Nanoparticles | Information Missing | Information Missing | Oncology, Chronic Therapies [121] | Tunable release profiles; suitability for multi-payload constructs [121] | High CMC & GMP compliance costs [121] |
| Liposomes | Information Missing | Information Missing | Oncology (e.g., chemotherapeutics) [121] | Established, well-understood technology; long history of clinical use [127] | Stability and sterilization during manufacturing [127] |
| Nanocrystals | Information Missing | Information Missing | Poorly Soluble Drugs [121] | Drastically improved solubility and bioavailability for BCS Class II drugs [127] | Milling and homogenization processes can be energy-intensive [127] |
| Dendrimers | Information Missing | Information Missing | Targeted Drug Delivery, Multivalent Ligand Display [121] | Precise, monodisperse structure with high surface functionality [127] | Complex, costly synthesis and potential toxicity concerns [121] [127] |
Table 2: Efficacy and Safety Profile of Leading Nanoplatforms
| Platform | Targeting Efficiency (Representative) | Key Safety Considerations | Scalability (1-5, 5=Best) | Regulatory Approval Landscape |
|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | High (Validated for mRNA delivery) [121] | Reactogenicity (e.g., temporary flu-like symptoms); long-term biodistribution data evolving [121] [33] | 4 (Rapid advances in scalable manufacturing) [121] | Clear pathway post-COVID-19 vaccines; established FDA/EMA guidance [121] |
| Liposomes | Moderate to High (e.g., 94% targeting accuracy in preclinical models) [121] | Infusion reactions; "complement activation-related pseudoallergy" (CARPA) [127] | 5 (Well-established, large-scale production) [127] | Mature, with many approved products (e.g., Doxil, Myocet) [127] |
| Polymeric NPs (PLGA) | High (e.g., 94% precision in tumor chemotherapy in study) [121] | Inflammatory response to degradation products; uncertain long-term toxicology [121] [33] | 3 (Scale-up bottlenecks exist) [121] | Several approved products (e.g., Abraxane); requires extensive characterization [128] |
| Gold Nanoparticles | High (for photothermal therapy) [128] | Long-term accumulation concerns; potential cytotoxicity [33] [128] | 2 (Cost and complex functionalization) [128] | Primarily in imaging and diagnostics; therapeutic approvals pending [128] |
Experimental Protocols for Key Nanoplatforms
Protocol 1: Formulation of Lipid Nanoparticles (LNPs) via Microfluidic Mixing
This protocol details the synthesis of LNPs for nucleic acid encapsulation, a technology pivotal to modern gene therapies and vaccines [121] [129].
1. Principle: LNPs are formed by rapid mixing of an aqueous phase containing nucleic acids (e.g., mRNA) with an organic phase containing ionizable lipids, phospholipids, cholesterol, and PEG-lipids. The rapid change in polarity causes lipid self-assembly into particles that encapsulate the nucleic acid payload [121].
2. Research Reagent Solutions:
- Ionizable Lipid (e.g., DLin-MC3-DMA): Serves as the primary cationic component for complexing anionic nucleic acids and enabling endosomal escape.
- Phospholipid (e.g., DSPC): Stabilizes the LNP bilayer structure and enhances fusion with cell membranes.
- Cholesterol: Modulates membrane fluidity and stability, improving structural integrity and circulation time.
- PEG-lipid (e.g., DMG-PEG2000): Shields the LNP surface, reducing nonspecific interactions with proteins and cells, thereby prolonging circulation half-life.
- mRNA (or other nucleic acid): The therapeutic payload, typically in a citrate buffer (pH 4.0).
- Ethanol (Absolute): Solvent for the lipid mixture.
- TRIS Buffered Saline (TBS, pH 7.4): For dialysis and final formulation.
