Germline-Targeting vs. Lineage-Based Vaccines: A Comparative Analysis of Next-Generation Immunization Strategies
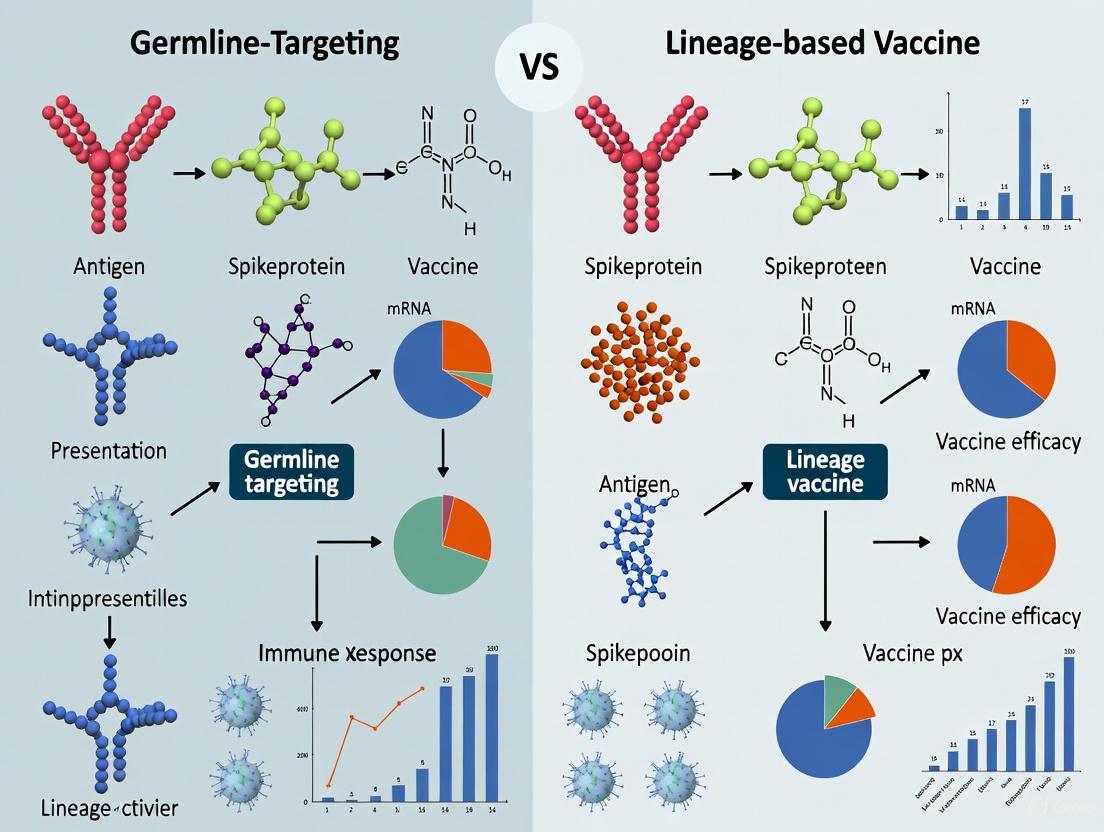
This article provides a comprehensive comparative analysis of two pioneering vaccine strategies: germline-targeting and lineage-based approaches.
Germline-Targeting vs. Lineage-Based Vaccines: A Comparative Analysis of Next-Generation Immunization Strategies
Abstract
This article provides a comprehensive comparative analysis of two pioneering vaccine strategies: germline-targeting and lineage-based approaches. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles, methodological applications, and current challenges of these platforms. Germline-targeting, exemplified by HIV vaccine trials, uses sequential immunogens to guide B cells toward producing broadly neutralizing antibodies. In contrast, lineage-based strategies, used for rapidly mutating viruses like SARS-CoV-2, adapt vaccine formulations to match circulating viral strains. The scope spans from conceptual frameworks and preclinical design to clinical validation, synthesizing recent data to evaluate the relative effectiveness, advantages, and optimal use cases for each strategy in modern vaccinology.
Conceptual Frameworks: From Empirical Design to Rational Vaccine Engineering
The rapid evolution of pathogens like HIV and influenza presents a monumental challenge for traditional vaccinology. In response, two pioneering strategies have emerged: germline-targeting and lineage-based vaccine design. Both aim to guide the immune system toward generating broadly neutralizing antibodies (bNAbs) that can protect against diverse viral variants. While they share this ultimate goal, they are founded on distinct core principles and scientific approaches. Germline-targeting focuses on reverse-engineering immunogens to engage rare, naive B cell precursors with known bNAb potential. In contrast, the lineage-based approach leverages natural infection history, using computational reconstruction of mature bNAb lineages from infected individuals to design immunogens that recapitulate this maturation pathway. This guide provides a comparative analysis of these strategies, examining their theoretical foundations, methodological workflows, and supporting clinical data to inform researchers and drug development professionals.
Core Principle Comparison
The following table summarizes the foundational concepts, objectives, and technological underpinnings of each strategy.
Table 1: Core Principles of Germline-Targeting and Lineage-Based Vaccine Strategies
| Aspect | Germline-Targeting Strategy | Lineage-Based Strategy |
|---|---|---|
| Fundamental Principle | Reverse-engineering of immunogens to bind and activate rare naive B cells expressing B cell receptors (BCRs) with bNAb potential [1]. | Computational reconstruction of the natural maturation history of bNAb lineages from infected individuals to identify key mutations [1]. |
| Primary Objective | To "prime" rare bNAb-precursor B cells, initiating an immune response that can be sequentially guided toward breadth [2]. | To design immunogens that selectively promote the acquisition of critical "improbable" mutations required for neutralization breadth during the affinity maturation process [1]. |
| Key Technological Drivers | Structural biology, protein engineering, high-resolution epitope mapping, and next-generation sequencing for B cell repertoire analysis [1] [3]. | Single B cell cloning, deep sequencing, phylogenetic analysis, and in-silico lineage reconstruction [1]. |
| Role of Immunogen Series | A sequence of distinct, rationally designed immunogens administered to shepherd the primed B cell lineage toward broader neutralization [1] [2]. | A series of immunogens designed to mirror the natural evolutionary path of a bNAb lineage, selecting for B cells that acquire desired mutations [1]. |
| Dependency on Human Genetics | High; dependent on an individual's inherited immunoglobulin gene alleles (e.g., IGHV1-2*02 for VRC01-class bNAbs) [4]. | Less dependent on germline genetics; focuses on guiding the somatic hypermutation process after B cell activation. |
Experimental Protocols and Workflows
The translation of these core principles into effective vaccines requires distinct experimental pipelines. The methodologies below outline the key steps for each strategy, from initial design to clinical evaluation.
Germline-Targeting Workflow
This pipeline involves engineering an immunogen to initiate a desired B cell response.
- Identification of a Target bNAb: Isolate and characterize a potent bNAb from a chronically infected individual. A prominent example is VRC01, which targets the CD4-binding site of HIV Env [1] [5].
- Lineage Analysis and Ancestral Reconstruction: Trace the evolutionary lineage of the mature bNAb back to its inferred germline (unmutated common ancestor) sequence.
- Priming Immunogen Design: Use structural biology (e.g., X-ray crystallography, Cryo-EM) to engineer a immunogen, such as eOD-GT8, that is specifically tailored to have high affinity for the germline-encoded BCR of the target bNAb lineage [1] [2].
- Preclinical Validation: Test the engineered immunogen in animal models, such as knock-in mice expressing humanized BCRs, to confirm its ability to activate the desired naive B cell precursors [3].
- Clinical Trial Evaluation (Priming): Evaluate the immunogen in Phase I trials for safety and its ability to induce targeted B cell responses in humans. Success is measured by the frequency of precursor B cells in blood samples, often using flow cytometry and B cell receptor sequencing [2] [4]. The IAVI G001 and G002 trials are key examples [1] [2].
- Boosting Immunogen Design and Testing: Develop and test a series of distinct, sequentially administered immunogens (e.g., Core-g28v2 and 426c.Mod.Core) designed to bind intermediates of the maturing B cell lineage, guiding them toward broader neutralization [1] [2].
Lineage-Based Workflow
This approach focuses on recapitulating a known successful immune response.
- bNAb Donor Selection: Identify individuals living with HIV (PLWH) who have naturally developed potent bNAb responses after years of infection [1].
- Longitudinal Sampling and Deep Sequencing: Collect blood samples over time to capture the temporal development of the bNAb response. Isolate and sequence the B cell receptors from antigen-specific memory B cells and plasma cells.
- Phylogenetic Lineage Reconstruction: Use computational tools to build a phylogenetic tree from the sequenced BCRs, mapping the evolutionary pathway from the germline ancestor to the mature bNAb [1].
- Identification of Key Mutations: Analyze the lineage to pinpoint critical somatic hypermutations (SHMs) that are essential for conferring neutralization breadth and potency. These are often termed "improbable" mutations [1].
- Intermediate Immunogen Design: Design immunogens that specifically bind to and select for B cell clones that have acquired these key intermediate mutations. The goal is to design a vaccination series that mimics the natural antigenic drive that occurred during infection.
- Preclinical and Clinical Testing: Test the series of immunogens in animal models and subsequently in clinical trials to determine if they can guide developing B cell lineages along a pathway that results in the production of bNAbs.
The following diagram illustrates the logical sequence and key decision points for the germline-targeting strategy, as demonstrated in recent clinical trials.
Key Experimental Data and Clinical Evidence
Recent clinical trials have provided proof-of-concept for these strategies, yielding critical quantitative data on their immunogenicity and performance.
Germline-Targeting Clinical Trial Data
The IAVI-sponsored trials (G001, G002, and G003) represent a landmark in germline-targeting, using the eOD-GT8 60mer immunogen to prime VRC01-class B cell precursors.
Table 2: Summary of Key Outcomes from Germline-Targeting Clinical Trials
| Trial Identifier | Platform & Population | Intervention | Key Immunological Readout | Result |
|---|---|---|---|---|
| IAVI G001 [1] [2] | Protein (eOD-GT8 60mer) with AS01B adjuvant; 48 participants | Two priming doses | Frequency of VRC01-class IgG B cells among memory B cells | 97% response rate (35/36). Median frequency: 0.09% (low dose) and 0.13% (high dose) of MBCs. |
| IAVI G002 [2] | mRNA-LNP (North America); 60 participants | Prime (eOD-GT8) + Heterologous Boost (Core-g28v2) | Development of VRC01-class responses; acquisition of somatic hypermutations (SHMs) | 100% (17/17) in the prime-boost group developed VRC01-class responses. >80% showed "elite" responses with multiple critical SHMs. |
| IAVI G003 [2] | mRNA-LNP (Rwanda & South Africa); 18 participants | Two priming doses | Activation of target naive B cells | 94% response rate (17/18), demonstrating feasibility in key target populations. |
Illustrative Data from a Lineage-Based Approach
While the search results provide more extensive clinical data for germline-targeting, they also describe the rationale and early progress for the lineage-based strategy. One report discussed the use of the BG505 SOSIP GT1.1 native-like trimer immunogen, which is modified to bind both VRC01-class and apex-specific B cell precursors. In infant macaques, three immunizations with this candidate led to expanded VRC01-class B cells that "accumulated several mutations associated with VRC01-class bNAbs," suggesting the antibodies were being guided toward a broad and potent state [1]. This exemplifies the lineage-based goal of using immunogens to promote specific, desirable mutations during the maturation process.
The Scientist's Toolkit: Essential Research Reagents
The development and evaluation of these advanced vaccine strategies rely on a suite of sophisticated research reagents and assays.
Table 3: Essential Reagents and Methods for Germline-Targeting and Lineage-Based Research
| Research Reagent / Assay | Primary Function | Strategic Application |
|---|---|---|
| Stabilized Envelope Trimers (e.g., SOSIP, Native-like) | Antigens that mimic the native structure of viral surface proteins (e.g., HIV Env); key immunogens [1] [6]. | Core component of both strategies; used to focus immune responses on neutralization-sensitive epitopes. |
| Next-Generation Sequencing (NGS) | High-throughput sequencing of B cell receptor (BCR) repertoires from immunized subjects [1]. | Critical for tracking B cell lineage dynamics, measuring SHM, and confirming the engagement of target B cell clones. |
| Cryo-Electron Microscopy (Cryo-EM) | High-resolution structural determination of antigen-antibody complexes [1] [6]. | Informs the rational design of immunogens by revealing atomic-level interactions with bNAbs and their precursors. |
| BLI / SPR Biosensors (e.g., Biolayer Interferometry, Surface Plasmon Resonance) | Label-free quantification of binding kinetics (affinity, kon, koff) between antibodies and antigens [1]. | Used to validate immunogen binding to germline and intermediate BCRs, a key parameter in germline-targeting. |
| IGHV Genotyping | Nucleotide-level identification of an individual's inherited immunoglobulin gene alleles [4]. | Essential for patient stratification in germline-targeting trials, as response is dependent on alleles like IGHV1-2*02. |
| Pseudovirus Neutralization Assay | Gold-standard in vitro measurement of antibody function against a panel of diverse viral variants [1] [7]. | The definitive functional assay for determining the breadth and potency of vaccine-elicited neutralizing antibodies. |
The following diagram maps the relationship between these core tools and the specific research questions they help answer within the vaccine development workflow.
Germline-targeting and lineage-based vaccine strategies represent two sophisticated, complementary paradigms in the pursuit of broadly protective immunity. The germline-targeting approach has demonstrated formidable clinical proof-of-concept, with trials like IAVI G002 showing that a prime-boost regimen can successfully initiate and then further mature VRC01-class B cell responses in humans [2]. Its main challenge lies in its inherent dependency on specific human immunoglobulin gene alleles, necessitating careful patient stratification or immunogen designs with broader specificity [4]. In contrast, the lineage-based approach seeks to recapitulate nature's proven path to breadth by guiding B cells through a pre-defined series of mutations, potentially offering a more "agnostic" entry point that is less constrained by germline genetics [1].
The future of vaccine development against highly variable pathogens will likely involve a synergistic integration of both concepts. Germline-targeting immunogens could be used to initiate the response, with subsequent boosts informed by lineage analyses to shepherd the B cells toward full maturity and breadth. As these platforms mature, leveraging mRNA for faster immunogen iteration and advanced adjuvants to shape the immune response, they hold promise not only for HIV but for other antigenically complex pathogens like influenza and future pandemic threats [6].
The development of effective vaccines against highly variable viruses such as HIV-1 and SARS-CoV-2 represents one of the most significant challenges in modern immunology. These pathogens employ sophisticated immune evasion strategies, including rapid genetic mutation, structural mimicry of host antigens, and glycan shielding of conserved epitopes [8] [9]. HIV-1, with its extraordinary global diversity and ability to establish latent reservoirs, has proven particularly recalcitrant to conventional vaccine approaches [10] [9]. Despite nine completed HIV-1 vaccine efficacy trials, only one has demonstrated modest efficacy, highlighting the formidable nature of this challenge [10].
In response to these challenges, the vaccine research community has developed two pioneering strategies: germline-targeting and B-cell lineage vaccine design [10]. Both approaches aim to guide the immune system through complex maturation pathways to generate broadly neutralizing antibodies (bNAbs) capable of recognizing diverse viral variants. This review provides a comparative analysis of these strategies, examining their underlying mechanisms, experimental support, and potential for addressing viral diversity and immune evasion.
Theoretical Foundations and Mechanisms
Germline-Targeting Vaccine Strategy
Germline-targeting represents a structure-based reverse engineering approach designed to initiate B-cell responses that can eventually mature into bNAb-producing lineages [10] [11]. This strategy employs engineered immunogens specifically designed to activate rare naive B cells bearing B-cell receptors (BCRs) with potential to develop into bNAbs [12]. The fundamental premise is that the immune system must be deliberately guided through a predefined maturation pathway, as the stochastic natural immune response rarely produces bNAbs even during actual infection [8].
The germline-targeting approach requires sequential immunization with a series of increasingly native-like HIV Envelope immunogens [10]. The process begins with priming immunogens that engage precursor B cells, followed by booster immunogens that shepherd these cells along affinitity maturation pathways toward breadth and potency [12]. As researcher William Schief has described, this approach essentially involves "shepherding" the immune system through multiple shots containing multiple different antigens along a predefined path [12].
Lineage-Based Vaccine Strategy
Lineage-based vaccine design takes a different approach, leveraging computational reconstruction of antibody maturation pathways observed in natural infection [8]. This method analyzes the evolutionary history of bNAbs from HIV-infected individuals and uses this information to design sequential immunogens that recapitulate these pathways in vaccinated individuals [10] [8]. Rather than reverse-engineering from structural biology alone, this approach draws directly from successful antibody lineages that nature has already produced.
The lineage-based approach acknowledges that the antigen stimulating memory B cells during affinity maturation may differ from the antigen that initially activated naive B cells [8]. This insight necessitates using distinct antigens for prime and boost vaccinations to optimize clonal evolution [8]. Additionally, this approach must overcome host immunoregulatory mechanisms that often suppress the development of B cells producing antibodies with "disfavored" characteristics, such as polyreactivity or long heavy-chain third complementarity-determining regions commonly found in bNAbs [8].
Comparative Analysis of Strategic Approaches
Table 1: Comparison of Germline-Targeting and Lineage-Based Vaccine Strategies
| Feature | Germline-Targeting Approach | Lineage-Based Approach |
|---|---|---|
| Fundamental Principle | Structure-based reverse engineering of immunogens to engage precursor B cells [10] [12] | Computational reconstruction of natural antibody maturation pathways from infected individuals [10] [8] |
| Initiation Mechanism | Engineered immunogens bind rare naive B cells with bNAb potential [11] [12] | Immunogens designed based on ancestral antibodies from successful lineages [8] |
| Vaccination Series | Sequential immunization with increasingly native-like envelope immunogens [10] | Prime-boost with antigens representing different stages of lineage development [8] |
| Key Challenges | Engaging extremely rare B cell precursors (~1 in 300,000 naive B cells) [12]; Guiding through complex maturation pathways [11] | Overcoming host regulatory suppression of "disfavored" antibody characteristics; Recapitulating complex maturation pathways [8] |
| Technological Requirements | High-resolution structural biology; Immunogen engineering [12] | High-throughput antibody sequencing; Computational lineage reconstruction [8] |
| Representative Candidates | eOD-GT8 60mer nanoparticle [10] [12] | CH235 lineage-based immunogens [10] |
Synergistic Potential and Combination Approaches
Recent research has explored potential synergies between B-cell and T-cell vaccine approaches to optimize immune responses against HIV [10] [13]. The US National Institute of Allergy and Infectious Diseases (NIAID) convened a workshop in 2023 specifically to explore these synergies [10]. Preclinical studies suggest that combining B-cell and T-cell vaccine strategies can establish protection at lower, more attainable concentrations of bNAbs [10] [13].
Studies in non-human primates have demonstrated that combining HIV SOSIP protein vaccines with potent T-cell-inducing viral vectors provided better protection against SHIV challenge than either candidate alone [13]. Importantly, the combination was protective even with sub-optimal titers of neutralizing antibodies [10]. Similarly, vaccine-mediated induction of potent T-cell responses lowered the antibody threshold needed to prevent SARS-CoV-2 infection in non-human primates [10]. These findings suggest a promising framework where bNAbs provide sterilizing immunity while T-cell responses control infected cells that escape neutralization [10].
Experimental Models and Methodologies
Key Experimental Models for Vaccine Evaluation
Table 2: Experimental Models for Vaccine Assessment
| Model System | Application | Key Readouts | Advantages | Limitations |
|---|---|---|---|---|
| Non-Human Primates (NHPs) | SHIV challenge studies [10] [13] | Neutralizing antibody titers; Protection against infection [10] | Physiologically relevant immune system; Mucosal challenge possible [10] | Costly; Limited availability; SHIV not identical to HIV [10] |
| Mouse Models with Humanized Immune Systems | Initial testing of germline-targeting immunogens [12] | Activation of specific B cell precursors; Germinal center responses [12] | Can engraft human B cell precursors; Controlled experimental conditions [12] | Incomplete human immune system reconstitution [12] |
| In Vitro Binding and Neutralization Assays | Screening immunogen-antibody interactions [10] | Binding affinity and kinetics; Neutralization breadth and potency [10] | High-throughput capability; Quantifiable results [10] | Does not capture full immune system complexity [10] |
| Clinical Trials | Evaluation of safety and immunogenicity in humans [10] | bNAb precursor frequency; IgG+ B cells in blood [10] | Direct relevance to human immune responses [10] | Ethical and safety constraints; Costly and time-consuming [10] |
Representative Experimental Protocols
Germline-Targeting Clinical Trial Protocol (IAVI G001)
The IAVI G001 trial represented a landmark proof-of-concept for germline-targeting [12]. This Phase I trial evaluated the eOD-GT8 60mer nanoparticle immunogen, designed to activate naive B cells capable of producing VRC01-class bNAbs targeting the CD4 binding site [12]. The methodology involved:
- Participant Cohort: Healthy adult volunteers without HIV
- Immunization Schedule: Prime and boost vaccinations at designated intervals
- Immunogen: eOD-GT8 60mer nanoparticle administered intramuscularly
- Primary Endpoints: Safety and tolerability of the vaccine regimen
- Key Immunological Assays: Flow cytometry to quantify VRC01-class B cell precursors; ELISA to measure antibody responses; memory B cell characterization [12]
The trial successfully demonstrated that 97% of vaccinees showed VRC01-class bNAb precursors with a median frequency of 0.1% IgG+ B cells in blood, providing critical proof-of-concept for germline-targeting [10] [12].
Lineage-Based Vaccine Assessment in NHPs
A representative preclinical study evaluating lineage-based vaccines involves:
- Immunogen Series: Sequential immunization with immunogens representing different stages of identified bNAb lineages
- Animal Model: Rhesus macaques
- Challenge Model: SHIV challenge via mucosal route
- Immunological Monitoring: Longitudinal assessment of antibody breadth and potency using neutralization panels; B cell sorting and sequencing to track lineage development
- Correlates of Protection: Association between specific antibody responses and protection from infection [10]
Key Research Reagents and Experimental Tools
Essential Research Reagents
Table 3: Key Research Reagents for Vaccine Development
| Reagent Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| Engineered Immunogens | eOD-GT8 60mer; SOSIP trimers; CH848 ferritin nanoparticles | Activate specific B cell precursors; Guide antibody maturation | [10] [12] |
| Adjuvant Systems | 3M-052 aqueous formulation; Saponin/MPLA nanoparticles; Alum | Enhance immunogenicity; Modulate immune response quality | [10] |
| Delivery Platforms | mRNA-LNP; Adenovirus vectors; DNA plasmids with electroporation | Present immunogens; Enhance cellular uptake; Promote sustained antigen expression | [10] [12] |
| Animal Models | SHIV in rhesus macaques; Humanized mouse models | Preclinical efficacy assessment; Study of B cell responses in vivo | [10] [13] |
| Analysis Tools | High-throughput B cell sequencing; Neutralization assays; Structural biology techniques | Characterize immune responses; Determine antibody breadth and potency; Guide immunogen design | [10] [8] |
Signaling Pathways and Experimental Workflows
B Cell Activation and Maturation Pathway
B Cell Maturation to bNAb Producer - This diagram illustrates the sequential process of guiding B cells from naive precursors to bNAb-producing cells through germline-targeting and sequential immunization.
Sequential Immunization Workflow
Sequential Immunization Workflow - This diagram outlines the systematic approach for guiding the immune system through sequential immunizations to generate bNAb responses.
The comparative analysis of germline-targeting and lineage-based vaccine strategies reveals complementary approaches to addressing the fundamental challenges of viral diversity and immune evasion. While both strategies aim to induce bNAbs through sequential immunization, they differ in their starting points and design principles. Germline-targeting begins with structure-based engineering to engage precise B cell precursors, while lineage-based approaches leverage natural antibody evolution from infected individuals.
Recent advances in mRNA delivery platforms and adjuvant technologies have accelerated both strategies, enabling more rapid iteration and optimization of vaccine candidates [10]. The demonstrated success of germline-targeting in priming desired B cell responses in clinical trials provides proof-of-concept for this approach [10] [12]. Meanwhile, lineage-based designs benefit from following nature's blueprint for effective antibody responses.
Future HIV vaccine regimens will likely incorporate elements from both strategies, potentially combined with T-cell vaccine components to create synergistic protection [10] [13]. As the field progresses, the integration of structural biology, computational design, and deep understanding of B cell biology will be essential to develop vaccines capable of overcoming viral diversity and immune evasion mechanisms. The scientific imperative to address these challenges remains critical for controlling not only HIV but other highly variable pathogens with pandemic potential.
The development of a protective HIV vaccine represents one of the most formidable challenges in modern immunology. Traditional vaccine approaches have consistently failed to provide appreciable protection, largely due to the virus's extraordinary genetic diversity and sophisticated immune evasion strategies [1]. In response, researchers have pioneered novel immunization strategies designed to overcome these obstacles through precise engineering of the immune response.
Two leading approaches have emerged: germline-targeting and lineage-based vaccination strategies. While both aim to elicit broadly neutralizing antibodies (bNAbs), they differ fundamentally in their initial mechanisms. Germline-targeting employs reverse-engineered immunogens specifically designed to activate rare naïve B cells possessing genetic signatures characteristic of bNAb precursors [1] [14]. In contrast, lineage-based approaches leverage the reconstructed maturation pathways of known bNAbs to guide B cell development [1].
This review provides a comparative analysis of these strategies, focusing on their mechanistic foundations, clinical validation, and potential for integration into a globally effective HIV vaccine regimen.
Comparative Analysis of Strategic Approaches
Table 1: Core Strategic Comparison Between Germline-Targeting and Lineage-Based Vaccine Approaches
| Feature | Germline-Targeting Strategy | Lineage-Based Strategy |
|---|---|---|
| Core Principle | Structure-based immunogen design to activate rare naïve B cell precursors with bNAb potential [1] [14] | Computational reconstruction of bNAb maturation history to design immunogens that promote key mutations [1] |
| Initial Target | Naïve B cells expressing BCRs with specific germline-encoded features (e.g., IGHV1-2*02 for VRC01-class) [4] | Memory B cells, guiding pre-selected lineages toward breadth [1] |
| Immunogen Sequence | Predefined series of immunogens with increasing native-like structure [1] [14] | Immunogens designed to select for specific, critical improbable mutations [1] |
| Key Advantage | Ability to initiate responses from an extremely rare precursor pool [1] [2] | Strategy informed by known, effective bNAb maturation pathways [1] |
Key Experimental Findings and Clinical Validation
Proof-of-Concept Clinical Trials
Recent clinical trials have demonstrated the feasibility of the germline-targeting approach in humans. The IAVI G001 trial used the eOD-GT8 60mer immunogen to prime VRC01-class B cell precursors, achieving a 97% response rate (35 of 36 participants) [1] [2]. Subsequent trials IAVI G002 (North America) and IAVI G003 (Africa) utilized an mRNA platform to deliver the same immunogen, showing similarly high response rates and demonstrating cross-population applicability [2].
A critical finding from these studies was the impact of human genetic variation on vaccine response. Individuals lacking permissive IGHV1-2 alleles (specifically *02 or *04) failed to generate VRC01-class responses, highlighting the necessity of considering population-level immunoglobulin allelic variations in vaccine design [4].
Table 2: Summary of Key Clinical Trial Outcomes for Germline-Targeting Vaccines
| Trial Identifier | Immunogen/Platform | Key Findings | Response Rate |
|---|---|---|---|
| IAVI G001 [2] | eOD-GT8 60mer protein + AS01B adjuvant | Successful priming of VRC01-class bnAb precursors; dose-effect observed confounded by IGHV genotype [4] | 35 of 36 participants (97%) [1] |
| IAVI G002 [2] | eOD-GT8 60mer mRNA prime, core-g28v2 60mer mRNA boost | Heterologous boost drove further maturation; "elite" responses with multiple beneficial mutations in >80% of boosted participants [2] | 17 of 17 in prime-boost group (100%) [2] |
| IAVI G003 [2] | eOD-GT8 60mer mRNA (prime only) in African cohorts | Successful priming of VRC01-class B cells in African populations; responses similar to North American trials [2] | 17 of 18 participants (94%) [2] |
| HVTN 301 [1] | 426 c.Mod.Core nanoparticle | Isolation of 38 mAbs with similarities to VRC01-class antibodies; currently under characterization | Data pending |
Preclinical Evidence for Combination Approaches
Beyond targeting single epitopes, research has progressed to evaluating regimens that simultaneously initiate multiple bNAb lineages. A seminal non-human primate study demonstrated that immunization with a combination of three distinct germline-targeting immunogens (targeting the V3-glycan site, V2 Apex, and MPER) could concurrently prime bnAb precursor lineages to all three epitopes without apparent interference [15]. This finding supports the development of multivalent HIV vaccine regimens aiming to elicit a polyclonal bNAb response, which would be critical for overcoming viral diversity and escape mutants.
Essential Research Reagents and Methodologies
The advancement of germline-targeting vaccines relies on a specialized toolkit of reagents and analytical techniques.
Table 3: Essential Research Reagent Solutions for Germline-Targeting Vaccine Development
| Research Reagent / Tool | Function and Application | Example Use Case |
|---|---|---|
| Engineered Priming Immunogens (e.g., eOD-GT8 60mer, BG505 SOSIP GT1.1) [1] [14] | Activate rare, naïve B cells bearing specific germline-encoded BCRs. | eOD-GT8 60mer used in IAVI G001, G002, and G003 trials to prime VRC01-class precursors [2]. |
| Native-like Env Trimers | Serve as boosting immunogens to guide primed B cells toward broader neutralization. | BG505 SOSIP GT1.1 trimer used to expand and mutate VRC01-class B cells in macaques [1]. |
| mRNA-LNP Vaccine Platform [2] [6] | Enables rapid production and potent delivery of encoded immunogens; can induce strong germinal center responses. | Moderna's mRNA platform used in IAVI G002/G003 trials, found to be at least as effective as protein immunization [1]. |
| IGHV Genotyping & Repertoire Analysis [4] | Identifies permissive immunoglobulin alleles in trial participants and quantifies precursor frequency. | Personalised genotyping in IAVI G001 linked IGHV1-2*02 allele to higher precursor frequency and response [4]. |
| B Cell Isolation & Characterization | Isolate antigen-specific B cells and characterize their antibodies. | 38 vaccine-induced mAbs isolated in HVTN 301 trial for characterization by BLI and cryo-EM [1]. |
Key Experimental Workflow and Signaling
The following diagram visualizes the core experimental workflow and the critical B cell receptor signaling pathway involved in activating rare B cell precursors through a germline-targeting vaccine.
Detailed Experimental Protocols
Protocol: Assessment of Vaccine-Induced VRC01-Class B Cell Responses
This protocol is adapted from the methods used in the IAVI G001, G002, and G003 clinical trials [2].
Sample Collection: Collect peripheral blood mononuclear cells (PBMCs) from trial participants at baseline and at predetermined intervals post-vaccination (e.g., weeks 4, 8, and 10).
B Cell Sorting and Culture:
- Isolate memory B cells or antigen-specific B cells using fluorescence-activated cell sorting (FACS). For VRC01-class cells, use labeled eOD-GT8 or related probes.
- Culture sorted B cells and stimulate them to differentiate into antibody-secreting cells.
Antibody Sequencing and Analysis:
- Extract RNA from single B cells and synthesize cDNA.
- Amplify immunoglobulin heavy and light chain variable regions using PCR.
- Sequence the amplified products and analyze the sequences for:
- IGHV1-2 Gene Usage: Confirm use of IGHV1-2*02 or *04 alleles [4].
- Somatic Hypermutation (SHM): Calculate the mutation frequency relative to the inferred germline sequence.
- Lineage Analysis: Track the clonal evolution of B cell lineages over time.
Functional Characterization:
- Express the recombinant monoclonal antibodies from the sequenced pairs.
- Evaluate binding affinity and kinetics to the immunogen using biolayer interferometry (BLI).
- Test neutralization breadth and potency against a panel of diverse HIV pseudoviruses in a TZM-bl neutralization assay.
Protocol: IGHV Genotyping and Naïve B Cell Repertoire Analysis
This protocol is based on the work that revealed the critical role of IGHV1-2 allelic variation [4].
Library Preparation:
- Isulate naïve B cells (e.g., CD19+IgM+IgD+) from participant PBMCs.
- Construct IgM libraries from these cells, incorporating unique molecular identifiers (UMIs) during cDNA synthesis to ensure accurate sequence quantification.
High-Throughput Sequencing: Perform deep sequencing of the immunoglobulin heavy chain loci on a platform such as Illumina.
Germline Allele Inference:
- Use a germline allele inference tool (e.g., IgDiscover) to determine the individual's IGHV genotype with nucleotide-level precision [4].
- Identify all alleles, including single-nucleotide variants.
Repertoire Quantification:
- Map sequence reads to the personalized genotype.
- Calculate the frequency of specific alleles (e.g., IGHV1-2*02 vs. *04) in the naïve repertoire by counting UMIs.
- Count unique heavy chain complementarity-determining region 3 (HCDR3) sequences to estimate the number of unique B cells for each allele.
Germline-targeting vaccines have transitioned from a theoretical concept to a clinically validated strategy for initiating the complex process of eliciting HIV bNAbs. Direct comparative evidence, notably from the IAVI G002 trial, demonstrates that a heterologous prime-boost regimen can drive these early responses toward a more mature state, a key milestone on the path to breadth [2]. The critical influence of human IGHV genotyping on response magnitude underscores the need for personalized vaccinology approaches and the development of a diverse portfolio of immunogens to achieve global coverage [4].
The future of HIV vaccine development likely lies in combination strategies—both in terms of eliciting multiple bNAb classes simultaneously [15] and in potentially integrating germline-targeting and lineage-based approaches in a single regimen. Continued advances in immunogen design, platform delivery (like mRNA), and a deep understanding of human B cell immunology will be essential to guide these rare B cell precursors to become potent, broad, and protective antibody responses.
The field of vaccinology has undergone a revolutionary transformation from empirical discovery to rational, structure-based design. Historically, most successful vaccines were developed empirically through an "isolate, inactivate or attenuate, and inject" approach, without a detailed understanding of the immunological mechanisms underlying protection [16]. While this approach led to tremendous successes against various infectious diseases, it proved inadequate for addressing more complex pathogens such as HIV, influenza, and dengue viruses [16]. The major hurdles included identifying early markers of vaccine efficacy, developing relevant antigens and adjuvants, defining correlates of protection, and understanding mechanisms underlying long-lasting protective immune responses [16].
The rapid emergence of high-throughput 'Omics' methodologies has enabled a comprehensive view of the dynamic responses to vaccines at a cellular and molecular level, giving rise to the field of systems vaccinology [16]. This review traces the historical evolution from empirical approaches to modern structure-based vaccine design, comparing the effectiveness of different strategies and providing the experimental frameworks that have enabled these advances.
Historical Foundations of Empirical Vaccine Development
The Empirical Era
The history of vaccination began long before the understanding of immunology. The earliest documented practices date back to 16th century China and India with variolation against smallpox, which involved inoculation of smallpox pus or scabs through nasal or cutaneous routes [17]. In 1796, Edward Jenner famously demonstrated that inoculation with cowpox lesions could confer immunity against smallpox, leading to the first vaccine (derived from "Vacca," Latin for cow) [17] [18]. For nearly two centuries following this breakthrough, vaccine development proceeded primarily through empirical observation and optimization:
- Late 1800s: Louis Pasteur developed live attenuated vaccines against rabies [17]
- Early 1900s: Chemically inactivated toxins (toxoids) and killed bacteria were introduced for diphtheria and tetanus [18]
- 1920s: Gaston Ramon discovered adjuvants by observing that materials like starch and saponins increased inflammatory responses to diphtheria toxoid [18]
- 1926: Alexander Glenny found that potassium aluminum sulfate (alum) enhanced antibody responses, leading to the most common vaccine adjuvant [18]
- 1930s: Development of viral cultivation techniques enabled influenza and yellow fever vaccines [17]
- 1950s: The golden age of vaccines introduced polio, measles, mumps, rubella, and varicella vaccines [17]
Limitations of the Empirical Approach
While empirically developed vaccines have saved millions of lives, the approach faced significant limitations:
- Mechanistic understanding: The mechanisms of action (MOA) of successful vaccines and adjuvants remained largely unknown [18]
- Development bottlenecks: Difficult-to-target pathogens resisted empirical approaches
- Standardization challenges: Reliable standardized assays to predict protective efficacy were unavailable [16]
- Antigen selection: Identification of protective antigens was time-consuming and labor-intensive
Table 1: Key Milestones in Empirical Vaccine Development
| Time Period | Development | Key Examples | Limitations |
|---|---|---|---|
| 1796-1900 | Live attenuated vaccines | Smallpox, Rabies | Safety concerns, unknown mechanisms |
| 1920-1950 | Inactivated vaccines & toxoids | Diphtheria, Tetanus, Pertussis | Weaker immune responses, required adjuvants |
| 1950-1980 | Cell culture-based vaccines | Polio, Measles, Mumps, Rubella | Technical challenges in viral cultivation |
| 1980s-present | Polysaccharide conjugate vaccines | Pneumococcal, Meningococcal | Limited to certain pathogen types |
The Transition to Rational Vaccine Design
Technological Enablers of Rational Design
The transition from empirical to rational vaccine design was facilitated by several technological advances:
- High-throughput Omics methodologies: Genomics, transcriptomics, proteomics, and metabolomics enabled comprehensive monitoring of systemic changes at molecular, cellular, and organism levels following vaccination [16]
- Structural biology tools: X-ray crystallography and nuclear magnetic resonance (NMR) allowed determination of 3D structures of viral proteins and antigen-antibody complexes [16]
- Computational capabilities: Advanced algorithms for theoretical predictions of antigen-antibody interactions [16]
- Bioorthogonal chemistry and proteomics: Enabled identification and isolation of cell receptors for adjuvants [18]
Systems Vaccinology Framework
Systems vaccinology has emerged as a key discipline that integrates multiple types of data over time to create predictive models of vaccine-induced immunity [16]. This approach involves:
- Monitoring different components of the biological system in response to vaccination
- Integrating multiple types of Omics data over time
- Creating mathematical models to predict system structure and behavior
- Testing and validating novel hypotheses through iterative experimentation [16]
Key findings from systems vaccinology studies include the identification of molecular signatures of vaccine efficacy. For example, studies of the yellow fever vaccine YF-17D revealed interferon and innate antiviral gene signatures predictive of CD8+ T cell and neutralizing antibody responses [16]. Similarly, transcriptional signatures induced by inactivated trivalent influenza vaccine revealed markers associated with plasmablast expansion that predicted antibody responses [16].
Structure-Based Vaccine Design Strategies
Reverse Vaccinology
Reverse vaccinology represents a fundamental shift from traditional methods. This approach involves:
- Computational mining and analysis of large datasets related to immune responses to pathogens
- Analysis of host-pathogen interactions and genomic data from both host and pathogen
- Prediction of promising antigen candidates through bioinformatic analysis
- Large-scale sampling of potential antigens with down-selection based on affinity for antibodies or MHC molecules [16]
Structural Vaccinology
Structural vaccinology utilizes detailed structural information to design optimized antigens:
- Structure-function analysis: Using structures of viral proteins and antigen-antibody complexes for docking and modeling studies [16]
- Epitope grafting: Transplanting linear and discontinuous epitopes onto computationally designed scaffolds [16]
- Stabilization of native conformations: Engineering antigens to maintain preferred conformations for optimal immune recognition
This approach has been successfully used to develop immunogenic vaccine candidates from respiratory syncytial virus (RSV) glycoprotein and MERS virus spike protein [16].
Germline-Targeting Vaccine Design
For difficult targets like HIV, germline-targeting represents a sophisticated structure-based approach:
- Immunogen design: Creating "germline-targeting" immunogens that can activate rare and low-affinity broadly neutralizing antibody (bnAb) precursor B cells [19]
- Lineage-based design: Guiding the maturation of bnAb precursors through sequential immunization with a series of engineered immunogens [19]
The development of bnAbs against HIV is particularly challenging because these antibodies often exhibit unusual properties including long heavy-chain complementarity-determining region 3 loops and/or autoreactivity, which normally trigger immune tolerance mechanisms [19]. Additionally, mature bnAbs contain a large number of somatic mutations, suggesting that prolonged germinal center reactions are needed for their development [19].