3. Procedure: 1. Lipid Phase Preparation: Dissolve the ionizable lipid, phospholipid, cholesterol, and PEG-lipid at a defined molar ratio (e.g., 50:10:38.5:1.5 mol%) in absolute ethanol to a final concentration of 10-20 mg/mL total lipids. Filter through a 0.22 µm PTFE membrane. 2. Aqueous Phase Preparation: Dilute the mRNA in a citrate buffer (pH 4.0) to a concentration that achieves the desired Nitrogen-to-Phosphate (N:P) ratio. 3. Microfluidic Mixing: Use a commercial microfluidic mixer (e.g., NanoCalibur system [123]). Set the flow rate ratio (aqueous:organic) to 3:1. Simultaneously pump the aqueous and organic phases into the mixer's inlet channels. 4. Collection: Collect the resulting LNP suspension in a sterile container. 5. Buffer Exchange & Purification: Transfer the crude LNP suspension into a dialysis cassette (MWCO 100 kDa) and dialyze against a large volume of TBS (pH 7.4) for at least 18 hours at 4°C to remove ethanol and exchange the buffer. Alternatively, use tangential flow filtration (TFF). 6. Sterile Filtration: Filter the final LNP formulation through a 0.22 µm sterile filter into an apyrogenic vial.
4. Characterization: * Particle Size and PDI: Determine by Dynamic Light Scattering (DLS). Target size: 70-100 nm; PDI < 0.2. * Zeta Potential: Measure by Laser Doppler Micro-electrophoresis. Expected value: Slightly negative or neutral in physiological buffer. * Encapsulation Efficiency: Quantify using a Ribogreen assay. Compare fluorescence before and after disruption of LNPs with Triton X-100. Target: >90%. * Morphology: Visualize using Cryo-Electron Microscopy (Cryo-EM) to confirm a spherical, core-shell structure.
Diagram 1: LNP Formulation Workflow
Protocol 2: Preparation of Polymeric Nanoparticles (PLGA) by Nanoprecipitation
This protocol describes the synthesis of biodegradable Poly(lactic-co-glycolic acid) (PLGA) nanoparticles for sustained drug release, widely used in oncology and chronic disease management [121] [127].
1. Principle: The method is based on the interfacial deposition of a polymer following the displacement of a semi-polar solvent from a lipophilic solution to an aqueous phase. This rapid diffusion causes the polymer to precipitate into nanoparticles, encapsulating hydrophobic drugs [127].
2. Research Reagent Solutions:
- PLGA (50:50, ester-terminated): The biodegradable polymer matrix that forms the nanoparticle core and controls drug release kinetics.
- Drug Molecule (Hydrophobic): The therapeutic agent to be encapsulated (e.g., Paclitaxel, Doxorubicin).
- Acetone (or Acetonitrile): A water-miscible organic solvent for dissolving the polymer and drug.
- Polyvinyl Alcohol (PVA): A surfactant/stabilizer dissolved in the aqueous phase to prevent nanoparticle aggregation.
- Ultrapure Water (Milli-Q): The aqueous antisolvent phase.
3. Procedure: 1. Organic Phase: Dissolve 50 mg of PLGA and 5 mg of the hydrophobic drug in 10 mL of acetone under magnetic stirring. 2. Aqueous Phase: Dissolve 100 mg of PVA in 100 mL of ultrapure water to create a 1% (w/v) solution. Filter through a 0.45 µm membrane. 3. Nanoprecipitation: Under moderate magnetic stirring (500-700 rpm), rapidly inject the organic phase into the aqueous phase using a syringe pump (e.g., 1 mL/min) or manual syringe. 4. Solvent Evaporation: Stir the resulting nano-suspension uncovered for 4-6 hours at room temperature to allow for complete evaporation of the organic solvent. 5. Purification: Centrifuge the suspension at 20,000 x g for 30 minutes at 4°C. Carefully decant the supernatant and re-suspend the nanoparticle pellet in ultrapure water. Repeat this wash step twice. 6. Lyophilization: Re-suspend the final pellet in a cryoprotectant solution (e.g., 5% trehalose) and lyophilize for 48 hours to obtain a dry, free-flowing powder for storage.