Table 2: Comparison of Vaccine Design Strategies
| Design Strategy | Key Principles | Application Examples | Advantages | Limitations |
|---|---|---|---|---|
| Empirical | Attenuation, inactivation, observation of natural immunity | Smallpox, Rabies, Polio, Measles | Proven success, straightforward | Limited for complex pathogens, slow |
| Reverse Vaccinology | Genome mining, computational prediction | Meningococcus B | Identifies novel antigens, high-throughput | Limited by prediction accuracy |
| Structural Vaccinology | Structure-based antigen design, epitope scaffolding | RSV, MERS | Precision targeting, rational optimization | Requires detailed structural data |
| Germline-Targeting | Sequential immunization, lineage guidance | HIV clinical trials | Can target difficult epitopes | Complex immunogen series required |
Comparative Analysis: Germline-Targeting vs. Lineage-Based Strategies
Germline-Targeting Approaches
Germline-targeting strategies focus on the initial activation of naive B cells expressing bnAb precursors:
- Immunogen design: Two primary approaches include well-folded native Envs based on transmitted/founder viruses from individuals who eventually generated bnAbs, and proteins engineered to bind unmutated common ancestors (UCAs) to mimic Env neutralizing epitopes [19]
- Affinity considerations: A key consideration is the affinity of the immunogen for B cell receptors expressed by naive bnAb precursor B cells [19]
- Validation tools: Transgenic mice expressing inferred UCA precursor BCRs are used to test immunogens' capacity to activate B cells with bnAb potential [19]
The eOD-GT8 60mer nanoparticle represents a promising germline-targeting immunogen that recently demonstrated success in a phase I clinical trial (NCT03547245, IAVI G001), where 97% of immunized individuals exhibited activated B cells with features of germline precursors of the VRC01 lineage [19].
Lineage-Based Vaccine Strategies
Lineage-based vaccine strategies aim to guide the maturation of bnAb responses through sequential immunization:
- Sequential immunogen series: A sequence of immunogens designed to selectively expand and mature bnAb lineages
- Somatic hypermutation guidance: Encouraging the accumulation of specific mutations required for breadth and potency
- Germinal center engagement: Promoting prolonged germinal center reactions to allow sufficient B cell maturation
Experimental Evidence and Clinical Validation
Recent clinical trials have provided critical insights into both strategies:
Table 3: Clinical Trials of Structure-Based HIV Vaccine Candidates
| Immunogen | Epitope Target | BnAb Lineage Targeted | Clinical Trial | Key Findings |
|---|---|---|---|---|
| eOD-GT8 | CD4 binding site | VRC01 | IAVI G001 (NCT03547245) | 97% of recipients showed activated B cells with germline precursor features [19] |
| BG505 SOSIP.gp140 | V3-glycan | PGT121 | IAVI C101 (NCT04224701) | Ongoing evaluation |
| CH505 TF gp120 | CD4 binding site | CH103 | HVTN 115 (NCT03220724) | Sequential immunization strategy |
| CH848 10.17DT | V3-glycan | DH270.6 | HVTN 3XX | Evaluating germline-targeting and lineage guidance |
The Antibody Mediated Prevention (AMP) trials provided proof-of-concept that bnAb-inducing vaccines could protect against HIV, demonstrating 75% protective efficacy against VRC01-sensitive viruses [19]. However, the lack of overall protection highlighted that high titers of neutralizing antibodies against a wide breadth of HIV isolates will be needed, likely requiring a mixture of bnAbs targeting different epitopes [19].
Experimental Protocols and Methodologies
Structural Biology Techniques
X-ray crystallography and 2D-NMR are essential for determining the spatial interactions between ligand functional groups and their receptors [18]. These techniques provide:
- Atomic-resolution structures of antigen-antibody complexes
- Identification of key residues involved in binding interactions
- Dynamic information about molecular movements (NMR)
- Foundation for structure-based design of improved antigens and adjuvants
Immunological Assays for Vaccine Evaluation
Compprehensive vaccine evaluation requires multiple complementary assays:
- Binding antibody measurements: ELISA, surface plasmon resonance to quantify antibody quantity and affinity [20]
- Neutralization assays: Pseudovirus and live virus neutralization to assess functional antibodies [20]
- T cell responses: ELISpot for IFN-γ production, multiparameter flow cytometry for T cell phenotyping [20]
- Gene expression profiling: Microarray or RNA-seq to identify transcriptional signatures [16]
- B cell repertoire analysis: High-throughput sequencing of B cell receptors [16]
Systems Vaccinology Workflows
The typical systems vaccinology workflow involves:
Diagram 1: Systems Vaccinology Workflow
The Scientist's Toolkit: Key Research Reagents and Technologies
Table 4: Essential Research Reagents for Structure-Based Vaccine Design
| Reagent/Technology | Function | Application Examples |
|---|---|---|
| Protein microarrays | High-throughput mapping of antibody and T cell reactivity to antigens [16] | Antigen discovery, epitope mapping |
| Monoclonal antibodies | Define neutralizing epitopes, provide structural insights [19] | bnAb isolation, passive protection studies |
| Transgenic mouse models | Test immunogens' capacity to activate bnAb precursor B cells [19] | Germline-targeting immunogen validation |
| Pseudovirus systems | Safe measurement of neutralization against dangerous pathogens [20] | Vaccine immunogenicity assessment |
| Mass cytometry (CyTOF) | High-dimensional single-cell analysis of immune responses | Comprehensive immunoprofiling |
| Next-generation sequencing | B cell and T cell receptor repertoire analysis [16] | Immune response characterization |
| Structural biology platforms | Determine atomic-level structures of antigens and complexes [16] [18] | Rational antigen design |
| Bioorthogonal chemistry | Identify and isolate cell receptors for adjuvants [18] | Mechanism of action studies |
Genetic Distance Models for Predicting Vaccine Effectiveness
Recent advances have enabled predictive modeling of vaccine effectiveness based on genetic distance between vaccine strains and circulating variants. Studies of COVID-19 vaccines have established that:
- Genetic distance (GD) in the receptor-binding domain (RBD) of SARS-CoV-2 is highly predictive of vaccine protection, accounting for 86.3-87.9% of VE variation [21]
- For every residue substitution on the RBD, VE decreases by an average of 5.2% for mRNA vaccines, 6.8% for viral vector vaccines, 14.3% for protein subunit vaccines, and 15.8% for inactivated vaccines [21]
- The VE-GD framework enables real-time predictions of vaccine protection against novel variants [21]
This approach demonstrates how structure-based understanding can inform vaccine deployment and public health responses against evolving pathogens.
Diagram 2: Genetic Distance Vaccine Effectiveness Model
The evolution from empirical to structure-based vaccine design represents a fundamental transformation in vaccinology. While empirical approaches successfully controlled many infectious diseases, they reached limitations against complex pathogens. Structure-based strategies, including reverse vaccinology, structural vaccinology, and germline-targeting, leverage detailed molecular understanding to design precision vaccines.
The comparative effectiveness of germline-targeting versus lineage-based vaccine strategies continues to be evaluated in preclinical and clinical studies. Current evidence suggests that successful vaccines against difficult targets will likely require combinations of approaches to elicit broad and potent immune responses. The integration of systems vaccinology with structure-based design provides a powerful framework for addressing remaining challenges in vaccine development, including rapidly evolving pathogens, antigenic variation, and the need for durable protection in diverse populations.
As the field advances, the continued refinement of predictive models based on genetic distance and structural features, coupled with high-resolution monitoring of immune responses, will enable more rational and effective vaccine design against emerging infectious threats.
From Bench to Bedside: Immunogen Design and Clinical Implementation
The development of a broadly effective HIV vaccine represents one of the most formidable challenges in modern immunology. This guide provides a comparative analysis of two pioneering vaccine strategies: germline-targeting versus lineage-based approaches. We focus specifically on the eOD-GT8 60-mer nanoparticle immunogen, examining its design rationale, clinical performance, and mechanistic advantages through structured experimental data, protocol details, and visual schematics. The data presented herein offer researchers a comprehensive resource for evaluating the relative merits of these distinct but complementary immunological strategies.
The quest for an HIV vaccine has evolved through multiple generations of candidates, from early protein subunits to viral vectors and multi-platform regimens [22]. The extraordinary genetic diversity and immune evasion tactics of HIV have necessitated increasingly sophisticated vaccine design strategies [13]. Two principal paradigms have emerged to address these challenges: germline-targeting and lineage-based vaccine approaches [1].
Germline-targeting employs reverse-engineered immunogens designed to bind and activate rare naïve B cells expressing precursors of broadly neutralizing antibodies (bNAbs) [1]. This strategy aims to initiate a carefully guided maturation pathway through sequential immunization with increasingly native-like HIV envelope immunogens.
Lineage-based vaccines computationally reconstruct the natural maturation history of bNAbs from HIV-infected individuals, using this roadmap to design sequential immunizations that shepherd B cell development toward bNAb production [1].
This guide objectively compares the performance of the leading germline-targeting candidate—the eOD-GT8 60-mer nanoparticle—against alternative strategies, providing researchers with experimental data and methodological details to inform future vaccine development.
Comparative Performance Analysis of Vaccine Strategies
Table 1: Strategic Comparison of HIV Vaccine Approaches
| Feature | Germline-Targeting (eOD-GT8) | Lineage-Based Approaches | Traditional Empirical Vaccines |
|---|---|---|---|
| Core Principle | Reverse-engineered immunogens to prime rare bNAb precursors [1] | Guide B cell maturation along reconstructed bNAb lineages [1] | Empirical testing of immune responses without precise B cell targeting |
| Target B Cells | Naïve B cells with BCRs having bNAb potential [23] [1] | Developing B cell lineages at various maturation stages | Polyclonal B cell responses without specific guidance |
| Immunogen Design | Structure-based engineering for specific BCR engagement [1] | Immunogens based on ancestral/intermediate sequences in bNAb lineages [1] | Natural pathogen antigens or empirical designs |
| Clinical Validation | Phase 1 trials (IAVI G001, G002) demonstrating precursor activation [23] [1] | Preclinical and early clinical development | Multiple Phase 2b/3 trials with limited efficacy [22] [13] |
| Key Advantage | Precision targeting of desired B cell precursors | Roadmap based on naturally evolved bNAbs | Established development pathway |
Table 2: Quantitative Clinical Trial Outcomes for eOD-GT8
| Trial Identifier | Platform | Dose | Response Rate | Key Immunological Readouts |
|---|---|---|---|---|
| IAVI G001 [23] [1] | Protein nanoparticle + AS01B adjuvant | 20 µg or 100 µg | 97% (35/36) with VRC01-class precursors; 84-93% with CD4+ T cell responses [23] | Median frequency of 0.1% IgG+ VRC01-class B cells in blood [1] |
| IAVI G002 [13] [1] | mRNA-LNP | Not specified | VRC01-class priming at least equivalent to G001 [1] | Higher number of mutations in IGHV1-2-using VRC01-class mAbs vs. G001 [1] |
eOD-GT8 Nanoparticle Design and Mechanism
The eOD-GT8 immunogen represents a paradigm shift in structure-based vaccine design. This engineered outer domain germline-targeting version 8 (eOD-GT8) is presented as a 60-mer self-assembling nanoparticle that mimics the spatial arrangement of HIV envelope proteins, enhancing B cell receptor cross-linking and activation [23] [1].
The immunogen is co-administered with AS01B adjuvant, which contains MPL (a TLR4 agonist) and QS-21 (a saponin derivative) to enhance innate immune activation and promote robust T follicular helper (Tfh) cell responses [23]. These Tfh cells are crucial for providing the necessary help to B cells during germinal center reactions, ultimately supporting the affinity maturation required for bNAb development.
Diagram Title: eOD-GT8 Germline-Targeting Mechanism
Experimental Protocols for Key Studies
IAVI G001 Clinical Trial Protocol
Objective: Evaluate safety and immunogenicity of eOD-GT8 60-mer nanoparticle with AS01B adjuvant in healthy adults [23] [1].
Methodology:
- Study Design: Randomized, double-blind, placebo-controlled Phase 1 trial
- Participants: 48 healthy HIV-negative adults
- Vaccination: Intramuscular injection at 0 and 2 months
- Doses: 20 µg or 100 µg eOD-GT8 with AS01B adjuvant
- Immunogenicity Assessment:
- Flow Cytometry: Detection of antigen-specific memory B cells
- ELISPOT: Quantification of antibody-secreting cells
- Luminex: Serum antibody binding to eOD-GT8 and LumSyn
- T Cell Assays: Intracellular cytokine staining for polyfunctional CD4+ T cell responses
Key Analysis: Frequencies of VRC01-class IgG+ B cells were quantified using fluorescently labeled eOD-GT8 probes. T cell epitope "hotspots" were mapped within both eOD-GT8 and lumazine synthase (LumSyn) proteins [23].
Antigen-Specific B Cell Analysis
Objective: Isolate and characterize monoclonal antibodies from vaccine-elicited B cells [1].
Methodology:
- B Cell Sorting: Single-cell sorting of antigen-specific memory B cells using fluorophore-conjugated eOD-GT8
- Antibody Cloning: Amplification of immunoglobulin heavy and light chain variable regions by RT-PCR
- Recombinant Expression: Production of monoclonal antibodies in HEK293T cells
- Binding Analysis: Biolayer interferometry (BLI) to determine antibody affinity and kinetics
- Neutralization Assessment: TZM-bl cell-based assays against HIV pseudoviruses
Key Analysis: 38 monoclonal antibodies from HVTN 301 trial recipients were characterized by BLI, neutralization assays, and cryo-electron microscopy to determine VRC01-class similarity [1].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Germline-Targeting HIV Vaccine Research
| Reagent / Solution | Function | Example Use |
|---|---|---|
| eOD-GT8 60-mer Nanoparticle | Prime immunogen for VRC01-class bNAb precursors [23] [1] | IAVI G001 and G002 clinical trials |
| AS01B Adjuvant | Enhance innate immunity and Tfh cell responses [23] | Administered with eOD-GT8 in IAVI G001 |
| mRNA-LNP Platform | Delivery system for encoded immunogens [13] [1] | IAVI G002 and G003 trials |
| Fluorophore-Labeled eOD-GT8 | Probe for identifying antigen-specific B cells [1] | Flow cytometry sorting of B cell precursors |
| Stabilized Env Trimers (SOSIP) | Boost immunogens to guide affinity maturation [13] [1] | Sequential immunization after prime |
| Biolayer Interferometry (BLI) | Measure antibody binding kinetics and affinity [1] | Characterization of isolated mAbs |
| Alhydrogel + CpG ODN | Adjuvant system for protein subunit vaccines [24] | Preclinical studies with various immunogens |
Diagram Title: Research Platforms and Assay Workflow
Discussion: Strategic Implications for Vaccine Development
The comparative data demonstrate that germline-targeting with eOD-GT8 successfully primes rare VRC01-class B cell precursors in most vaccine recipients, achieving a 97% response rate with a median frequency of 0.1% IgG+ B cells in peripheral blood [1]. This represents a significant milestone in structure-based vaccine design.
The mRNA platform (IAVI G002) appears to induce at least equivalent priming efficiency compared to the protein nanoparticle, with the potential advantage of driving greater somatic hypermutation in VRC01-class antibodies [1]. This suggests platform selection may influence the quality of the immune response.
Future development requires optimizing sequential immunization regimens to shepherd these primed B cells toward broad neutralization capacity. Combination approaches that engage both B cell and T cell immunity may lower the antibody titers required for protection, as demonstrated in preclinical models [13].
The germline-targeting strategy exemplified by eOD-GT8 provides a robust foundation for iterative vaccine improvement. As additional clinical data emerge from ongoing trials, the comparative effectiveness of this approach against lineage-based and other strategies will become increasingly clear, potentially heralding a new era in precision vaccinology.
Sequential immunization regimens, often termed "prime-boost" strategies, represent a cornerstone of modern vaccinology, particularly in the fight against complex pathogens. A heterologous prime-boost approach involves administering two different vaccine types or formulations targeting the same pathogen in sequence. This strategy has gained significant traction for its ability to elicit more robust and durable immune responses compared to homologous regimens (using the same vaccine for all doses). The immunological rationale stems from the ability of different vaccine platforms to engage the immune system through distinct mechanisms, thereby overcoming limitations associated with repeated administration of identical vectors or antigens. This guide provides a comprehensive comparison of heterologous prime-boost strategies, examining their performance across various disease targets, with a specific focus on the comparative context of germline-targeting versus lineage-based vaccine strategies.
The fundamental advantage of heterologous regimens lies in their capacity to avert the inhibitory effects of vector-specific immune responses. When the same viral vector is used for multiple vaccinations, immune responses against the vector itself can dampen the response to the target antigen in subsequent doses. By switching vaccine platforms between prime and boost, heterologous strategies circumvent this issue, potentially enhancing both cellular and humoral immunity against the pathogen of interest [25]. Furthermore, introducing new antigens into boost inoculations can be advantageous, demonstrating that the effect of 'original antigenic sin'—where the immune system preferentially recalls responses to the initially encountered strain—is not absolute [25].
Comparative Performance of Vaccine Platforms
Quantitative Comparison of Immune Responses
Table 1: Comparison of Immune Responses in Heterologous vs. Homologous SARS-CoV-2 Vaccination
| Vaccine Regimen | Neutralizing Antibody Titers | CD8+ T Cell Responses | CD4+ T Cell Responses | Mucosal Immunity | Key Findings |
|---|---|---|---|---|---|
| Adenovirus (Prime) + mRNA (Boost) | 6-73-fold increase [26] | Significantly enhanced [26] | Significantly enhanced [26] | Moderate (systemic focus) | Superior neutralizing antibodies and T cell responses against variants [26] |
| mRNA (Prime) + Adenovirus (Boost) | Enhanced compared to homologous | Enhanced compared to homologous | Enhanced compared to homologous | Moderate (systemic focus) | Platform sequence influences immune polarization |
| Adenovirus (Prime) + Protein Subunit (Boost) | Enhanced breadth | Moderate enhancement | Strong CD4+ helper response | Limited | Focus on antibody quality over quantity |
| Homologous mRNA | 4-20-fold increase [26] | Moderate | Strong | Limited | High initial antibody titers but potentially limited breadth |
| Homologous Adenovirus | Lower than heterologous | Moderate | Moderate | Limited | Potentially hampered by anti-vector immunity |
Table 2: HIV-Specific Vaccine Approaches and Outcomes
| Vaccine Strategy | Target | Immune Response | Efficacy/Status | Key Challenges |
|---|---|---|---|---|
| Germline-Targeting (e.g., eOD-GT8 60mer) | Naïve B cells with bnAb potential | Precursor B cell activation: 97% response rate in Phase I [10] | Early clinical trials (IAVI G001) | Requires multiple sequential immunogens to achieve maturity [12] |
| Lineage-Based Design | Evolving B cell lineages | Guided antibody maturation | Preclinical optimization | Complex immunogen design requiring reconstruction of maturation history [10] |
| Adenovirus/Mosaic (Imbokodo, Mosaico) | T cells and non-neutralizing antibodies | CD8+ T cell responses | Efficacy trials completed (HVTN 705/706) | Limited bnAb induction [12] |
| Fusion Peptide Approach | Conserved fusion epitope | Multiple bnAb lineages targeting single epitope | Preclinical/early clinical | Achieving sufficient neutralizing potency [12] |
| Passive bNAb Administration (AMP Trials) | Virus neutralization | Direct virus neutralization | Proof-of-concept: protection at high titers (>1:500) [10] | High antibody titers required for protection |
Mechanisms of Enhanced Immunogenicity
The superior performance of heterologous prime-boost regimens can be attributed to several interconnected immunological mechanisms. Single-cell transcriptomic analysis of injection-site tissues in mouse models has revealed that adenoviral priming establishes a pre-conditioned innate immune environment that is further amplified upon mRNA boosting, particularly through fibroblast-driven chemokine responses that promote immune cell recruitment [26]. This creates a favorable microenvironment for the generation of adaptive immunity.
Additionally, adenovirus-based vaccines may contribute to heterologous efficacy through trained immunity—a memory-like state within the innate immune system where innate cells (particularly monocytes and macrophages) are epigenetically and metabolically reprogrammed to respond more robustly to future challenges [26]. This prolonged activation of monocytes, lasting up to three months post-vaccination, enhances cytokine production and antigen presentation capabilities, thereby priming the immune system for more effective responses to subsequent exposures [26].
The route of administration further modulates efficacy. Recent research demonstrates that mucosal delivery of heterologous boost vaccines can overcome deleterious prime-derived immunological imprinting—a phenomenon where preexisting immunity to an antigen negatively impacts responses to related antigens [27]. Intranasal boosting engages different compartments of the immune system, generating robust mucosal immunity while bypassing the suppressive effects of serum antibodies, resulting in enhanced T and B cell responses in respiratory tissues [27].
Experimental Protocols and Methodologies
Preclinical Evaluation of Heterologous Regimens
Table 3: Key Research Reagents for Prime-Boost Studies
| Research Reagent | Function/Application | Example Use Cases |
|---|---|---|
| ChAdOx1 vectors | Adenoviral vaccine vector | SARS-CoV-2, HIV, cancer vaccine studies [27] [28] |
| mRNA-LNP | Lipid nanoparticle-formulated mRNA | COVID-19 vaccines, HIV immunogen delivery [10] [26] |
| SOSIP trimers | Stabilized envelope trimers | HIV bnAb induction studies [10] |
| TLR7/8 agonists (3M-052) | Vaccine adjuvant | Enhancing antibody responses in protein vaccines [10] |
| eOD-GT8 60mer | Germline-targeting nanoparticle | Priming HIV bnAb precursors [10] [12] |
Protocol 1: Evaluating Heterologous Regimens in Mouse Models
- Immunization: Female BALB/c mice (4-6 weeks old) are immunized intramuscularly in the hind limb. Prime and booster vaccinations are typically administered 3 weeks apart [26].
- Sample Collection: Blood is collected via facial vein puncture under anesthesia. Spleens and lungs are harvested post-euthanasia for cellular analysis. For mucosal immunity assessment, bronchoalveolar lavage (BAL) and nasal-associated lymphoid tissue (NALT) fluid are collected [27].
- Immune Monitoring: Serum antibodies are analyzed by ELISA for antigen-specific IgG, IgA, and IgM. Neutralizing capacity is assessed using pseudovirus neutralization assays or ACE-2 competition assays. T cell responses are evaluated via intracellular cytokine staining or ELISpot after antigen res stimulation [27] [26].
- Single-Cell Analysis: Injection-site tissues are processed for single-cell RNA sequencing 16 hours post-vaccination to characterize innate immune activation and chemokine responses [26].
Clinical Evaluation of Heterologous Regimens
Protocol 2: Clinical Trial Design for Heterologous COVID-19 Vaccines
- Study Population: Healthcare workers or general adult population without prior SARS-CoV-2 infection (confirmed by serological testing) [29].
- Vaccination Groups: Participants are randomized to receive homologous regimens (e.g., ChAdOx1/ChAdOx1) or heterologous regimens (e.g., CoronaVac/ChAdOx1, ChAdOx1/mRNA) with appropriate intervals between doses [29].
- Serological Assessment: Blood samples are collected at predefined intervals (e.g., 2, 4, 12 weeks post-each dose). A multiplex microsphere assay is employed to measure IgG, IgM, and IgA isotypes against various SARS-CoV-2 antigens (Spike trimer, RBD variants, nucleoprotein) [29].
- Data Analysis: Antibody levels are compared across groups. Gaussian Mixture Models (GMMs) can cluster immune responses to differentiate between vaccination types and identify breakthrough infections based on distinct serological profiles [29].
Germline-Targeting vs. Lineage-Based Strategies: A Comparative Framework
The development of HIV vaccines has catalyzed the advancement of two sophisticated immunization strategies: germline-targeting and lineage-based vaccine design. Both approaches represent structured heterologous regimens aimed at solving the unique challenges posed by highly variable pathogens.
Germline-Targeting Approach
Germline targeting employs structure-based design to reverse engineer HIV immunogens that can initiate bnAb development by engaging naïve B cells with bnAb potential [10]. This approach involves a sequential immunization strategy:
The initial prime immunogen is designed to activate rare B cells (approximately 1 in 300,000 naïve B cells) that have the potential to develop into bnAb-producing cells [12]. Successive booster immunogens with increasingly native-like HIV Envelope proteins then shepherd these B cell lineages toward bnAb development through multiple rounds of somatic hypermutation and selection [10]. Clinical trials of the eOD-GT8 60mer immunogen have demonstrated that this initial step is feasible, with 97% of vaccinees showing targeted bnAb precursor responses [10].
Lineage-Based Design
Lineage-based approaches computationally reconstruct the maturation history of a known bnAb from an HIV-infected individual and use this as a blueprint for sequential immunizations [10]. Rather than starting with germline precursors, this strategy aims to recapitulate the natural evolution of bnAbs by presenting a series of immunogens that correspond to sequential stages in the bnAb development pathway.
Comparative Effectiveness
Table 4: Germline-Targeting vs. Lineage-Based Vaccine Strategies
| Parameter | Germline-Targeting Approach | Lineage-Based Approach |
|---|---|---|
| Starting Point | Reverse-engineered immunogens to bind germline B cells [10] | Mature bnAbs from infected individuals [10] |
| Design Basis | Structure-based immunogen engineering [12] | Computational reconstruction of bnAb lineages [10] |
| Immunization Sequence | Predefined path from germline to mature bnAbs [12] | Recapitulation of natural bnAb evolution [10] |
| Clinical Validation | Early-stage clinical trials (IAVI G001) [10] | Preclinical optimization [10] |
| Key Challenge | Engaging extremely rare B cell precursors [12] | Accurately reconstructing evolutionary pathways [10] |
| Advantage | Rational design from first principles | Based on empirically successful bnAb pathways |
Applications Across Disease Targets
SARS-CoV-2 and Respiratory Viruses
For SARS-CoV-2, heterologous prime-boost strategies have demonstrated superior efficacy against variants of concern. Heterologous vaccination (adenoviral prime, mRNA boost) elicits higher neutralizing antibody titers and stronger CD8+ T cell responses against Delta and Omicron variants compared to homologous regimens [26]. This enhanced breadth is particularly valuable for addressing continued viral evolution.
Mucosal delivery of heterologous boosts represents a promising advancement for respiratory viruses. Intranasal administration of omicron vaccine boosters overcame the limitations of immunological imprinting from ancestral strain priming, generating de novo B cell responses in the lungs and recruiting cross-reactive T cells to respiratory tissues [27]. This "prime-pull" strategy enhances protection at the primary site of viral entry, representing a significant improvement over intramuscular vaccination alone.
HIV Vaccine Development
HIV vaccine development has been at the forefront of sophisticated heterologous regimen design. The extraordinary global diversity of HIV and its immune evasion tactics necessitate strategies that can induce broad and potent immune responses [10]. The combination of B cell and T cell vaccine strategies appears particularly promising, with preclinical studies demonstrating that combining an HIV SOSIP protein vaccine that induces autologous neutralizing antibodies with potent T cell-inducing viral vectors provided better protection against SHIV challenge than either candidate alone [10]. Notably, vaccine-mediated induction of potent T cell responses lowered the antibody threshold needed to prevent infection, suggesting important synergies between these arms of immunity [10].
Cancer Immunotherapy
Heterologous prime-boost strategies are also being explored in cancer immunotherapy. A regimen combining a self-assembling peptide nanoparticle TLR-7/8 agonist (SNP) vaccine prime with a chimp adenovirus (ChAdOx1) boost administered intravenously elicited potent CD8+ T cell responses and promoted tumor regression in mouse models [28]. Intravenous administration of the boost generated 4-fold higher antigen-specific CD8+ T cell responses compared to intramuscular boosting and mediated tumor regression through type I IFN-dependent remodeling of the tumor microenvironment [28]. This approach demonstrates how heterologous regimens can be optimized for specific therapeutic applications through route and platform selection.
Heterologous prime-boost vaccination strategies represent a powerful tool in modern vaccinology, offering enhanced immunogenicity and broader protection compared to homologous regimens across multiple disease targets. The comparative analysis presented in this guide demonstrates that the strategic combination of different vaccine platforms can overcome limitations associated with single-platform approaches, including vector-specific immunity, antigenic imprinting, and restricted immune breadth.
The ongoing development of both germline-targeting and lineage-based strategies for HIV vaccination illustrates how heterologous regimens can be rationally designed to address specific immunological challenges. As vaccine science advances, the intentional selection and sequencing of vaccine platforms based on their complementary immunological properties will likely play an increasingly important role in combating complex pathogens, with implications for infectious diseases, cancer immunotherapy, and beyond. The experimental data and methodologies compiled in this guide provide researchers with a framework for evaluating and optimizing sequential immunization regimens for specific applications.
Messenger RNA (mRNA) vaccines represent a fundamental shift in vaccinology, moving from traditional biological-based production to a programmable platform technology that leverages the body's own cellular machinery. Unlike conventional vaccines that require the production of antigens in complex biological systems (e.g., chicken eggs or cell cultures), mRNA vaccines deliver genetic instructions that direct human cells to temporarily produce specific antigenic proteins, thereby eliciting protective immune responses [30] [31]. This core difference in mechanism enables unprecedented speed and flexibility in vaccine development, which was dramatically demonstrated during the COVID-19 pandemic when mRNA vaccines were developed, tested, and authorized in less than a year – a process that traditionally takes 5-10 years [32] [31].
The technological underpinnings of mRNA vaccines were established through decades of research addressing key challenges such as mRNA instability, inefficient delivery, and excessive inflammatory responses [33] [32]. Critical breakthroughs include the incorporation of modified nucleosides to reduce immunogenicity and improve stability, sequence engineering to optimize protein expression, and the development of lipid nanoparticles (LNPs) as efficient delivery vehicles that protect mRNA and facilitate its cellular uptake [30] [33] [32]. These advances have created a versatile platform that can be rapidly adapted to target various pathogens, with current research extending to influenza, respiratory syncytial virus (RSV), human immunodeficiency virus (HIV), and even non-infectious diseases like cancer [30] [33].
This review will objectively compare the performance of mRNA vaccine platforms against traditional alternatives, examining their relative advantages and limitations through published experimental data. Within the broader context of comparative effectiveness between germline-targeting and lineage-based vaccine strategies, the mRNA platform offers unique insights due to its capacity for rapid iteration and its potent activation of both humoral and cellular immunity, potentially informing future vaccine design paradigms.
Comparative Platform Performance: mRNA vs. Traditional Vaccine Technologies
Mechanism of Action and Technological Characteristics
Traditional vaccine platforms, including live-attenuated, inactivated, and subunit vaccines, introduce foreign antigens or whole pathogens to stimulate an immune response. In contrast, mRNA vaccines function as a genetic instruction set, delivering mRNA sequences that encode specific antigenic proteins [31]. The fundamental differences in their mechanisms of action lead to distinct performance characteristics, advantages, and limitations for each platform, as summarized in the table below.
Table 1: Comparative analysis of mRNA versus traditional vaccine platforms
| Feature | mRNA Vaccines | Live-Attenuated Vaccines | Inactivated Vaccines | Subunit/Recombinant Vaccines |
|---|---|---|---|---|
| Mechanism of Action | Cellular production of antigen from delivered mRNA [30] | Weakened pathogen triggers immune response [31] | Killed pathogen triggers immune response [31] | Purified pathogen components trigger immune response [31] |
| Development Timeline | Rapid (weeks for candidate design) [32] | Lengthy (months to years) [32] | Lengthy (months to years) [32] | Lengthy (months to years) [32] |
| Immune Profile | Strong humoral and cellular immunity [30] [33] | Strong, often lifelong immunity [31] | Weaker, may require boosters [31] | Targeted, may require adjuvants [32] |
| Safety Profile | Non-infectious, no risk of reversion, cannot integrate into DNA [33] [31] | Risk of reversion to virulence in immunocompromised [32] | No risk of reversion, may cause stronger injection reactions [31] | High safety, no live components [31] |
| Manufacturing Process | Cell-free, synthetic process [32] | Requires pathogen cultivation in eggs or cells [31] | Requires pathogen cultivation and inactivation [31] | Requires complex protein purification or recombinant systems [32] |
| Stability & Storage | Requires ultra-cold chain ( -20°C to -70°C) [31] | Often stable at refrigerator temperatures [31] | Often stable at refrigerator temperatures [31] | Often stable at refrigerator temperatures [31] |
| Platform Flexibility | High; sequence can be updated for new variants [30] [33] | Low; new strains require new development [31] | Low; new strains require new development [31] | Medium; antigens can be swapped but require new protein development [31] |
Quantitative Performance Data from Clinical Applications
The comparative performance of these platforms is further elucidated by clinical data, particularly from vaccines against COVID-19 and influenza. The table below summarizes key efficacy and response data.
Table 2: Clinical performance data for mRNA versus traditional vaccine platforms
| Vaccine / Platform | Pathogen | Efficacy/Effectiveness | Immune Response Characteristics | Key Clinical Findings |
|---|---|---|---|---|
| Pfizer-BioNTech (BNT162b2) [30] | SARS-CoV-2 | >90% against symptomatic infection [30] | Robust neutralizing antibodies and CD4+ & CD8+ T-cell responses [30] | High efficacy maintained across diverse populations; real-world effectiveness against severe disease |
| Moderna (mRNA-1273) [30] | SARS-CoV-2 | >90% against symptomatic infection [30] | Robust neutralizing antibodies and CD4+ & CD8+ T-cell responses [30] | Similar high efficacy profile; strong durability of immune response |
| Conventional Inactivated Influenza Vaccine [31] | Influenza | 40-60% seasonal effectiveness [31] | Primarily antibody-mediated, strain-specific | Lower efficacy due to antigenic drift and egg-adaptation changes |
| Moderna's mRNA-1010 (Investigational) [33] | Influenza | Phase III trials ongoing [33] | Higher hemagglutination inhibition (HAI) titers vs. licensed comparator [33] | Designed for better match to circulating strains without egg-adaptation |
| mRNA-1083 (Combined COVID-19/Influenza) [34] | SARS-CoV-2 & Influenza | Phase I/II shows strong immune response to both [34] | Superior immune responses versus co-administered standalone vaccines [34] | Demonstrates potential for multivalent, combination vaccines |
Experimental Evidence: Elucidating the mRNA Vaccine Mechanism
Key Methodologies in mRNA Vaccine Research
Research into mRNA vaccine technology relies on specific experimental protocols to evaluate the stability, delivery, immunogenicity, and efficacy of vaccine candidates. Key methodologies include:
In Vitro Transcription (IVT) and mRNA Modification: Synthetic mRNA is produced using phage RNA polymerases (e.g., T7) in a cell-free system to transcribe a linear DNA template containing the target sequence. This mRNA is then modified with a 5′ cap structure (e.g., using CleanCap technology for Cap 1 formation) and a 3′ poly(A) tail, and incorporates modified nucleosides (e.g., pseudouridine) to enhance stability and reduce innate immune recognition [32]. Purification steps (e.g., HPLC) remove double-stranded RNA contaminants that can trigger excessive interferon responses [32].
Lipid Nanoparticle (LNP) Formulation and Characterization: mRNA is encapsulated in LNPs via rapid mixing of an aqueous mRNA solution with an ethanol solution containing ionizable lipids, phospholipids, cholesterol, and PEG-lipids using microfluidic devices [33] [32]. The resulting particles are characterized for size (typically 80-100 nm), polydispersity, encapsulation efficiency, and stability. In vivo biodistribution studies using radiolabeled or fluorescently tagged LNPs are conducted to evaluate tissue targeting and delivery efficiency [33].
Immunogenicity and Efficacy Assessment in Preclinical Models: Animal models (e.g., mice, ferrets, non-human primates) are immunized with the mRNA-LNP candidate. Serum is regularly collected to measure antigen-specific antibody titers (e.g., by ELISA and neutralization assays). Cellular immune responses are quantified by intracellular cytokine staining (ICS) and ELISpot to detect antigen-specific T-cells. Challenge studies involve exposing immunized animals to the live pathogen to evaluate protective efficacy based on viral load reduction and prevention of clinical disease [33].
Evaluation of Innate Immune Activation: The magnitude and type of innate immune response are critical. This is assessed by measuring cytokine and chemokine levels (e.g., IFN-α, IL-6) in serum after vaccination. The maturation status of antigen-presenting cells (e.g., dendritic cells) in lymphoid tissues is analyzed by flow cytometry for surface activation markers (e.g., CD80, CD86, MHC-II) [35].
Case Study: mRNA Vaccines as Immune Modulators for Cancer Therapy
A compelling example of the unique immune-activating properties of mRNA platforms comes from recent investigations into their off-target anti-cancer effects. A pivotal 2025 study published in Nature analyzed over 1,000 cancer patients and found that those who received an mRNA COVID-19 vaccine within 100 days of starting immunotherapy (immune checkpoint inhibitors) had significantly improved survival [36] [35] [37].
- Experimental Workflow and Key Findings:
- Retrospective Cohort Analysis: Researchers analyzed records of 180 advanced non-small cell lung cancer (NSCLC) patients who received an mRNA COVID-19 vaccine within 100 days of immunotherapy and 704 who did not. The vaccinated group showed a near-doubling of median survival (37.33 months vs. 20.6 months) and a significantly improved 3-year overall survival rate (55.7% vs. 30.8%) [36] [35].
- Preclinical Mechanistic Studies: In mouse models, SARS-CoV-2 mRNA vaccines triggered a substantial surge in type I interferon (IFN). This "resets" the immune system by enhancing the ability of antigen-presenting cells in lymphoid organs to prime CD8+ T cells against tumor-associated antigens [35] [37].
- Impact on Tumor Microenvironment: The innate immune activation caused by the mRNA vaccine led tumor cells to upregulate the immune checkpoint protein PD-L1 as a defense mechanism. This created a vulnerability that could be effectively targeted by anti-PD-L1/PD-1 immunotherapy, turning "cold" immunologically silent tumors into "hot", responsive ones [36] [35]. Patients with these typically treatment-resistant "cold" tumors experienced a nearly five-fold improvement in three-year overall survival after receiving the vaccine [36].
This study underscores that the immunostimulatory power of mRNA vaccines extends beyond the antigen they encode. The platform itself acts as a potent immune modulator, a property that is now being formally tested in a randomized Phase III trial to determine if mRNA vaccines should be part of standard care for patients receiving immunotherapy [36].
Diagram Title: mRNA Vaccine Synergy with Cancer Immunotherapy
The Scientist's Toolkit: Essential Reagents for mRNA Vaccine Research
The development and evaluation of mRNA vaccines depend on a specialized set of reagents and materials. The following table details key components of the research toolkit for scientists working in this field.
Table 3: Essential research reagents and materials for mRNA vaccine development
| Research Reagent / Material | Function and Role in Development |
|---|---|
| Linear DNA Template | Contains phage polymerase promoter (e.g., T7), 5' and 3' UTRs, the antigen open reading frame (ORF), and a poly(A) tract. Serves as the template for in vitro transcription [32]. |
| Modified Nucleotides | (e.g., N1-methylpseudouridine). Incorporated during IVT to decrease innate immune sensing by pattern recognition receptors (PRRs) and enhance mRNA translation efficiency [32]. |
| CleanCap AG Cap 1 Analog | A trinucleotide cap analog (m7GpppAG) used in co-transcriptional capping. Produces a higher yield of properly capped mRNA (Cap 1 structure) than older methods, improving translation and reducing immunogenicity [32]. |
| Ionizable Lipids | (e.g., DLin-MC3-DMA, SM-102). The key functional component of LNPs, enabling efficient encapsulation of mRNA and endosomal escape upon cellular uptake. Their positive charge at acidic pH facilitates release of mRNA into the cytoplasm [33] [32]. |
| Lipid Nanoparticles (LNPs) | A multi-component delivery system comprising ionizable lipid, phospholipid, cholesterol, and PEG-lipid. Protects mRNA from degradation and mediates cellular delivery and endosomal escape [30] [33] [32]. |
| Human Cell Lines | (e.g., HEK-293). Used for in vitro transfection experiments to test mRNA expression, protein production, and immunogenicity before moving to animal models [33]. |
| ELISA Kits | Used to quantify antigen-specific antibody titers (IgG, IgM) in immunized animal or human serum, measuring the humoral immune response [33]. |
| ELISpot Kits | Used to enumerate antigen-specific T-cells (IFN-γ ELISpot for CD8+ T-cells) from peripheral blood mononuclear cells (PBMCs), quantifying the cellular immune response [33]. |
The advent of mRNA technology has unequivocally established a new paradigm for vaccine development, characterized by unprecedented speed, flexibility, and the ability to elicit robust cellular and humoral immunity. Quantitative data from both infectious disease and oncology contexts demonstrate that the platform's impact may extend beyond its initial target indications, potentially enabling new therapeutic strategies. While challenges related to stability, delivery, and long-term safety persist, ongoing research into improved nucleotide chemistries, delivery systems, and manufacturing processes continues to address these limitations. As the field matures, the programmable nature of mRNA vaccines positions them as a powerful tool not only for responding to emerging pathogens but also for developing sophisticated therapeutic interventions for a broad spectrum of diseases, thereby reshaping the future of both preventive and therapeutic medicine.
The rapid evolution of viruses presents a formidable challenge in vaccine development, necessitating distinct strategic approaches to maintain vaccine effectiveness. Germline-targeting strategies aim to guide the immune system through a series of precisely engineered immunogens to elicit broad, neutralizing antibodies against highly variable pathogens. In contrast, lineage-based strategies rely on continuous surveillance of circulating viral strains to periodically update vaccine formulations to match predominant lineages. The comparative effectiveness of these paradigms is a central focus of modern immunology and virology research. This guide objectively compares their application, performance, and supporting experimental data, providing researchers with a framework for strategic decision-making in vaccine design.