4. Characterization: * Particle Size and PDI: Analyze by DLS. * Drug Loading & Encapsulation Efficiency: Determine by HPLC-UV/Vis. Dissolve a known amount of nanoparticles in DMSO to release the drug and compare to a standard curve. * In Vitro Drug Release: Use dialysis against PBS (pH 7.4) at 37°C. Collect samples at predetermined time points and quantify drug content via HPLC.
Safety and Efficacy Assessment Pathways
A critical component of nanomedicine development is the systematic evaluation of biological interactions. The following diagram and protocol outline a standard workflow for assessing nanoparticle safety and efficacy in vitro.
Diagram 2: Nanoparticle Safety & Efficacy Screening
Protocol 3: In Vitro Cytotoxicity and Cellular Uptake Assessment
1. Principle: This protocol uses a colorimetric MTT assay to measure cell viability as a marker of cytotoxicity and flow cytometry to quantify cellular uptake of fluorescently labeled nanoparticles [33] [128].
2. Research Reagent Solutions:
- Cell Line: Relevant to target tissue (e.g., HeLa for cancer, Caco-2 for oral delivery).
- Nanoparticles: Test formulations, with one batch fluorescently labeled (e.g., with Cy5).
- MTT Reagent: (3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide) dissolved in PBS.
- Lysis Buffer: Acidified isopropanol or DMSO.
- Flow Cytometry Buffer: PBS with 2% FBS.
3. Procedure for MTT Assay: 1. Cell Seeding: Seed cells in a 96-well plate at a density of 1x10⁴ cells/well and incubate for 24 hours. 2. Treatment: Treat cells with a concentration series of nanoparticles (e.g., 0.1-100 µg/mL) for 24-48 hours. Include untreated cells as a negative control and cells treated with a cytotoxic agent (e.g., 1% Triton X-100) as a positive control. 3. MTT Incubation: Replace media with 100 µL of fresh media containing 0.5 mg/mL MTT. Incubate for 4 hours at 37°C. 4. Solubilization: Carefully remove the MTT solution and add 100 µL of DMSO to each well to dissolve the formed formazan crystals. 5. Absorbance Measurement: Measure the absorbance at 570 nm using a microplate reader. Calculate cell viability as a percentage of the untreated control.
4. Procedure for Cellular Uptake (Flow Cytometry): 1. Treatment: Seed cells in a 12-well plate. At ~80% confluency, treat with Cy5-labeled nanoparticles at a predetermined concentration for 1-4 hours. 2. Harvesting: Wash cells twice with cold PBS. Trypsinize and resuspend in flow cytometry buffer. 3. Analysis: Analyze cells immediately using a flow cytometer. Use untreated cells to set the autofluorescence baseline. The geometric mean fluorescence intensity (MFI) of the treated population is proportional to nanoparticle uptake.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Nanotechnology Drug Delivery Research
| Reagent / Material | Function in Research | Example Use-Case |
|---|---|---|
| Ionizable Cationic Lipids | Complexes nucleic acids; enables endosomal escape in LNPs [121] | Formulating mRNA vaccines or gene therapies. |
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer matrix for controlled drug release [127] | Creating sustained-release nanoparticles for chemotherapeutics. |
| DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine) | Phospholipid that stabilizes the lipid bilayer in liposomes and LNPs [121] | Improving structural integrity and fusion with cell membranes. |
| DMG-PEG2000 | PEG-lipid used for surface shielding to increase circulation half-life [121] | Reducing protein opsonization and rapid clearance by the immune system. |
| PVA (Polyvinyl Alcohol) | Surfactant and stabilizer in polymeric nanoparticle formation [127] | Preventing aggregation during the nanoprecipitation process. |
| MTT/XTT Reagents | Indicators of metabolic activity for in vitro cytotoxicity testing [33] | Assessing nanoparticle safety profile on cell lines. |
| Cy5 NHS Ester | Fluorescent dye for labeling nanoparticles for tracking studies [128] | Visualizing cellular uptake and biodistribution in vitro and in vivo. |
Conclusion
Nanotechnology has unequivocally transformed the paradigm of targeted drug delivery, offering sophisticated solutions to enhance therapeutic efficacy and reduce systemic toxicity. The journey from foundational nanoparticle design to clinical application, however, is fraught with challenges, most notably the significant translational gap and complex manufacturing and regulatory hurdles. Future success hinges on developing more predictive preclinical models, advancing non-PEG stealth coatings, and embracing integrated formulation strategies. The convergence of nanomedicine with artificial intelligence for drug design and the push towards personalized nanotherapies represent the next frontier. For researchers and developers, a focused approach on biocompatibility, scalable manufacturing, and rigorous clinical validation is paramount to fully realize nanotechnology's potential in saving and improving lives.