The following sections will dissect the surveillance mechanisms, strain selection processes, and experimental protocols that underpin these strategies, with data drawn from current practices for influenza, SARS-CoV-2, and HIV-1.
Lineage-Based Vaccine Strategy in Practice
The lineage-based approach, exemplified by seasonal influenza and COVID-19 vaccines, relies on a global surveillance and response system to track viral evolution and update vaccine antigens accordingly.
Surveillance and Strain Selection Workflow
The process for determining viral lineages for vaccine updates is a continuous, global effort coordinated by public health agencies. The logical workflow for this system is depicted in the diagram below.
Global Surveillance and Strain Selection Workflow
The foundational step involves continuous global surveillance to collect circulating virus samples from patients worldwide [38]. National and international laboratories then perform genetic sequencing and antigenic characterization to identify emerging variants and assess their potential impact on public health [39] [38]. This data is compiled and analyzed by expert committees at organizations like the World Health Organization (WHO) and the U.S. Food and Drug Administration (FDA). These committees convene at predetermined times—typically twice yearly for influenza—to recommend specific virus strains for inclusion in seasonal vaccines [39] [40] [38]. This recommendation triggers manufacturers to begin production of updated vaccine formulations, a process that can take several months depending on the platform used (e.g., egg-based, cell-based, or mRNA) [41].
Current Formulations and Supporting Data
For the 2025-2026 season, regulatory agencies have recommended specific vaccine compositions based on this lineage-selection process. The quantitative details of these formulations are summarized in the table below.
Table 1: 2025-2026 Season Vaccine Strain Compositions
| Vaccine Type | Virus Strains Included | Target Lineages | Regulatory Authority |
|---|---|---|---|
| Influenza (Egg-based) | A/Victoria/4897/2022 (H1N1)pdm09-like virusA/Croatia/10136RV/2023 (H3N2)-like virusB/Austria/1359417/2021 (B/Victoria lineage)-like virus | H1N1, H3N2, B/Victoria | U.S. FDA [39] |
| Influenza (Cell/Recombinant) | A/Wisconsin/67/2022 (H1N1)pdm09-like virusA/District of Columbia/27/2023 (H3N2)-like virusB/Austria/1359417/2021 (B/Victoria lineage)-like virus | H1N1, H3N2, B/Victoria | U.S. FDA [39] [42] |
| COVID-19 (2025-2026 Formula) | Monovalent JN.1-lineage (preferentially LP.8.1 strain) | JN.1 SARS-CoV-2 lineage | U.S. FDA [40] |
The lineage-based approach, while essential for rapidly evolving viruses, faces the inherent challenge of antigenic mismatch, where the vaccine strain may not perfectly match the dominant circulating strain by the time the vaccine is deployed. For instance, for the 2025-2026 flu season, an H3N2 variant termed "subclade K" emerged after the vaccine strain selection was finalized [43] [44]. This real-world example underscores a critical limitation of the lineage approach: its effectiveness is contingent on accurate prediction of future viral dominance.
Germline-Targeting Vaccine Strategy
In contrast to the reactive nature of lineage-based approaches, germline-targeting represents a proactive strategy designed to overcome the challenges posed by viruses with extreme genetic diversity, most notably HIV-1.
Strategic Framework and Rationale
Germline-targeting is a multi-step immunization strategy aimed at eliciting broadly neutralizing antibodies (bNAbs). The core challenge it addresses is that the precursor B cells capable of developing into bNAb-producers are exceedingly rare in the human body [45]. Furthermore, bNAbs themselves require extensive maturation through a process called somatic hypermutation (SHM) to acquire the breadth needed to neutralize diverse viral strains [45]. The germline-targeting strategy uses a series of specifically engineered immunogens to first "recruit" these rare precursor B cells and then guide them through the necessary maturation steps. This approach is particularly critical for HIV-1, where the envelope (Env) glycoprotein is shielded by a dense "glycan shield" and exhibits extraordinary genetic diversity, making a conventional lineage-based vaccine ineffective [45].
Experimental Models and Research Tools
Research into germline-targeting vaccines relies on sophisticated animal models and reagent solutions to study B cell recruitment and antibody maturation pathways. The experimental workflow is complex and multi-staged.
Germline-Targeting Experimental Workflow
Key research reagents are essential for executing this workflow. The table below details critical tools used in this field.
Table 2: Key Research Reagent Solutions for Germline-Targeting
| Research Reagent | Function in Experimentation | Application Context |
|---|---|---|
| Engineered Immunogens (e.g., eOD-GT8, BG505 SOSIP) | Designed to bind and activate specific precursor B cells; serve as prime and boost immunogens. | Preclinical studies in knock-in mouse models and non-human primates [45]. |
| Knock-in Mouse Models (e.g., VRC01-class, 3BNC60-class) | Engineered to express human B cell receptors; model human immune responses. | Testing immunogen ability to recruit and expand desired precursor B cell lineages [45]. |
| Adeno-associated Virus (AAV) Vectors | Deliver immunogens or bNAb genes for in vivo expression; used in "vectored immunoprophylaxis". | Preclinical delivery of bNAbs and immunogens in animal models [45]. |
| Pseudotype-Based Neutralization Assays | Measure the breadth and potency of antibody responses against a panel of heterologous viruses. | Assessing the functional outcome of immunization in preclinical and clinical studies [45]. |
The primary quantitative outcome measured in these experiments is the breadth of neutralization, typically reported as the percentage of a diverse viral panel that is neutralized by serum from immunized animals. While lineage-based vaccines for influenza and COVID-19 achieve effectiveness by matching circulating strains, the goal of a germline-targeting HIV-1 vaccine is to achieve a high level of breadth—often targeting over 30-50% of a global virus panel—without being tied to specific, transient lineages [45].
Comparative Analysis of Strategic Performance
Directly comparing the effectiveness of these strategies is complex, as they are applied to different viral pathogens with distinct challenges. However, an analysis of their performance outcomes and logistical requirements provides critical insights for vaccine developers.
Quantitative Effectiveness and Limitations
Table 3: Strategic Comparison Based on Published Data
| Performance Metric | Lineage-Based Strategy | Germline-Targeting Strategy |
|---|---|---|
| Reported Efficacy/Effectiveness | Flu VE: 19-60% (US, 2010-2023) [41]COVID-19: Prevents severe illness [46] | ~30% efficacy (RV144 HIV trial) [45] |
| Primary Limitation | Antigenic mismatch (e.g., H3N2 subclade K) [43] [44] | Inability to consistently elicit bNAbs [45] |
| Key Strength | Rapid deployment of updated, matched formulations | Aims for broad, variant-proof protection |
| Production Timeline | 6-8 months (egg-based influenza vaccines) [41] | N/A (Still in preclinical/early clinical stages) |
The data reveals a fundamental trade-off. Lineage-based vaccines are deployable and provide measurable public health benefit, but their effectiveness is variable and can be compromised by viral evolution. The germline-targeting approach for HIV aims for a universal solution but has not yet achieved high efficacy in clinical trials, with the most successful trial (RV144) showing only 31.2% efficacy [45].
Experimental Protocols for Critical Assays
The evaluation of both strategies relies on robust and standardized experimental protocols. Below are detailed methodologies for two key assays used in lineage-based vaccine evaluation.
Hemagglutination Inhibition (HI) Assay for Influenza Vaccine Match
- Purpose: To quantify the antigenic similarity between influenza vaccine strains and circulating viruses, informing strain selection and estimating potential vaccine effectiveness [41].
- Procedure:
- Serum Collection: Obtain post-vaccination ferret antisera raised against the candidate vaccine virus.
- Virus Preparation: Standardize circulating virus isolates to a specific concentration of hemagglutinating units.
- Serum-Virus Incubation: Serially dilute the antisera and mix with the virus isolates. Include control wells.
- Red Blood Cell (RBC) Addition: Add a suspension of turkey or guinea pig RBCs to each well.
- Inhibition Reading: Incubate and then assess for hemagglutination. The HI titer is the highest serum dilution that completely inhibits hemagglutination. A ≥4-fold reduction in titer between a vaccine strain and circulating virus is often considered antigenically distinct [41].
Vaccine Effectiveness (VE) Study using Test-Negative Design
- Purpose: To measure the real-world effectiveness of a vaccine in preventing sought-out medical care for laboratory-confirmed illness [43].
- Procedure:
- Subject Recruitment: Enroll individuals who seek medical care for an acute respiratory illness.
- Data Collection: Record vaccination status and relevant covariates (e.g., age, underlying conditions, time since vaccination).
- Laboratory Testing: Test all subjects for the virus of interest (e.g., influenza or SARS-CoV-2) using PCR.
- Case-Control Classification: Classify subjects as "cases" (test-positive) or "controls" (test-negative).
- Odds Ratio Calculation: Calculate the odds ratio (OR) of vaccination among cases compared to controls. VE is then calculated as (1 - OR) × 100% [43].
The choice between germline-targeting and lineage-based vaccine strategies is not merely binary but is dictated by the biological characteristics of the pathogen and the public health objective. The lineage-based approach is a proven, pragmatic solution for managing viruses like influenza and SARS-CoV-2 that evolve in a relatively predictable, sequential manner. However, its susceptibility to antigenic mismatch and the associated manufacturing lag are significant drawbacks. Research is actively focused on improving surveillance predictive models and adopting faster vaccine platforms (e.g., mRNA, recombinant) that allow for later strain selection decisions, potentially improving the vaccine match [41].
Conversely, the germline-targeting strategy represents a pioneering, long-term solution for viruses like HIV-1 that have so far eluded conventional vaccine approaches due to their extreme diversity and structural defenses. While clinical success has been modest, advancements in immunogen design, mRNA delivery, and a deeper understanding of B cell biology are steadily progressing toward the goal of elicting potent bNAbs [45].
For researchers and drug development professionals, the future lies in the convergence of these strategies. The lessons learned from the precise engineering of germline-targeting immunogens could inform the design of broader, more durable influenza and coronavirus vaccines. Meanwhile, the robust surveillance and rapid manufacturing systems built for lineage-based vaccines provide a deployment framework for which future universal vaccines can be integrated. The continued comparative evaluation of these paradigms is therefore not just an academic exercise, but a critical driver of innovation in global public health.
This guide provides a comparative analysis of two advanced vaccine development strategies deployed against different viral threats: the germline-targeting approach for a preventive HIV vaccine and the lineage-based strategy used for the updated 2024-2025 COVID-19 vaccine. The IAVI G002 and G003 trials represent a foundational step in a multi-step, rational vaccine design aimed at eliclying broadly neutralizing antibodies (bnAbs) against the highly variable HIV virus. [2] [47] In contrast, the 2024-2025 COVID-19 vaccine exemplifies the rapid application of a lineage-based strategy, where vaccines are updated to match currently circulating SARS-CoV-2 variants, specifically targeting the Omicron JN.1 and KP.2 lineages. [48] This comparison explores the distinct methodologies, trial outcomes, and effectiveness data underpinning these two paradigms in modern vaccinology.
HIV Vaccine Development: IAVI G002 & G003 Trials
Experimental Protocol & Methodology
The IAVI G002 (North America) and IAVI G003 (South Africa and Rwanda) trials were Phase 1 clinical trials designed to test the initial stages of a germline-targeting HIV vaccine strategy. [2]
- Study Population: G002 enrolled 60 participants, and G003 enrolled 18 participants. [2]
- Vaccine Platform: The immunogens were delivered using messenger RNA (mRNA) technology. [2]
- Immunogen Design: The approach used a sequential immunization strategy.
- Priming Immunogen: eOD-GT8 60mer, designed to activate rare naïve B cells with the potential to develop into bnAb-producing cells. This is the first step in "germline targeting." [2] [47]
- Heterologous Booster Immunogen: A distinct booster (Core-g28-v2 60mer in G002) was designed to further guide the primed B cells toward maturation. [2] [47]
- Key Workflow: The G002 trial tested the prime-boost sequence, while G003 tested the priming immunogen alone in an African population to ensure relevance in a high-HIV-burden region. [2]
The conceptual workflow of this germline-targeting strategy is illustrated in the diagram below.
Key Immunological & Safety Outcomes
The trials successfully demonstrated proof-of-concept for the germline-targeting approach.
Table 1: Key Outcomes from IAVI G002 and G003 Trials
| Trial | Population | Intervention | Immune Response | Key Result | Safety Profile |
|---|---|---|---|---|---|
| IAVI G002 [2] | North American (n=60) | Prime + Heterologous Boost | VRC01-class bnAb precursors | 100% (17/17) of boosted participants developed VRC01-class responses; >80% showed "elite" responses with multiple helpful mutations. [2] | Skin reactions (e.g., itching, hives) in 18% of participants; 10% developed chronic urticaria (all resolved). [2] |
| IAVI G003 [2] | South Africa & Rwanda (n=18) | Prime only | VRC01-class bnAb precursors | 94% of participants generated the desired VRC01-class response, confirming relevance in key populations. [2] | Mild, short-lived itching in 11% of participants; no cases of urticaria. [2] |
COVID-19 Vaccine: The 2024-2025 Formula
Vaccine Design & Real-World Effectiveness Protocol
The 2024-2025 COVID-19 vaccine formula was updated to a monovalent design targeting the Omicron JN.1 lineage and its derivatives (like KP.2) to address viral evolution and waning immunity. [48]
- Vaccine Platform: mRNA (Moderna, Pfizer-BioNTech) and a protein subunit option (Novavax). [48]
- Study Design: Real-world vaccine effectiveness (VE) studies using a test-negative design. [48]
- Data Sources: Analyses were conducted through two CDC-funded networks, VISION and IVY, which collect data from hundreds of emergency departments/urgent care centers and hospitals across the United States. [48]
- Methodology: Researchers compared the odds of prior vaccination between case-patients (test-positive for SARS-CoV-2) and control-patients (test-negative) to estimate VE against medically attended illness. [48]
The following diagram outlines the general workflow for assessing the effectiveness of a lineage-based vaccine.
Interim Effectiveness Estimates
Interim data from September 2024 through January 2025 demonstrates the added protection offered by the updated vaccine.
Table 2: Interim Vaccine Effectiveness of the 2024-2025 COVID-19 Formula (CDC) [48]
| Outcome | Study Population | Days Post-Vaccination | Vaccine Effectiveness (VE) | 95% Confidence Interval |
|---|---|---|---|---|
| ED/UC Visit | Adults ≥18 years | 7-119 days | 33% | 28% – 38% |
| Hospitalization | Immunocompetent Adults ≥65 years | 7-119 days | 45% - 46% | 36% – 53% / 26% – 60% |
| Hospitalization | Adults ≥65 years with Immunocompromising Conditions | 7-119 days | 40% | 21% – 54% |
Direct Comparison: Germline-Targeting vs. Lineage-Based Strategies
The following table provides a side-by-side comparison of the two vaccine strategies based on the available data.
Table 3: Strategic Comparison of HIV Germline-Targeting and COVID-19 Lineage-Based Vaccines
| Aspect | HIV Germline-Targeting (IAVI G002/G003) | COVID-19 Lineage-Based (2024-2025 Formula) |
|---|---|---|
| Core Objective | Elicit broadly neutralizing antibodies (bnAbs) against a highly variable virus. [2] [47] | Generate a strain-specific response against currently dominant variants. [48] |
| Development Strategy | Rational design of a multi-step immunization series to "coach" the immune system. [2] [12] | Periodic updates based on surveillance of circulating viral lineages. [48] |
| Key Metric | Activation and maturation of target precursor B cells and bnAb pathways. [2] | Vaccine Effectiveness (VE) against clinical endpoints (infection, severe disease). [48] |
| Stage of Development | Proof-of-concept (Phase 1) for the initial steps of the immunization pathway. [2] | Deployed public health intervention with ongoing effectiveness monitoring. [48] |
| Challenge Addressed | Overcoming HIV's extreme antigenic diversity and poor innate immunogenicity. [47] | Addressing SARS-CoV-2's ongoing antigenic drift and immune escape. [48] |
The Scientist's Toolkit: Essential Research Reagents
The following reagents and tools are critical for advancing research in both germline-targeting and lineage-based vaccine development.
Table 4: Key Research Reagent Solutions for Vaccine Development
| Research Reagent / Tool | Function in Vaccine Research | Application in Featured Studies |
|---|---|---|
| Engineered Immunogens (e.g., eOD-GT8 60mer, Core-g28-v2 60mer) | Precisely designed protein antigens to bind and activate specific naïve or precursor B cells. [2] [12] | Used as prime and boost vaccines to initiate and guide bnAb development in IAVI trials. [2] [47] |
| mRNA Vaccine Platform | A versatile delivery system for encoding antigenic proteins, enabling rapid manufacturing and potent immune responses. [2] | Platform for delivering HIV immunogens in IAVI G002/G003; primary platform for COVID-19 vaccines. [2] [48] |
| State Immunization Information Systems (IIS) | Centralized electronic registries that record vaccine administration data from providers. [48] | Critical data source for accurate vaccination status ascertainment in real-world COVID-19 VE studies. [48] |
| Pseudovirus Neutralization Assay | A high-throughput, safe method to measure the potency and breadth of neutralizing antibodies against viral entry proteins. | Used to characterize antibody responses in HIV vaccine research (e.g., VRC01-class responses). [2] [49] |
| Spike Gene Target Failure (SGTF) | A proxy in certain RT-PCR tests for presumptive identification of specific SARS-CoV-2 variants (e.g., Omicron BA.5). [50] | Used for rapid lineage classification in surveillance and VE studies before WGS confirmation. [50] |
The data from the IAVI G002/G003 trials and the 2024-2025 COVID-19 vaccine program highlight the tailored application of different vaccine strategies. The HIV vaccine work represents a long-term, pioneering investment in germline-targeting, demonstrating that the immune system can be guided along a predefined path to generate sophisticated bnAbs. In contrast, the COVID-19 vaccine program showcases the successful public health implementation of a nimble, lineage-based strategy to mitigate an ongoing pandemic, providing measurable protection against severe outcomes. Both approaches are at the forefront of vaccinology, addressing the distinct challenges posed by two complex viruses.
Navigating Challenges and Optimizing Immune Responses
Overcoming B Cell Rarity and Guiding Affinity Maturation
The development of effective vaccines against rapidly mutating pathogens like HIV and influenza represents a monumental challenge in modern immunology. A central hurdle is the need to engage rare B cells capable of producing broadly neutralizing antibodies (bnAbs) and then precisely guide their maturation through complex evolutionary pathways. To address this, two sophisticated vaccine strategies have emerged: germline-targeting and mutation-guided lineage-based approaches. Both aim to overcome the biological constraints that naturally limit the production of bnAbs, yet they employ distinct philosophies and technical methodologies. This guide provides a comparative analysis of these pioneering strategies, examining their underlying principles, experimental support, and practical implementation to inform researchers and drug development professionals.
Comparative Analysis of Vaccine Strategies
The table below summarizes the core characteristics, advantages, and challenges of the two main strategies for eliciting broadly neutralizing antibodies.
Table 1: Comparison of Germline-Targeting and Lineage-Based Vaccine Strategies
| Feature | Germline-Targeting Strategy | Mutation-Guided Lineage-Based Strategy |
|---|---|---|
| Core Principle | Reverse engineering of immunogens to activate rare naive B cell precursors; uses a sequence of distinct immunogens to "shepherd" maturation [14] [12]. | Computational reconstruction of the natural maturation history of a known bnAb; immunogens are designed to select for key improbable mutations required for breadth [1]. |
| Target B Cell State | Naive B cells with B cell receptors (BCRs) possessing inherent bnAb potential [14] [1]. | The evolving B cell lineage at multiple stages of its affinity maturation pathway [8] [1]. |
| Immunogen Design | A series of engineered immunogens, each optimized for a specific stage:• Primer: Binds naive BCRs.• Booster(s): Binds intermediate BCRs.• Polisher: Finalizes bnAb maturation [14]. | Immunogens derived from computationally inferred intermediate ancestors within a bnAb clonal lineage to promote specific, critical mutations [8] [1]. |
| Key Advantage | Demonstrates high response rates in initial human trials for priming desired precursors (e.g., 97% in IAVI G001) [1]. | Aims to accelerate the affinity maturation process by focusing on the most critical mutations, potentially shortening the timeline to develop breadth [1]. |
| Main Challenge | Requires the rational design and sequential administration of multiple, highly specific immunogens to guide B cells along a predefined path [14] [12]. | Relies on deep knowledge of the bnAb lineage and may require different immunogen series for different bnAb classes or individuals [8]. |
Experimental Protocols and Workflows
To empirically evaluate and implement these strategies, researchers rely on sophisticated experimental workflows. The following diagrams and protocols detail the key methodologies.
Germline-Targeting Sequential Immunization
This protocol tests the ability of a predefined series of immunogens to prime and mature bnAb precursors in vivo.
Diagram 1: Sequential Immunization Workflow. This flow depicts the stepwise administration of different immunogens to guide B cell maturation from the naive state to bnAb-producing plasma cells. Key immunogens from clinical trials include the eOD-GT8 60mer primer and the core-g28v2 60mer booster [14] [1].
- Key Experimental Model: Humanized mouse models and non-human primates (e.g., rhesus macaques), followed by Phase I human clinical trials (e.g., IAVI G001, G002) [14] [51] [1].
- Priming Phase: Administer germline-targeting immunogen (e.g., eOD-GT8 60mer) with an adjuvant (e.g., saponin/MPLA nanoparticles) via intramuscular injection [14] [51]. Analyze blood and lymph nodes post-immunization using flow cytometry and B cell receptor sequencing to confirm the activation and expansion of desired precursor B cells [1].
- Boosting & Polishing Phase: Administer booster immunogens (e.g., core-g28v2 60mer, BG505 SOSIP GT1.1) at intervals of several weeks to months [14] [1]. The serum is analyzed for antibody binding (via ELISA or BLI) and neutralization breadth (in vitro against a panel of heterologous HIV pseudoviruses). Monoclonal antibodies are isolated from memory B cells or plasma cells to characterize SHM and epitope specificity using cryo-electron microscopy [1].
B Cell Immortalization and Directed Evolution
This protocol allows for the ex vivo discovery and optimization of cross-reactive antibodies, bypassing some of the complexity of in vivo guidance.
Diagram 2: B Cell Immortalization and Directed Evolution. This workflow illustrates the process of creating renewable libraries of human B cells and using directed evolution to enhance antibody properties against viral escape variants [52].
- Key Experimental Model: Primary human B cells isolated from peripheral blood mononuclear cells (PBMCs) or tonsil tissue of convalescent donors or vaccine recipients [52].
- B Cell Immortalization: Isolate B cells via FACS or immunomagnetic beads. Activate cells on hCD40L-expressing L-cells with IL-21. Transduce activated B cells using retroviral vectors encoding apoptosis inhibitors Bcl6 and Bcl-xL to achieve immortalization, yielding transduction efficiencies of ~50-70% [52].
- Library Screening & Directed Evolution: Culture immortalized B cells in small pools. Screen ~40,000 cells per library via high-throughput assays (e.g., neutralization assays against a panel of viral variants) to identify cross-reactive clones [52]. For affinity maturation, subject selected clones to ex vivo AID-induced SHM. Subsequently, screen the resulting libraries for clones with improved binding affinity and neutralization potency against escape variants (e.g., SARS-CoV-2 variants EG.5.1 and JN.1) [52].
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of these strategies depends on specialized reagents and tools. The following table catalogues essential materials for this field of research.
Table 2: Key Research Reagents for B Cell-Focused Vaccine Development
| Research Reagent | Function and Application |
|---|---|
| Engineered Immunogens(e.g., eOD-GT8 60mer, N332-GT5, BG505 SOSIP GT1.1) | Artificially designed protein nanoparticles or trimers used to bind and activate specific naive or intermediate B cells. Critical for both germline-targeting and lineage-based strategies [14] [51] [1]. |
| Adjuvants(e.g., Saponin/MPLA nanoparticles, 3M-052-AF/Alum) | Enhance the immune response to co-administered immunogens, promoting stronger germinal center reactions and B cell maturation [51] [1]. |
| mRNA Vaccine Platform(e.g., mRNA-1644) | Enables in vivo expression of the designed immunogen after immunization. Offers potential for rapid development and improved immunogenicity, as seen in the IAVI G002 trial [14] [1]. |
| Bcl6/Bcl-xL Retroviral Vector | A tool for immortalizing primary human B cells, allowing the creation of stable, renewable libraries that retain antibody secretion capability for functional screening [52]. |
| Biolayer Interferometry (BLI) | A label-free optical technique for measuring the kinetics of antibody-antigen binding (kon, koff, KD). Used to characterize the affinity of vaccine-induced antibodies and bnAbs [1]. |
Discussion and Data Interpretation
The comparative data reveals that both strategies are progressing from concept to clinical reality. The germline-targeting approach has demonstrated remarkable success in the initial priming step. The IAVI G001 trial showed a 97% response rate (35/36 participants) in activating the desired VRC01-class B cell precursors after two immunizations with the eOD-GT8 60mer protein [1]. Subsequent trials (IAVI G002/G003) using an mRNA platform for delivery reported that the primed B cells accumulated even greater levels of somatic hypermutation, a key indicator of maturation [1].
For the lineage-based approach, research highlights the critical importance of specific "improbable" mutations. Studies indicate that broadly neutralizing antibodies (bnAbs) typically possess a high degree of somatic hypermutation (~15%), compared to ~7% for non-neutralizing antibodies, underscoring the extensive maturation required [8]. The ability to immortalize B cell libraries has provided a powerful tool for this strategy, with one study achieving 67.5% transduction efficiency for PBMCs, enabling the functional screening of tens of thousands of clones to find cross-reactive neutralizers [52].
A significant challenge observed across both approaches is the issue of viral escape. The Antibody Mediated Prevention (AMP) trials demonstrated that a single bnAb (VRC01) was insufficient for reliable protection, indicating that a successful vaccine will likely need to elicit antibodies targeting at least three different conserved epitopes on the HIV envelope [1]. This underscores the necessity for combination strategies. Furthermore, safety considerations are paramount; one germline-targeting trial (HVTN 133) targeting the MPER epitope was halted due to an anaphylactic reaction to the PEG component in the vaccine formulation, highlighting the need for careful excipient selection [14].
The quest to overcome B cell rarity and guide affinity maturation sits at the frontier of vaccinology. Germline-targeting and lineage-based strategies offer complementary, sophisticated blueprints for achieving this goal. Germline-targeting has shown early, impressive success in priming desired responses in humans, while lineage-based approaches and new tools like B cell immortalization provide a deeper mechanistic understanding and a platform for rapid antibody optimization. The prevailing evidence suggests that a globally effective vaccine against complex pathogens will not rely on a single strategy but will intelligently combine elements of both to elicit a robust and diverse arsenal of broadly neutralizing antibodies. For researchers, the ongoing challenge lies in refining these protocols, developing better predictive models, and designing immunogens that can more efficiently shepherd the immune response toward broad and potent neutralization.
The development of vaccines against rapidly mutating pathogens, such as human immunodeficiency virus (HIV) and influenza, necessitates innovative strategies to induce broad and potent immunity. Two leading approaches—germline-targeting and lineage-based vaccine design—aim to guide the immune system toward generating broadly neutralizing antibodies (bnAbs) but present distinct challenges regarding immune reactions and tolerability. Germline-targeting involves engineering immunogens that specifically activate rare, naive B cells with the potential to develop into bnAb-producing lineages [53] [54]. In contrast, lineage-based vaccine design typically uses a series of native-like immunogens that mirror the evolutionary path of bnAb development observed in natural infection, aiming to guide pre-engaged B cell receptors through the necessary maturation steps [19] [53]. A critical consideration for both strategies is the unique nature of bnAbs themselves, which often possess unusual biochemical properties—such as long heavy-chain complementarity-determining region 3 (HCDR3) loops, polyreactivity, or autoreactivity—that can trigger immune tolerance mechanisms and potentially lead to undesired immune reactions [19] [55]. This analysis compares the safety and tolerability profiles of these approaches through experimental case studies, focusing on their capacity to elicit targeted responses while minimizing potential adverse immunological outcomes.
Comparative Framework: Germline-Targeting vs. Lineage-Based Strategies
Table 1: Strategic Comparison of Vaccine Approaches
| Feature | Germline-Targeting Strategy | Lineage-Based Strategy |
|---|---|---|
| Core Principle | Engineered immunogens designed to bind and activate rare bnAb precursor B cells [56] [54] | Sequential immunogens based on viral evolution to guide B cell maturation [19] [53] |
| Primary Immunological Challenge | Overcoming low precursor frequency and potential immune ignorance [55] [54] | Navigating complex mutation pathways and avoiding off-target activation |
| Key Safety Considerations | Risk of eliciting non-neutralizing or off-specificity antibodies; theoretical autoimmunity concerns from designed immunogens [55] | Risk of immune fixation on variable epitopes; potential for eliciting antibodies with autoreactive features [19] |
| Representative Immunogens | eOD-GT8 60mer (CD4bs) [19] [56]; Epitope scaffolds for 10E8-class (gp41) [54] | CH505 TF gp120 (CD4bs) [19]; BG505 SOSIP.664 gp140 trimers [19] |
| Current Clinical Status | Early-phase human trials (e.g., IAVI G001) [19] | Preclinical and early clinical evaluation (e.g., HVTN 115) [19] |
Case Study 1: Germline-Targeting for HIV-1 VRC01-Class bnAbs
Experimental Protocol and Workflow
The germline-targeting approach for eliciting VRC01-class bnAbs, which target the CD4-binding site (CD4bs) on HIV-1 Env, was pioneered using the eOD-GT8 60mer immunogen. The experimental methodology typically involves a multi-stage process [56]:
- Immunogen Design and Production: The eOD-GT8 protein is engineered to possess high-affinity binding for the inferred germline versions of VRC01-class bnAbs. This protein is then self-assembled into a 60-mer nanoparticle to enhance B cell cross-linking and activation.
- Animal Models: Knock-in mouse models are generated, wherein a significant portion of their B cells express the germline-reverted heavy chain of a VRC01-class bnAb (e.g., VRC01) [56]. These models are crucial for evaluating the activation of rare, specific B cell precursors.
- Immunization and Analysis: Mice are primed with the eOD-GT8 60mer nanoparticle, often formulated with adjuvants like Ribi. The immune response is subsequently analyzed using techniques such as enzyme-linked immunosorbent assay (ELISA) to measure antigen-specific antibodies, flow cytometry to track activated B cell populations, and hybridoma generation for detailed characterization of isolated antibodies [56].
Table 2: Immune Response and Safety Profile of eOD-GT8 60mer
| Experimental Metric | Germline-Targeting (eOD-GT8 60mer) | Control (Native-like Immunogen) |
|---|---|---|
| Precursor B Cell Activation | Successful activation of VRC01-class precursors in knock-in mice [56] | Failed to activate VRC01-class precursors [56] |
| Induced Antibody Features | Short CDRL3 (5 aa); mutations enabling gp120 binding [56] | Not applicable |
| Affinity of Induced Antibodies | 72/115 antibodies showed no mutations from germline yet bound eOD-GT8 with high affinity [56] | Not applicable |
| Adjuvant Comparison (Alum vs. Ribi) | Ribi elicited more and higher-affinity antibodies than Alum [56] | Not applicable |
| Reported Adverse Events | No significant autoimmune reactions reported in mouse models [56] | Not applicable |
This case study demonstrates the precision and efficacy of the germline-targeting approach. The engineered eOD-GT8 immunogen successfully primed the desired B cell precursors, a feat that native-like immunogens failed to achieve. The induced antibodies exhibited key characteristics of VRC01-class bnAbs, including a critical short light chain complementarity determining region 3 (CDRL3) and acquired mutations that improved binding to more native-like HIV-1 envelope proteins [56]. From a safety perspective, the study reported no significant undesired immune reactions in the mouse models, indicating good initial tolerability for this priming immunogen [56].
Case Study 2: Germline-Targeting for HCDR3-Dominant 10E8-Class bnAbs
Experimental Protocol and Workflow
Targeting the membrane-proximal external region (MPER) of HIV-1 gp41 with 10E8-class bnAbs presents a greater challenge, as these antibodies are typically HCDR3-dominant and often possess long HCDR3s with specific lipid-binding motifs, raising theoretical concerns about autoreactivity [54]. The experimental protocol for this approach is as follows [54]:
- Epitope Scaffold Design: Protein scaffolds are engineered to present the 10E8 epitope while maintaining high-affinity binding to germline versions of 10E8-class bnAbs. These scaffolds are designed for structural mimicry of the native epitope.
- Nanoparticle Assembly: The epitope scaffolds are arrayed on protein nanoparticles or encoded by mRNA for delivery, creating a multivalent display to efficiently engage rare B cell precursors.
- Cross-species Evaluation: The immunogens are tested in stringent mouse models (e.g., bnAb precursor knock-in mice) and rhesus macaques to evaluate their ability to elicit 10E8-class precursor B cells with the required long HCDR3 and specific binding motif.
- Ex vivo Human B Cell Screening: The scaffolds are also used in screens with human naive B cells from donors to confirm binding to authentic human bnAb precursors.
Immune Response and Safety Profile
This research demonstrated that germline-targeting epitope scaffold nanoparticles could indeed elicit rare 10E8-class bnAb-precursor B cells with predefined binding specificities and critical HCDR3 features in both mouse models and rhesus macaques [54]. The scaffolds exhibited structural mimicry of the native epitope and successfully bound to bnAb-precursor human naive B cells in ex vivo screens, confirming their biological relevance [54]. A significant finding from a safety perspective was that the mRNA-encoded nanoparticles triggered similar precursor responses in mice, offering a potentially more flexible vaccine platform [54]. While MPER-targeting bnAbs like 2F5 and 4E10 have historically raised tolerance concerns due to their lipid reactivity, the successful priming of 10E8-class precursors without reported autoimmune complications in these pre-clinical models suggests that this specific germline-targeting strategy may circumvent some of these tolerability barriers [54]. This indicates progress in managing one of the most significant potential undesired immune reactions in HIV vaccine development.
The Scientist's Toolkit: Essential Reagents for Germline-Targeting Research
Table 3: Key Research Reagents for Germline-Targeting Vaccine Development
| Reagent / Tool | Primary Function | Application in Case Studies |
|---|---|---|
| Knock-in Mouse Models | In vivo models where B cells express germline-reverted bnAb genes; essential for evaluating immunogen efficacy and B cell activation [56] [54]. | Used to test eOD-GT8 60mer and 10E8-class scaffold nanoparticles. |
| Engineered Epitope Scaffolds | Proteins designed to mimic a specific bnAb epitope while stabilizing it and optimizing binding to germline precursors [54]. | Core component of both eOD-GT8 (CD4bs) and 10E8-class (MPER) immunogens. |
| Self-Assembling Nanoparticles | Platforms for multivalent display of immunogens; enhance B cell receptor cross-linking and activation of rare precursors [56] [54]. | eOD-GT8 60mer; protein nanoparticles for 10E8 epitope scaffolds. |
| mRNA Constructs | Nucleic acid platform encoding the immunogen; allows in vivo expression of the antigen, potentially simplifying vaccine formulation [54]. | Used to deliver 10E8-class targeting nanoparticles in mice. |
| Adjuvant Systems (e.g., Ribi) | Immune potentiators added to vaccines to enhance the magnitude and quality of the adaptive immune response. | Compared with alum in the eOD-GT8 study, with Ribi showing superior results [56]. |
The comparative analysis of germline-targeting and lineage-based vaccine strategies reveals a complex landscape of efficacy, precision, and safety. Germline-targeting immunogens, as exemplified by the eOD-GT8 60mer and 10E8-class epitope scaffolds, demonstrate a remarkable ability to precisely engage and expand rare bnAb-precursor B cells that are often ignored by native-like immunogens [56] [54]. A key safety advantage of this approach is its potential to steer the immune response toward desired bnAb lineages from the outset, theoretically reducing the risk of eliciting non-neutralizing or strain-specific antibodies that could dominate the response. However, the engineered nature of these immunogens and their focus on activating B cells with bnAb-like traits (e.g., long HCDR3s, specific motifs) necessitate rigorous and long-term safety monitoring in advanced models for potential undesired immune reactions, including autoreactivity. The recent success of mRNA-encoded nanoparticles for the 10E8-class target further expands the technological arsenal for this strategy [54].
In contrast, lineage-based strategies, which employ a series of native-like immunogens, face their own safety and tolerability challenges, primarily the risk of the immune response being diverted toward immunodominant, variable epitopes rather than the conserved bnAb targets. The critical insight from the AMP clinical trials—that a single bnAb specificity is insufficient for broad protection—underscores that any successful HIV vaccine will likely need to incorporate elements of both strategies to elicit a multi-pronged bnAb response [19]. Future research must continue to refine immunogen design to improve safety profiles and will need to carefully evaluate the potential for cumulative undesired immune reactions when these strategies are combined in multi-step vaccination regimens. The ultimate goal remains the development of a vaccine that is not only effective but also exhibits a favorable safety and tolerability profile for widespread clinical use.
Optimizing Intervals and Dosages in Sequential Immunization Schedules
The development of vaccines against rapidly evolving pathogens like HIV-1 represents one of the most formidable challenges in modern immunology. Traditional vaccine approaches, which often rely on single immunogens or simple prime-boost regimens, have proven inadequate for eliciting the broad and potent immune responses required for protection. In response to this challenge, sequential immunization strategies have emerged as a sophisticated alternative, designed to actively guide the immune system through a predetermined maturation pathway. These strategies involve administering a series of distinct immunogens in a specific order, with carefully optimized intervals and dosages between administrations. The fundamental objective is to recapitulate the natural antibody maturation process that occurs during chronic infection, but within a compressed timeframe and with greater precision.
The two most prominent approaches in this domain are germline-targeting and lineage-based vaccine strategies, which form the central comparative axis of this analysis. Germline-targeting focuses on engaging rare precursor B cells that possess inherent potential to develop into broadly neutralizing antibody (bNAb) producers, while lineage-based approaches aim to guide the maturation of these precursors along pathways reconstructed from natural infection. Both paradigms face the critical challenge of determining the optimal sequence of immunogens, the dosage for each stage, and the intervals between administrations that will most effectively drive B cells toward bnAb production. This comparison guide synthesizes current experimental data and methodological approaches to address these optimization challenges, providing researchers with a structured framework for evaluating and implementing sequential immunization schedules in preclinical and clinical settings.
Comparative Analysis of Sequential Immunization Strategies
Conceptual Frameworks and Underlying Principles
Germline-Targeting Strategies initiate the immunization sequence with engineered immunogens specifically designed to activate rare B cell precursors that possess the genetic signature of bNAb potential. These preliminary immunogens, such as eOD-GT8 60mer, are characterized by their enhanced ability to bind germline-encoded B cell receptors (BCRs) that would otherwise show weak or no reactivity to native viral proteins [14]. Following this priming phase, subsequent booster immunizations employ antigens that progressively more closely resemble native viral structures, with the goal of steering the affinity maturation process toward bNAb development. The glycan engineering and epitope scaffolding utilized in these immunogens are crucial for focusing immune responses on conserved vulnerable sites while avoiding immunodominant variable regions [11].
In contrast, Lineage-Based Vaccination Strategies leverage reverse engineering of naturally occurring bNAb lineages from individuals with chronic infection. Researchers computationally reconstruct the ancestral B cell receptors and intermediate mutants that led to potent bNAbs, then design a series of immunogens that correspond to these historical maturation steps [1]. This approach aims to recapitulate the natural evolutionary pathway of bNAb development, but in an accelerated timeframe. The strategy depends on identifying the key improbable mutations that were critical for breadth development in natural infection and designing immunogens that selectively promote B cells possessing these mutations.
A third emerging approach, the Germline/Lineage Agnostic Strategy, utilizes native-like envelope trimers in sequential immunization to engage any naive B cell recognizing bNAb target epitopes, allowing the polyclonal response to be focused on conserved targets through heterologous boosting [1]. This method leverages the natural propensity of the immune system to mature responses against functionally constrained epitopes without predetermined B cell lineages.
Table 1: Fundamental Characteristics of Sequential Immunization Strategies
| Strategy Characteristic | Germline-Targeting | Lineage-Based | Germline/Lineage Agnostic |
|---|---|---|---|
| Starting Immunogen | Engineered to bind germline BCRs | Based on ancestral viral sequences | Native-like trimers |
| B Cell Selection Basis | Genetic signatures of bNAb potential | Historical maturation pathways | Epitope specificity only |
| Immunogen Sequence Design | Structure-based rational design | Phylogenetic reconstruction | Antigenic distance-based |
| Maturation Guidance | Epitope focusing | Mutation-guided | Polyclonal competition |
| Personalization Requirement | Dependent on Ig germline genetics | Dependent on shared lineages | Not required |
Experimental Models and Clinical Evaluation
Substantial progress in optimizing sequential immunization has been achieved through sophisticated animal models, including knock-in mice expressing germline-reverted bNAb precursors and non-human primates. The seminal study by Jardine et al. demonstrated that immunization with a germline-targeting immunogen successfully activated VRC01-class bnAb precursors in knock-in mice, while native-like immunogens failed to do so [57]. This established the proof-of-concept for the germline-targeting approach and highlighted the critical importance of the initial immunogen in engaging the desired B cell lineages.