References
- 1. the transformative potential of nanotechnology in medicine [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1556426/full]
- 2. Precise nanoscale fabrication technologies, the “last mile” of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145073/]
- 3. Nano–bio interactions and drug delivery using soft nanoparticles [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d4pm00170b]
- 4. Characterisation of polymeric nanoparticles for drug delivery [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr00071h]
- 5. Achieving Targeted Delivery with Nanoscale Systems [https://www.pharmtech.com/view/achieving-targeted-delivery-with-nanoscale-systems]
- 6. Advances in nanoparticles in targeted drug delivery–A review [https://www.sciencedirect.com/science/article/pii/S2666845925001163]
- 7. Bridging the Gap: The Role of Advanced Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579833/]
- 8. Strategies for nanoscale drug delivery systems to evade ... [https://pubmed.ncbi.nlm.nih.gov/40845988/]
- 9. Advances in Liposomal Drug Delivery - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298344/]
- 10. Versatility of LNPs across different administration routes for targeted ... [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb00575b]
- 11. Characterisation of polymeric nanoparticles for drug delivery [https://pubs.rsc.org/en/content/articlelanding/2025/nr/d5nr00071h]
- 12. Liposomes: recent progress on nanoparticles production ... [https://www.sciencedirect.com/science/article/pii/S2772950825004121]
- 13. Galloylated liposomes enable targeted drug delivery by ... [https://www.nature.com/articles/s41467-025-63198-4]
- 14. Lipid Nanoparticle Drug Delivery Advances April 1-7, 2025 [https://www.linkedin.com/pulse/lipid-nanoparticle-drug-delivery-advances-april-1-7-2025-g4mzc]
- 15. Lipid Nanoparticle (LNP) Drug Delivery Advances, April 7-14, 2025 [https://www.precigenome.com/post/lipid-nanoparticle-lnp-drug-delivery-advances-april-7-14-2025]
- 16. Advanced rational design of polymeric nanoparticles for ... [https://pubmed.ncbi.nlm.nih.gov/40484283/]
- 17. Polymeric Nanoparticles in Targeted Drug Delivery [https://www.mdpi.com/2073-4360/17/7/833]
- 18. Overview of dendrimers as promising drug delivery ... [https://www.sciencedirect.com/science/article/pii/S2590156725000751]
- 19. Dendrimer-based drug delivery systems: history, challenges ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-022-00298-5]
- 20. The Promise of PAMAM Dendrimers in Biomedical Applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299782/]
- 21. Dendrimers for drug delivery: An overview of its classes, ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224724005653]
- 22. Targeted Nanoparticles for Drug Delivery Across the Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627166/]
- 23. Targeted drug delivery in neurodegenerative diseases [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1522223/full]
- 24. current challenges and perspectives in drug delivery systems [https://pubmed.ncbi.nlm.nih.gov/35005431/]
- 25. Review on metal nanoparticles as nanocarriers [https://link.springer.com/article/10.1007/s42247-021-00335-x]
- 26. Drug nanocrystals: Surface engineering and its ... [https://www.sciencedirect.com/science/article/pii/S2589004224024106]
- 27. The Enhanced Permeability and Retention (EPR) Effect [https://pmc.ncbi.nlm.nih.gov/articles/PMC8402171/]
- 28. Enhanced permeability and retention effect [https://en.wikipedia.org/wiki/Enhanced_permeability_and_retention_effect]
- 29. Nano-drug delivery: Is the enhanced permeability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7397928/]
- 30. Enhancement of EPR Effect for Passive Tumor Targeting [https://www.mdpi.com/2076-3417/15/6/3189]
- 31. A Quantitative MRI-Based Approach to Estimate the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11412736/]
- 32. Beyond the EPR effect: Intravital microscopy analysis of ... [https://www.sciencedirect.com/science/article/pii/S0169409X25000353]
- 33. the transformative potential of nanotechnology in medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360437/]