Recent clinical trials have provided the first evidence that these approaches can engage human immune systems as designed. The IAVI G001 trial (NCT03547245) demonstrated that the eOD-GT8 60mer immunogen elicited desired precursor B cell responses in 35 of 36 (97%) participants, with only one individual failing to respond due to lacking the necessary IGHV1-2 alleles [1]. This remarkable response rate validates the germline-targeting concept in humans and highlights the importance of host genetic factors in vaccine responsiveness. Subsequent trials including IAVI G002 (NCT05001373) and IAVI G003 (NCT05414786) have further advanced this approach using mRNA delivery platforms, with initial observations suggesting that mRNA vaccination primes VRC01-class B cell precursors at least as effectively as protein immunization [1].
For the lineage-based approach, the HVTN 133 trial evaluated an MPER-targeting immunogen, demonstrating that binding antibody responses could be elicited in most participants after just two doses, with some serum samples neutralizing 15% of tier 2 HIV strains and 35% of clade B strains [14]. Importantly, the precursor B cells appeared to remain in a state of ongoing development, a promising finding for achieving further maturation with additional boosts.
Table 2: Comparative Clinical Trial Outcomes of Sequential Immunization Strategies
| Trial / Study | Strategy | Immunogen Sequence | Dosing Interval | Key Findings |
|---|---|---|---|---|
| IAVI G001 (NCT03547245) | Germline-Targeting | eOD-GT8 60mer (prime) | Not specified | 97% response rate; VRC01-class precursors activated |
| IAVI G002 (NCT05001373) | Germline-Targeting | eOD-GT8 60mer (prime) → core-g28v2 60mer (boost) | Under investigation | mRNA platform enhanced IGHV1-2 mutations compared to protein |
| HVTN 301 (NCT05471076) | Germline-Targeting | 426c.Mod.Core (prime/boost) | Under investigation | 38 mAbs isolated; similarities to VRC01 reactivity |
| HVTN 133 | Lineage-Based | MPER-peptide LNP (prime/boost) | Not specified | bnAbs emerged within weeks; 15% tier 2 neutralization |
| Infant Macaque Study | Germline-Targeting | BG505 SOSIP GT1.1 (3 immunizations) | Not specified | VRC01-class B cells accumulated bnAb-associated mutations |
Methodologies for Evaluating Sequential Immunization
B Cell Repertoire Analysis Techniques
The optimization of intervals and dosages in sequential immunization relies heavily on advanced methods for tracking antigen-specific B cell lineages and assessing their maturation status. High-throughput sequencing of B cell receptor repertoires enables researchers to monitor the expansion and somatic hypermutation of vaccine-induced B cell clones over time. The virtual workshop sponsored by NIAID on August 13, 2024 brought together experts to standardize and improve these analytical methods, emphasizing the need for cost-effective deep characterization of vaccine-induced repertoires [1]. Key methodologies discussed included next-generation sequencing of immunoglobulin genes, bioinformatic pipeline development for identifying antigen-enriched B cell lineages, and phylogenetic analysis to reconstruct B cell clonal families.
Complementing repertoire sequencing, antigen-specific B cell sorting using fluorophore-labeled recombinant proteins allows for the isolation and detailed characterization of vaccine-responsive B cells. Flow cytometry and single-cell RNA sequencing further enable the identification of B cell activation states, germinal center residency, and transcriptional signatures associated with effective antibody maturation. These techniques collectively provide a multidimensional view of how different immunization intervals and dosages influence the breadth, depth, and quality of B cell responses.
Diagram 1: B Cell Maturation Cycle. This diagram illustrates the cyclical process of germinal center reactions that occurs after each immunization in a sequence, driving B cells toward increased affinity and breadth.
Antibody Functional and Structural Characterization
Determining the functional consequences of different immunization schedules requires comprehensive assessment of antibody neutralizing activity and epitope specificity. Standardized pseudovirus neutralization assays measure the breadth and potency of serum responses or isolated monoclonal antibodies against diverse viral panels. For HIV vaccine development, neutralization is typically assessed against tier 2 viruses, which are more resistant to neutralization and thus better indicators of protective potential [14].
At the structural level, cryo-electron microscopy (cryo-EM) and X-ray crystallography provide atomic-resolution insights into how vaccine-induced antibodies interact with their target epitopes. These techniques can verify whether immunization sequences are successfully guiding antibody development toward recognition of conserved neutralizing sites. In the HVTN 301 trial, cryo-EM analysis of 38 monoclonal antibodies induced by the 426c.Mod.Core immunogen confirmed similarities to VRC01-class antibodies in their mode of binding [1]. Biolayer interferometry (BLI) further offers quantitative data on antibody affinity and kinetics, enabling precise measurement of how affinity maturation progresses with each boost in the sequence.
Optimization Parameters for Sequential Immunization
Interval Optimization Between Doses
The timing between sequential immunizations represents a critical parameter that must balance competing biological processes. Sufficient intervals must be allowed for the completion of germinal center reactions, where B cells undergo somatic hypermutation and affinity-based selection, yet intervals should not be so long that the response wanes substantially. Studies in knock-in mouse models have demonstrated that intervals of 4-8 weeks between prime and boost effectively support the expansion and maturation of bNAb precursor lineages [57] [14]. However, optimal intervals may vary depending on the specific immunogens used and the stage in the sequence, with later boosts potentially requiring longer intervals to allow for more extensive maturation.
Evidence from COVID-19 vaccine studies suggests that longer intervals between prime and boost can enhance the magnitude and quality of antibody responses. Research on 2024-2025 COVID-19 vaccines showed that protection against hospitalization was sustained through 90-179 days after vaccination, indicating that extended intervals do not necessarily compromise efficacy [58]. For HIV sequential immunization, the appropriate interval likely depends on the specific stage of the regimen, with initial primes and boosts possibly benefiting from shorter intervals (4-8 weeks) to maintain momentum in the maturation process, while later polishing immunizations might employ longer intervals (3-6 months) to enable more thorough germinal center selection.
Dosage Optimization Strategies
Dosage optimization must consider both the absolute amount of immunogen and the delivery format. The HVTN 301 trial is explicitly comparing full bolus versus fractional doses of the 426c.Mod.Core immunogen, recognizing that dosage can qualitatively influence the B cell response by affecting the strength of BCR signaling and subsequent maturation [1]. Emerging data from mRNA platforms suggest that this delivery method may enhance immunogenicity even at lower doses, potentially due to more efficient in vivo antigen expression and prolonged exposure.
Recent approaches have also explored heterologous delivery systems within a sequence, such as priming with protein nanoparticles followed by mRNA boosts. Studies with the N332-GT5 immunogen demonstrated that mRNA delivery drove superior B cell maturation compared to protein subunit vaccines in mouse models [14]. This highlights how dosage cannot be considered independently of delivery platform, as the same nominal dose may have markedly different biological effects depending on formulation and administration route.
Table 3: Optimization Parameters for Sequential Immunization Schedules
| Parameter | Current Evidence | Knowledge Gaps | Assessment Methods |
|---|---|---|---|
| Interval Between Doses | 4-8 weeks common in preclinical models; longer intervals may enhance quality | Optimal interval duration at different maturation stages; effect on memory formation | B cell receptor sequencing; longitudinal serum antibody analysis |
| Immunogen Dosage | Full bolus vs. fractional dosing under investigation; mRNA may allow dose-sparing | Minimum effective dose for lineage engagement; dose-response relationships | Antigen-specific B cell frequency; antibody affinity measurements |
| Sequence Length | Multi-step sequences (3-5 immunizations) show progressive maturation | Number of boosts needed for breadth; individual variation in required steps | Neutralization breadth against heterologous viruses; somatic mutation accumulation |
| Delivery Platform | mRNA enhances immunogenicity; protein subunits allow precise structural control | Optimal platform sequences; effect on T follicular helper responses | Germinal center B cell and Tfh quantification; antigen persistence measurement |
Essential Research Reagents and Tools
The implementation and optimization of sequential immunization schedules depends on a specialized toolkit of reagents and analytical methods. The table below catalogues key resources that enable the precise engineering, delivery, and evaluation of sequential vaccine regimens.
Table 4: Essential Research Reagents for Sequential Immunization Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Engineered Immunogens | eOD-GT8 60mer, 426c.Mod.Core, BG505 SOSIP GT1.1, core-g28v2 60mer, N332-GT5 | Prime and boost components designed to engage and mature bNAb precursors |
| Delivery Platforms | Lipid nanoparticles (LNPs), mRNA constructs, virus-like particles (VLPs), protein subunits with adjuvants | Antigen presentation format influencing immunogenicity and response quality |
| Animal Models | Knock-in mice expressing germline-reverted bNAb precursors, humanized mice, non-human primates | Preclinical evaluation of immunization sequences and maturation pathways |
| Analysis Reagents | Fluorophore-labeled Env proteins, antigen-specific B cell sorting tools, single-cell RNA sequencing kits | Tracking and characterization of vaccine-induced B cell responses |
| Assay Systems | Pseudovirus neutralization assays, biolayer interferometry, cryo-EM structural analysis | Functional and structural assessment of antibody responses |
Integrated View of Strategy Implementation
The successful implementation of sequential immunization strategies requires careful coordination of multiple elements beyond just the immunogens themselves. Adjuvant selection plays a crucial role in shaping the quality of the immune response, with different adjuvants potentially being optimal for different stages of the sequence. The HVTN 301 trial utilizes the adjuvant 3M-052-AF combined with aluminum hydroxide to enhance the immunogenicity of the 426c.Mod.Core nanoparticle [1], while other approaches may employ different adjuvant formulations tailored to promote germinal center responses or specific antibody classes.
The growing recognition of host genetic factors necessitates consideration of population diversity in vaccine design. The failure of one participant in the IAVI G001 trial to respond to the eOD-GT8 60mer immunogen was directly attributable to the absence of permissive IGHV1-2 alleles required for VRC01-class antibody development [1]. This highlights that germline-targeting approaches may need to incorporate multiple immunogens designed to engage different germline precursors, or be combined with lineage-agnostic strategies to achieve broad population coverage.
Diagram 2: Sequential Immunization Workflow. This diagram outlines the generalized workflow for implementing and evaluating a sequential immunization regimen, highlighting key decision points and analytical checkpoints.
Looking forward, the field is moving toward increasingly personalized vaccination approaches that account for individual genetic backgrounds and immune histories. The integration of high-throughput screening methods with computational modeling of B cell maturation pathways will enable more rational design of immunization sequences tailored to maximize the probability of achieving bNAb development across diverse populations. As these technologies mature, the distinction between germline-targeting and lineage-based strategies may blur, giving rise to integrated approaches that leverage the strengths of both paradigms while mitigating their respective limitations.
The systematic optimization of intervals and dosages in sequential immunization schedules represents a frontier in vaccine development for challenging pathogens like HIV-1. Both germline-targeting and lineage-based strategies show promising early results in engaging desired B cell precursors and initiating their maturation along pathways toward broad neutralization. Current evidence suggests that 4-8 week intervals between immunizations effectively support the germinal center reactions necessary for affinity maturation, while dosage optimization must consider both the absolute amount of immunogen and the delivery platform.
The comparative analysis presented in this guide reveals that germline-targeting and lineage-based approaches, while conceptually distinct, face shared challenges in determining the optimal sequence of immunogens and managing individual variation in response. The emerging use of mRNA platforms appears to enhance immunogenicity and may allow for more flexible dosing strategies. Future progress will depend on continued refinement of B cell repertoire analysis methods, longitudinal tracking of vaccine-induced lineages, and iterative refinement of immunization sequences based on clinical observations. As these sophisticated vaccine strategies advance, they hold the potential to transform our approach not only to HIV but to other antigenically variable pathogens that have eluded conventional vaccine development.
Vaccine development faces a formidable obstacle: individual genetic variation that profoundly shapes immune responses. As vaccine strategies grow more sophisticated, understanding this genetic hurdle becomes paramount for designing effective immunization campaigns. This article examines how host genetics influence vaccine response through the comparative lens of two advanced vaccine design paradigms—germline-targeting strategies (which aim to guide rare B cells toward producing broadly neutralizing antibodies) and lineage-based strategies (which account for circulating pathogen diversity). Evidence from recent HIV, SARS-CoV-2, and influenza trials reveals that specific genetic polymorphisms can determine vaccine success or failure, presenting both challenges and opportunities for precision vaccinology.
Genetic Mechanisms of Vaccine Response Variation
Host genetic factors influence vaccine immunogenicity through several key biological pathways, with the most pronounced effects occurring in immune recognition, cell activation, and antibody production.
Key Genetic Factors and Their Impact
Table 1: Host Genetic Factors Influencing Vaccine Response
| Genetic Factor | Biological Function | Vaccine Example | Impact on Response |
|---|---|---|---|
| IGHV1-2 alleles | Encodes B cell receptor heavy chain | HIV germline-targeting vaccines | IGHV1-2*02 associated with 3-4× higher precursor frequency than *04 allele [4] |
| HLA polymorphisms | Antigen presentation | Measles, Hepatitis B | Account for up to 30% of inter-individual variation in antibody levels [59] |
| TLR gene variants | Pathogen recognition and innate immune activation | Influenza, measles | TLR3 polymorphisms linked to low measles antibody production post-vaccination [59] |
| CCR5 Δ32 mutation | Chemokine receptor function | Hepatitis B | Homozygous genotype associated with reduced vaccine immunogenicity [59] |
The diagram below illustrates how these genetic factors influence the vaccine response pathway from antigen recognition to immune memory formation:
Comparative Analysis: Germline-Targeting vs. Lineage-Based Vaccine Strategies
These two advanced vaccine approaches address pathogen diversity through fundamentally different mechanisms, each with distinct genetic considerations.
Germline-Targeting Vaccines
This strategy uses specifically engineered immunogens to prime rare naive B cells that have genetic signatures enabling them to develop into broadly neutralizing antibodies (bNAbs). The approach requires sequential immunization with priming immunogens that engage precursor B cells, followed by boosting immunogens that guide these cells through affinity maturation [14].
HIV vaccine development represents the most advanced application of this strategy. The eOD-GT8 60mer immunogen successfully primed VRC01-class B cell precursors in 97% of recipients (35 of 36) in the IAVI G001 trial [1]. These B cells require specific immunoglobulin heavy chain variable (IGHV) genes, particularly IGHV1-2*02 or *04 alleles, to produce bNAbs capable of neutralizing diverse HIV strains [4].
Critical genetic findings from these trials reveal that:
- Individuals with IGHV1-2*02 alleles showed approximately 4-fold higher frequencies of naive precursor B cells compared to those with *04 alleles [4]
- The one non-responder in the IAVI G001 trial had an 05/06 genotype lacking the necessary *02 or *04 alleles [4]
- mRNA delivery of germline-targeting immunogens (IAVI G002 trial) induced greater somatic hypermutation in IGHV1-2-using B cells than protein delivery [1]
Lineage-Based Vaccines
This approach addresses pathogen diversity by selecting vaccine components that match circulating lineages, as exemplified by influenza B vaccination. Trivalent influenza vaccines contain only one influenza B lineage (B/Victoria or B/Yamagata), creating potential for mismatch when the circulating lineage differs from the vaccine lineage [60].
Table 2: Lineage-Based Vaccine Performance (2000-2010)
| Season | Vaccine Lineage | Circulating Lineage | Match/Mismatch | Reported Efficacy |
|---|---|---|---|---|
| 2001-2002 | B/Yamagata | B/Victoria | Mismatch | ~50% protection against mismatched strain [60] |
| 2003-2004 | B/Victoria | B/Yamagata | Mismatch | Reduced efficacy due to lineage mismatch [60] |
| 2007-2008 | B/Victoria | B/Yamagata | Mismatch | 50% protection despite mismatch [60] |
| 2008-2009 | B/Yamagata | B/Victoria | Mismatch | Reduced efficacy due to lineage mismatch [60] |
Research indicates that lineage selection strategies can optimize trivalent vaccine effectiveness. A "hedging strategy" that considers residual protection from previous vaccinations, antigenic drift, and population immunity could capture some benefits of quadrivalent vaccines without the associated costs [60].
The diagram below illustrates the fundamental differences between these two vaccine strategies:
Experimental Protocols and Methodologies
IGHV Genotyping in Germline-Targeting Trials
Personalized immunoglobulin genotyping provides critical insights into vaccine responsiveness. The methodology employed in the IAVI G001 trial involved:
IgM Library Preparation: Peripheral blood mononuclear cells (PBMCs) were collected from trial participants pre- and post-vaccination. IgM-specific B cell receptors were amplified to capture the naive repertoire [4].
High-Throughput Sequencing: Unique molecular identifiers (UMIs) were incorporated during cDNA synthesis to enable accurate quantification of mRNA expression frequencies for different IGHV alleles [4].
Germline Allele Inference: The IgDiscover tool was applied to achieve nucleotide-level precision genotyping of IGHV1-2 alleles, identifying *02, *04, *05, *06, and the synonymous *02_S4953 variant [4].
HCDR3 Analysis: Unique heavy chain complementarity determining region 3 (HCDR3) sequences within IGHV1-2 mRNAs were counted to quantify unique IGHV1-2 B cells in each participant's repertoire [4].
This protocol revealed that mRNA expression frequency of IGHV1-202 was approximately 3.1% in homozygous individuals, compared to only 0.9% for IGHV1-204—explaining the differential vaccine response based on genotype [4].
Influenza B Lineage Selection Methodology
The lineage-based approach employs distinct experimental protocols to inform vaccine composition:
Antisera Collection: Pre- and post-vaccination antisera were obtained from vaccine trials across multiple countries (United States, Australia, New Zealand, Japan, China) [60].
Hemagglutination Inhibition (HI) Titration: HI titers were measured against both B/Victoria (e.g., B/Brisbane/60/2008) and B/Yamagata (e.g., B/Wisconsin/1/2010) lineage viruses to quantify cross-reactivity [60].
Population Immunity Modeling: A "hedging strategy" was developed that considers residual protection from previous vaccinations, antigenic drift, and newcomers to annual vaccination programs to optimize lineage selection [60].
Efficacy Estimation: Protection levels were estimated for different lineage selection strategies by analyzing historical data on vaccine lineage matches and mismatches from 2000-2010 [60].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Vaccine Immunology Studies
| Reagent / Tool | Application | Function in Research |
|---|---|---|
| eOD-GT8 60mer | HIV germline-targeting priming | Engineered gp120 nanoparticle immunogen designed to activate VRC01-class B cell precursors [1] [14] |
| BG505 SOSIP GT1.1 | HIV germline-targeting | Native-like trimer immunogen modified to bind VRC01-class and apex-specific B cell precursors [1] [61] |
| Hemagglutination Inhibition (HI) Assay | Influenza lineage studies | Quantifies antibody-mediated inhibition of viral hemagglutination to measure cross-reactivity between lineages [60] |
| IgDiscover Tool | IGHV genotyping | Computational tool for nucleotide-level germline allele inference from high-throughput BCR sequencing data [4] |
| Diversity Outbred (DO) Mice | Host genetics modeling | Outbred mouse population with characterizable genetic diversity for studying host genetic effects on vaccine responses [62] |
| Biolayer Interferometry (BLI) | Antibody affinity characterization | Measures binding kinetics and affinity of vaccine-induced antibodies for target immunogens [1] |
The integration of host genetics into vaccine development represents both a formidable challenge and tremendous opportunity. Germline-targeting strategies offer precision but face genetic barriers like IGHV allele restrictions, while lineage-based approaches address population-level diversity but struggle with unpredictable strain circulation. The future of vaccinology lies in developing strategies that either circumvent these genetic hurdles through sophisticated immunogen design or leverage genetic insights to optimize vaccine composition for specific populations. As demonstrated by recent successes in HIV and influenza vaccine research, acknowledging and addressing these genetic factors is essential for advancing toward effective, broadly protective vaccines against challenging pathogens.