- 34. Image-guided strategies to improve drug delivery to tumors ... [https://www.sciencedirect.com/science/article/pii/S0006291X25010617]
- 35. Drug Nanocarriers for Pharmaceutical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388938/]
- 36. Review Nanoparticle-enhanced drug delivery systems [https://www.sciencedirect.com/science/article/abs/pii/S0167732225001576]
- 37. Recent insights and applications of nanocarriers-based ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842825000344]
- 38. Optimal size and PEG coating of gold nanoparticles for ... [https://pubs.rsc.org/en/content/articlehtml/2025/na/d4na00782d]
- 39. Long-acting lipid-based nanomedicines: rethinking from ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592501079X]
- 40. Optimizing Cancer Treatment: A Comprehensive Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584355/]
- 41. Advances in passive and active targeting strategies [https://www.sciencedirect.com/science/article/abs/pii/S0378517325005733]
- 42. Exploring the therapeutic potential of ligand-decorated ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325005241]
- 43. Antibody-functionalized lipid nanocarriers for RNA-based ... [https://pubs.rsc.org/en/content/articlehtml/2025/na/d5na00323g]
- 44. Nanoparticle targeting: Review of passive and active ... [https://insidetx.com/resources/reviews/a-comprehensive-review-of-passive-and-active-nanoparticle-targeting-technics/]
- 45. Comprehensive analysis of the tumor targeting efficiency ... [https://www.nature.com/articles/s41598-025-22151-7]
- 46. pH-responsive Nanoparticles for Drug Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3379544/]
- 47. A comprehensive study on pH-sensitive nanoparticles ... [https://www.bsmiab.org/jabet/articles/178-1730094477]
- 48. Redox-responsive and pH-sensitive nanoparticles ... [https://www.dovepress.com/redox-responsive-and-ph-sensitive-nanoparticles-enhanced-stability-and-peer-reviewed-fulltext-article-DDDT]
- 49. Targeted and redox-responsive drug delivery systems ... [https://www.nature.com/articles/s41598-020-71071-1]
- 50. Strategies for delivering drugs across the blood-brain ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 51. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 52. Nanoparticles across mucosal barriers [https://www.sciencedirect.com/science/article/abs/pii/S0168365925008806]
- 53. Brain-targeted intranasal delivery of biologics - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00148j]
- 54. Nanomaterial-Based Blood-Brain-Barrier (BBB) Crossing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6915305/]
- 55. Nano based drug delivery systems: recent developments and ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-018-0392-8]
- 56. Navigating Neurotoxicity and Safety Assessment of ... [https://www.sciencedirect.com/science/article/pii/S1742706124005439]
- 57. Advances in targeted drug delivery systems for cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725008056]
- 58. Review article Mechanistic study of cancer drug delivery [https://www.sciencedirect.com/science/article/pii/S0223523425003009]
- 59. Nanoparticle-based targeted delivery unleashes the full ... [https://www.uchicagomedicine.org/forefront/cancer-articles/2025/may/nanoparticle-based-targeted-delivery-unleashes-the-full-power-of-anti-cancer-drugs]
- 60. Nanotechnology in oncology: advances in biosynthesis, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182552/]
- 61. Nanocarriers for Combination Therapy in Pancreatic Ductal ... [https://pubmed.ncbi.nlm.nih.gov/40801679/]
- 62. Advances in Lipid-Based Nanomedicine: Pathway Specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413497/]
- 63. Nano-Drug Delivery Systems for Bone Metastases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12115183/]
- 64. Design of nano-delivery systems for pancreatic cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525006706]
- 65. Advances in RNA-based cancer therapeutics: pre-clinical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512572/]
- 66. Bone targeted nano-drug and nano-delivery | Bone Research [https://www.nature.com/articles/s41413-024-00356-2]
- 67. Advancements in nano-based drug delivery systems for ... [https://pubs.rsc.org/en/content/articlelanding/2025/pm/d5pm00179j]
- 68. Nanomedicine: How nanomaterials are transforming drug ... [https://www.sciencedirect.com/science/article/pii/S2949829524000901]
- 69. Nanomaterials in Drug Delivery: Leveraging Artificial ... [https://www.mdpi.com/1422-0067/26/22/11121]
- 70. Comparison of Drug Delivery Systems with Different Types of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11679882/]
- 71. Advances in Nanotechnology-Based Drug Delivery Systems [https://www.mdpi.com/1999-4923/17/8/1038]
- 72. Nano-regenerative medicine towards clinical outcome of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3822969/]
- 73. Top 10 nanotechnology innovations for 2025 [https://www.inpart.io/blog/top-10-new-nanotechnology-innovations]
- 74. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 75. Lost in translation: the valley of death across preclinical and ... [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]
- 76. Factors determining drug delivery system translation [https://www.sciencedirect.com/science/article/abs/pii/S0168365925007795]
- 77. A Framework for Improving Clinical Translatability with AI ... [https://blog.td2inc.com/redesigning-preclinical-oncology?hsLang=en]
- 78. Navigating translational research in nanomedicine [https://www.sciencedirect.com/science/article/pii/S0378517325000389]
- 79. Upscaling and GMP production of pharmaceutical drug delivery systems - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/B9780128178706000110]
- 80. Current hurdles to the translation of nanomedicines from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8300981/]
- 81. Scaling nanopharmaceutical production for personalized medicine: challenges and strategies | Journal of Nanoparticle Research [https://link.springer.com/article/10.1007/s11051-025-06293-3]
- 82. Advances in Nanotechnology-Based Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389492/]
- 83. Nanotoxicity: An Interplay of Oxidative Stress, Inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5304638/]
- 84. Nanotoxicity unveiled: Evaluating exposure risks and ... [https://www.sciencedirect.com/science/article/pii/S2773050625000436]
- 85. General Nanotoxicity Mechanism [https://www.cd-bioparticles.com/t/General-Nanotoxicity-Mechanism_63.html]
- 86. Comprehensive insights into mechanism of nanotoxicity ... [https://link.springer.com/article/10.1186/s11671-024-04118-1]
- 87. 25 years of research and regulation: Is nanotechnology ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1629813/full]
- 88. Considering the immunogenicity of PEG - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413056/]
- 89. Developments in nanotechnology approaches for the ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00656-1]
- 90. PEG alternatives for RNA therapeutics [https://www.nature.com/articles/s41563-025-02408-2]
- 91. Anti-PEG Antibodies and Their Biological Impact on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388889/]
- 92. Impact of pre-existing anti-polyethylene glycol (PEG) IgM ... [https://pubmed.ncbi.nlm.nih.gov/40339658/]
- 93. Polyethylene glycol immunogenicity in nanomedicine [https://scholar.nycu.edu.tw/en/publications/polyethylene-glycol-immunogenicity-in-nanomedicine/]
- 94. Rethinking Pharmaceutical Industry with Quality by Design [https://www.pharmaexcipients.com/news/rethinking-pharmaceutical-industry-qbd/]
- 95. A Review on QbD-Driven Optimization of Lipid ... [https://pubmed.ncbi.nlm.nih.gov/40626137/]
- 96. Design of experiments in the optimization of nanoparticle- ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365923003073]
- 97. Quality of medicines questions and answers: Part 2 [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/quality-medicines-qa-introduction/quality-medicines-questions-answers-part-2]
- 98. Engineering precision nanoparticles for drug delivery [https://www.nature.com/articles/s41573-020-0090-8]
- 99. REVIEW Current research trends of nanomedicines [https://www.sciencedirect.com/science/article/pii/S2211383523001636]
- 100. Clinical cancer nanomedicines [https://www.sciencedirect.com/science/article/pii/S0168365925006121]
- 101. Cancer nanomedicine: a review of recent success in drug ... [https://clintransmed.springeropen.com/articles/10.1186/s40169-017-0175-0]
- 102. Nanoparticles in Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC9821409/]
- 103. Nanomedicine in Cancer Therapeutics: Current Perspectives ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02368-w]
- 104. Nanotechnology in Drug Delivery [https://blog.drugbank.com/nanotechnology-in-drug-delivery/]
- 105. Protocols - Nanotechnology Characterization Lab - NCI [https://dctd.cancer.gov/drug-discovery-development/assays/nano/protocols-and-capabilities]
- 106. Nanotechnology: What it can do for drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1949907/]
- 107. Nanomedicine applications in the treatment of breast cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC5566389/]
- 108. Nanotechnology in Targeted Drug Delivery [https://www.arensia-em.com/blog-48-nanotechnology-in-targeted-drug-delivery-breaking-barriers-in-cancer-treatment]
- 109. Progress and challenges towards targeted delivery of ... [https://www.nature.com/articles/s41467-018-03705-y]
- 110. Beyond Formulation: Contributions of Nanotechnology for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9415580/]
- 111. Safety and Efficacy of BIND-014, a Docetaxel Nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6233779/]
- 112. BIND Therapeutics Presents Complete Data on… [https://www.flagshippioneering.com/news/press-release/bind-therapeutics-presents-complete-data-clinical-activity-bind-014-patients-metastatic-c]
- 113. Regulatory pathways and guidelines for nanotechnology ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1544393/full]
- 114. Nanotechnology Drug Delivery Market: A Deep-Dive ... [https://www.pharmiweb.com/press-release/2025-07-17/nanotechnology-drug-delivery-market-a-deep-dive-analysis-2025-2035]
- 115. Nanotechnology Programs at FDA [https://www.fda.gov/science-research/science-and-research-special-topics/nanotechnology-programs-fda]
- 116. Nanotechnology: The vision of 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4131398/]
- 117. Regulatory assessment of nano-enabled health products in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10018019/]
- 118. EMA/HMA – Publication of the Nanotechnology-based ... [https://elsibi.hypotheses.org/24840]
- 119. Regulatory pathways and guidelines for nanotechnology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11919859/]
- 120. Nanotechnology Drug Delivery Market Size | Forecast - 2032 [https://www.alliedmarketresearch.com/nanotechnology-drug-delivery-market-A10459]
- 121. Nanotechnology Drug Delivery Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/nanotechnology-drug-delivery-market]
- 122. Nanotechnology Drug Delivery Market Projected to Reach ... [https://www.globenewswire.com/news-release/2025/11/26/3195125/0/en/Nanotechnology-Drug-Delivery-Market-Projected-to-Reach-USD-200-77-Billion-by-2032-Owing-to-Prevalence-of-Chronic-Diseases-Advances-in-Nanomedicine-SNS-Insider.html]
- 123. Nanotechnology Drug Delivery Market Share & Forecast 2035 [https://www.transparencymarketresearch.com/nanotechnology-drug-delivery-market.html]
- 124. Nanotechnology Drug Delivery Market Size to Hit USD ... [https://www.precedenceresearch.com/nanotechnology-drug-delivery-market]
- 125. Nanotechnology Drug Delivery Market Size and Forecast ... [https://www.researchnester.com/reports/nanotechnology-drug-delivery-market/7444]
- 126. Experimental Methods for the Biological Evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9959606/]
- 127. Nanopharmaceuticals and nanomedicines currently on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6391637/]
- 128. Nanotechnology advances for biomedical applications [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1639506/full]
- 129. Key trends and technologies in drug delivery for 2025 and ... [https://www.europeanpharmaceuticalreview.com/article/254459/key-trends-and-technologies-in-drug-delivery-for-2025-and-beyond/]