Balancing Breadth, Potency, and Durability in Elicited Immunity
The quest for vaccines against antigenically diverse pathogens such as HIV-1 represents one of the most significant challenges in modern immunology. Traditional empirical vaccine approaches, which have succeeded for many viral diseases, have consistently failed to elicit the broad and potent immunity required to prevent HIV-1 infection [8]. This failure has catalyzed the development of two sophisticated, structure-guided strategies: germline-targeting and lineage-based vaccine design. Both approaches aim to overcome HIV's extraordinary diversity and evasion tactics by systematically guiding the immune system to produce broadly neutralizing antibodies (bnAbs)—antibodies capable of neutralizing a wide spectrum of viral variants [12] [55]. While they share this ultimate goal, they diverge fundamentally in their conceptual frameworks, technical execution, and immunological navigation. This comparison guide provides an objective analysis of the comparative effectiveness of these two strategies, drawing on current experimental data to evaluate their respective capacities to elicit immunity with the necessary breadth, potency, and durability for protection against complex pathogens.
Conceptual Frameworks and Key Distinctions
Germline-Targeting Vaccine Strategy
The germline-targeting approach operates on the principle of reverse engineering. It begins with a known bnAb from an infected individual and designs a priming immunogen (e.g., eOD-GT8 60mer) specifically to activate rare, naive B cells that possess the genetic potential to develop into that bnAb lineage [12] [54]. This strategy shepherds the immune system through a predefined path using a sequence of distinct immunogens. The initial immunogen is engineered to bind specifically to the unmutated, "germline" versions of B cell receptors (BCRs) that are precursors to desired bnAbs [12] [14]. Subsequent booster immunogens are then designed to sequentially "shape" and "polish" the response, guiding B cells through increasing levels of maturation and affinity until they can produce potent, broad antibodies [12] [14]. The IAVI G001 clinical trial demonstrated proof-of-concept for this approach, showing that the eOD-GT8 60mer immunogen could successfully prime VRC01-class bnAb-precursor B cells in 97% of vaccine recipients [10] [14].
Lineage-Based Vaccine Strategy
In contrast, the lineage-based strategy focuses on reconstructing natural maturation pathways. This approach involves deeply studying the co-evolution of viruses and antibodies in individuals who naturally develop bnAbs over time [8]. Researchers computationally reconstruct the historical development of a potent bnAb lineage from its germline ancestor to its mature form [10] [8]. The vaccine regimen then aims to recapitulate this natural evolutionary pathway using a series of immunogens that mirror the sequential viral variants that drove bnAb development in natural infection [8]. Rather than designing de novo immunogens to bind predefined germline precursors, this strategy uses immunogens derived from actual viral sequences that were involved in the natural development of bnAbs, with the goal of guiding the immune system along a known productive pathway [8].
Table: Conceptual Comparison of Germline-Targeting and Lineage-Based Vaccine Strategies
| Feature | Germline-Targeting Strategy | Lineage-Based Strategy |
|---|---|---|
| Design Principle | Reverse engineering from mature bnAb structure | Forward reconstruction of natural bnAb lineage |
| Starting Point | Known bnAb with desired characteristics | Natural bnAb maturation pathway from infection |
| Immunogen Design | Engineered proteins (e.g., eOD-GT8) to bind germline BCRs | Viral envelope variants from actual lineage history |
| Vaccination Series | Predefined sequence of distinct immunogens | Sequential immunogens mirroring natural evolution |
| Target B Cells | Rare naive B cells with specific genetic signatures | B cell lineages with observed developmental pathways |
Diagram 1: Conceptual workflow comparison between germline-targeting and lineage-based vaccine strategies, highlighting their distinct approaches to eliciting broadly neutralizing antibodies.
Comparative Experimental Data and Performance Metrics
Breadth of Elicited Immune Responses
Breadth refers to the proportion of diverse viral strains that elicited antibodies can neutralize. The germline-targeting approach has demonstrated promising results in priming B cells that target multiple conserved epitopes on HIV-1 Envelope. The eOD-GT8 60mer immunogen successfully primed precursors for VRC01-class bnAbs targeting the CD4-binding site [12] [10]. Similarly, nanoparticle immunogens targeting the gp41 MPER region have elicited precursors of 10E8-class bnAbs, which show exceptional breadth (92-98% of HIV isolates) [54]. Recent research has also developed ApexGT trimers designed to prime bnAb precursors against the Env Apex region, another conserved site [63].
The lineage-based approach aims to achieve breadth by recapitulating the natural process where B cells accumulate mutations that gradually increase their ability to recognize diverse viral variants. Studies of natural HIV infection show that bnAbs develop through ongoing co-evolution with escaping viruses, progressively expanding their breadth [8]. The lineage approach seeks to replicate this process through sequential immunization with carefully designed immunogens that represent key stages in this expansion.
Potency of Neutralization
Potency refers to the concentration of antibody required to neutralize a virus, typically measured as the half-maximal inhibitory concentration (IC50). The germline-targeting approach faces challenges in achieving high potency, as the initial primed antibodies typically require extensive maturation to develop potent neutralization. In the IAVI G001 trial, while priming was successful, the elicited antibodies were precursors that required further maturation to develop significant potency [12] [10]. Recent studies of MPER-targeting immunogens show that while precursor B cells are activated, they often struggle to compete with higher-affinity B cell clones, limiting their potency development [54].
Lineage-based strategies aim to achieve potency by guiding antibodies through maturation pathways that are known to produce highly potent bnAbs. The sequential immunization with variants that progressively select for higher affinity is designed to build potency stepwise, similar to natural infection [8]. However, this process is complex and requires precise immunogen design at each stage to avoid dead ends.
Table: Experimental Outcomes from Key Vaccine Studies
| Study/Trial | Strategy | Target | Model System | Key Outcome | Breadth Assessment | Potency Assessment |
|---|---|---|---|---|---|---|
| IAVI G001 [12] [10] | Germline-targeting | CD4-binding site (VRC01-class) | Humans (Phase 1) | 97% of participants showed bnAb precursors | Precursors activated with desired specificity | Required further maturation for neutralization |
| Schiffner et al., 2024 [54] | Germline-targeting | gp41 MPER (10E8-class) | Mice & Macaques | Nanoparticles induced bnAb-precursor responses | Targeted highly conserved epitope (98% breadth potential) | Precursors faced competition from higher-affinity clones |
| HVTN 133 [14] | Lineage-based | gp41 MPER | Humans (Phase 1) | Neutralized 15% of tier 2 HIV strains after 2-3 doses | Moderate breadth achieved in short timeframe | Potency sufficient for partial neutralization |
| ApexGT6 Study [63] | Germline-targeting | Env Apex region | Rhesus macaques | Primed Apex bnAb-related precursors with long HCDR3s | Targeted conserved Apex epitope | Dependent on rare B cells with specific motifs |
Durability of Immune Responses
Durability encompasses both the persistence of antibody production and the stability of the B cell memory response. For germline-targeting approaches, a significant challenge is the longevity of the primed rare B cell clones. Studies show that germinal center residency and persistence of primed precursors are critical for successful maturation toward bnAbs [54]. In the MPER-targeting studies, only a subset of primed precursor clones managed to establish long-term germinal center residency necessary for full maturation [54].
Lineage-based approaches face durability challenges related to the complexity of the required maturation pathway. If the sequential immunization does not perfectly match the natural evolutionary pathway, the response may not persist or may veer toward non-neutralizing specificities [8]. The need for multiple boosts over an extended period presents practical challenges for vaccine deployment.
Detailed Experimental Protocols and Methodologies
Germline-Targeting Immunogen Design and Validation
The development of germline-targeting immunogens follows a rigorous structure-based design process. For the eOD-GT8 60mer immunogen, researchers first identified the mature VRC01 bnAb and worked backward to engineer an immunogen that could bind its germline precursor [12] [10]. This involved:
Structural Analysis: X-ray crystallography and cryo-electron microscopy were used to determine atomic-level structures of bnAbs in complex with their HIV Envelope targets [55] [54].
Epitope Scaffolding: For difficult-to-target epitopes like the MPER region, researchers engineered scaffold proteins that present the bnAb epitope while stabilizing it in a conformation that can engage germline BCRs [54].
Multivalent Display: Immunogens were displayed on self-assembling nanoparticles (60mers) to enhance B cell activation through avidity effects [12] [54].
In Vitro Binding Validation: Surface plasmon resonance (SPR) and bio-layer interferometry were used to quantify binding affinity to germline-reverted bnAbs and assess cross-reactivity [54] [63].
Animal Model Testing: Immunogens were tested in transgenic mouse models expressing human immunoglobulin genes, followed by non-human primate studies [54] [63].
Diagram 2: Experimental validation workflow for germline-targeting immunogens, from initial identification of target antibodies through clinical evaluation.
Lineage-Based Vaccine Development Protocol
The lineage-based approach employs distinct methodological strategies centered around natural infection studies:
Longitudinal Sampling: Collection of blood samples from HIV-infected individuals over time, particularly those who develop broad neutralization [8].
B Cell Clonal Lineage Analysis: Single B cell sorting and sequencing to reconstruct the developmental history of bnAb lineages from germline to maturity [8].
Ancestral Sequence Reconstruction: Computational methods to infer intermediate antibodies and viral envelope sequences that drove bnAb maturation [8].
Immunogen Design Based on Natural Variants: Design of vaccine immunogens based on actual viral sequences from the infected individual's bnAb lineage [8].
Sequential Immunization Testing: Evaluation of the immunogen series in animal models to assess their ability to guide B cell maturation along the desired pathway.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table: Key Research Reagents for Germline-Targeting and Lineage-Based Vaccine Development
| Reagent/Solution | Function/Application | Examples in Current Research |
|---|---|---|
| Stabilized Envelope Trimers | Native-like HIV Env proteins for structural studies and immunization | SOSIP trimers, BG505.SOSIP [12] |
| Epitope Scaffolds | Engineered proteins presenting bnAb epitopes in isolation | MPER scaffolds for 10E8 priming [54] |
| Nanoparticle Platforms | Multivalent display of immunogens for enhanced B cell activation | eOD-GT8 60mer, ferritin nanoparticles [10] [54] |
| mRNA-LNP Formulations | Delivery of genetic instructions for in vivo immunogen production | mRNA-1644 (Moderna) [10] [14] |
| Adjuvant Systems | Enhancement of immune responses to vaccine immunogens | AS01B, 3M-052 (TLR7/8 agonist) [10] [4] |
| Transgenic Mouse Models | In vivo testing of human-targeted immunogens | Mice expressing human immunoglobulin genes [54] [63] |
| B Cell Sorting Technologies | Isolation of rare antigen-specific B cells for analysis | Fluorescence-activated cell sorting, antigen baits [8] [4] |
| Structural Biology Tools | Atomic-level characterization of antibody-antigen interactions | Cryo-electron microscopy, X-ray crystallography [54] [63] |
The comparative analysis of germline-targeting and lineage-based vaccine strategies reveals complementary strengths and challenges. Germline-targeting approaches demonstrate superior precision in initiating desired immune responses, with strong clinical proof-of-concept for priming rare bnAb precursors [12] [10] [14]. However, these approaches face significant hurdles in guiding these precursors to full maturity with sufficient potency and durability. Lineage-based strategies benefit from following nature's blueprint for bnAb development but require exquisite precision in immunogen sequencing and face practical challenges in implementation.
Current research indicates that the most promising path forward may involve hybrid approaches that leverage the precision priming of germline-targeting with the maturation guidance of lineage-based strategies. Furthermore, the integration of mRNA-LNP delivery platforms offers enhanced flexibility for iterative immunogen testing and deployment [10] [14]. The critical importance of human genetic variation in shaping responses to both strategies [4] underscores the need for personalized vaccinology approaches that account for individual immunoglobulin genotypes.
For researchers and drug development professionals, the strategic selection between these approaches depends heavily on target epitope characteristics, available structural data, and specific product development considerations. Both strategies represent monumental advances in rational vaccine design and continue to evolve through iterative clinical evaluation. The emerging clinical data from ongoing trials will be crucial for determining the ultimate feasibility of these sophisticated approaches for preventing HIV and other challenging pathogens.
Evaluating Efficacy, Effectiveness, and Strategic Fit
The development of an effective HIV vaccine represents one of the most formidable challenges in modern immunology. The virus's exceptional genetic diversity, rapid mutation rate, and sophisticated immune evasion tactics have necessitated novel vaccine strategies that move beyond traditional empirical approaches [1] [22]. Among the most promising advanced strategies are germline-targeting and lineage-based vaccine approaches, which aim to guide the immune system through a predefined series of maturation steps to elicit broadly neutralizing antibodies (bNAbs) [1] [11] [14]. These bNAbs are crucial as they target conserved regions of the HIV envelope glycoprotein (Env), enabling them to neutralize a broad spectrum of viral variants [11] [22]. While both strategies share the ultimate goal of inducing potent bNAbs, they differ fundamentally in their starting points, design philosophies, and technical requirements. This guide provides a comparative analysis of these platforms, focusing on immunogenicity, neutralization breadth, and effectiveness, supported by quantitative data from recent clinical trials and preclinical studies to inform researchers and drug development professionals.
Comparative Analysis of Vaccine Strategies
Table 1: Core Strategic Comparison between Germline-Targeting and Lineage-Based Vaccine Approaches
| Metric | Germline-Targeting Strategy | Lineage-Based Strategy |
|---|---|---|
| Core Principle | Reverse-engineered immunogens to bind and activate rare naive B cell precursors with bNAb potential [1] [14] | Immunogens designed based on reconstructed historical maturation pathways of known bNAbs from infected individuals [1] [13] |
| Immunogen Design | Structure-based engineering of non-native proteins (e.g., eOD-GT8) to engage germline BCRs [1] [54] | Sequential immunogens with increasing native-like Env trimer structures to guide affinity maturation [1] |
| Target B Cell Status | Naive B cells [14] | Antigen-experienced memory B cells [1] |
| Key Challenge | Engaging extremely rare precursor B cells in the naive repertoire; requires precise priming [1] [54] | Designing a sequence of immunogens that faithfully recapitulates a complex, multi-year natural maturation process [1] [13] |
Table 2: Comparative Immunogenicity and Performance from Clinical Trials
| Vaccine Candidate / Trial | Strategy | Reported Immunogenicity | Neutralization Breadth | Key Findings |
|---|---|---|---|---|
| eOD-GT8 60mer (IAVI G001) [1] [14] | Germline-targeting (VRC01-class) | 35/36 participants (97%) showed desired precursor B cell responses [1] [14] | Priming step only; limited to precursor engagement | Proof-of-concept that designed immunogens can elicit predefined antibodies in humans [14] |
| eOD-GT8 mRNA (IAVI G002) [1] | Germline-targeting (VRC01-class) | Precursor priming at least as effective as protein platform; higher SHM [1] | Priming step only | mRNA platform enhanced somatic hypermutation (SHM) [1] |
| ConM SOSIP.v7 (ACTHIVE-001) [64] | Native-like trimer (germline-agnostic) | Robust strain-specific binding and neutralising antibodies in nearly all vaccinees [64] | Strain-specific (autologous) neutralization; no broad neutralization reported | Post-hoc analysis showed 22- and 6-fold higher neutralization titers in female-born participants after 2nd/3rd vaccination [64] |
| BG505 SOSIP GT1.1 [1] | Germline-targeting (VRC01-class & apex) | Expanded VRC01-class B cells accumulated several bNAb-associated mutations in macaques [1] | Evidence of advancement toward breadth in animal models [1] | Antibodies elicited were substantially advanced on the path toward becoming bNAbs [1] |
Experimental Protocols and Methodologies
Germline-Targeting Immunogen Design and Testing
The development of germline-targeting immunogens relies on a multi-stage experimental pipeline combining computational design, structural biology, and stringent pre-clinical validation [54]. A key example is the design of epitope scaffolds to elicit 10E8-class bnAbs targeting the membrane-proximal external region (MPER) of gp41, a highly conserved epitope [54].
Key Experimental Workflow:
- Computational Design and Structural Mimicry: Researchers developed germline-targeting epitope scaffolds with affinity for 10E8-class precursors. These scaffolds were engineered to maintain the structural conformation of the 10E8 epitope while being optimized for high-affinity binding to precursor B cell receptors (BCRs) [54].
- Multivalent Nanoparticle Engineering: To enhance B cell activation, these epitope scaffolds were displayed on protein nanoparticles or encoded by mRNA within lipid nanoparticles (LNPs). This multivalent presentation effectively cross-links BCRs on rare precursor cells, a critical signal for activation [54].
- Ex vivo Validation: The engineered immunogens were first tested for their ability to bind bnAb-precursor human naive B cells using ex vivo human B cell screens [54].
- In vivo Animal Immunization: Immunogens that passed ex vivo screening were used to immunize stringent mouse models (e.g., knock-in models with predefined BCR repertoires) and rhesus macaques. The readout was the successful activation and expansion of rare bnAb-precursor B cells with the predefined binding specificities and long HCDR3 features characteristic of 10E8-class bnAbs [54].
Assessing Lineage Development and Maturation
For both germline-targeting and lineage-based approaches, a critical goal of sequential immunization is to guide B cells along a desired maturation path. This requires sophisticated monitoring techniques.
- High-Throughput B Cell Repertoire Sequencing: This method involves tracking B cell lineages over time by sequencing the immunoglobulin genes from antigen-specific B cells isolated after each immunization. This allows researchers to map the phylogenetic trees of developing B cell lineages and quantify the accumulation of somatic hypermutations (SHMs) [1].
- Neutralization Assays: The functional outcome of B cell maturation is assessed using panels of diverse HIV pseudoviruses or heterologous Env proteins in in vitro neutralization assays (e.g., TZM-bl cell-based assays) [22] [64]. The percentage of viruses neutralized in such a panel defines the neutralization breadth.
- Biophysical Characterization: Techniques like biolayer interferometry (BLI) are used to measure the affinity of isolated monoclonal antibodies to the target immunogen and native-like Env trimers [1]. Cryo-electron microscopy (Cryo-EM) is employed to visualize the atomic-level interaction between the matured antibodies and the HIV Env trimer, confirming that the antibody binds to the desired conserved epitope [1].
Diagram 1: A comparative workflow of germline-targeting versus lineage-based vaccine strategies.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Technologies for HIV bNAb Vaccine Research
| Reagent / Technology | Function in Research | Example Use Case |
|---|---|---|
| Engineered Priming Immunogens (e.g., eOD-GT8 60mer, N332-GT5) [1] [14] | Designed to bind and activate rare naive B cells expressing specific bNAb precursors. | IAVI G001 and G002 trials used eOD-GT8 to prime VRC01-class precursors [1] [14]. |
| Stabilized Native-like Env Trimers (e.g., SOSIPs, ConM SOSIP.v7) [1] [64] | Serve as boosting immunogens to guide B cell maturation; present multiple bNAb epitopes in a native conformation. | Used in ACTHIVE-001 trial and as components of sequential boosting regimens [1] [64]. |
| mRNA-LNP Platform [1] [65] | Rapidly expresses immunogens in vivo; can enhance immunogenicity and T follicular helper (Tfh) cell responses. | IAVI G002 trial used mRNA-1644; Pfizer-BioNTech COVID-19 vaccine platform [1] [65]. |
| TLR Agonist Adjuvants (e.g., MPLA, 3M-052) [1] [64] | Potentiate immune responses by activating innate immunity via Toll-like Receptors (TLRs). | ConM SOSIP.v7 vaccine was adjuvanted with MPLA in liposomes [64]. |
| Tier 2 Neutralization Panel [22] [64] | Standardized set of diverse, hard-to-neutralize HIV pseudoviruses to rigorously assess neutralization breadth. | Used in ACTHIVE-001 and other trials to measure vaccine-induced antibody breadth [64]. |
The comparative analysis of germline-targeting and lineage-based strategies reveals a complementary rather than competitive landscape. Germline-targeting has demonstrated remarkable success in the initial priming of predefined precursor B cells in humans, a critical first hurdle [1] [14]. Meanwhile, lineage-based approaches and the use of native-like trimers provide a roadmap for the complex maturation journey required to achieve breadth [1] [13]. Current data suggests that neither strategy alone has yet succeeded in inducing broad neutralization in humans, highlighting the immense complexity of the task.
Future HIV vaccine development is likely to see a convergence of these strategies, potentially combined with T-cell-eliciting platforms to create synergistic effects [13]. Preclinical studies in non-human primates have already shown that combining B-cell and T-cell vaccines can provide better protection, even with lower titers of neutralizing antibodies, suggesting T-cell-mediated immunity can control infected cells that escape neutralization [13]. Furthermore, the adoption of agile mRNA platforms for rapid immunogen screening and the careful consideration of subject-specific factors like genetic background and sex [64] will be crucial for designing the effective sequential immunization regimens needed to end the HIV pandemic.
Germline-Targeting Strengths and Limitations in Addressing Complex Pathogens
Germline-targeting represents a structure-based vaccine strategy designed to overcome one of the most significant challenges in developing vaccines against complex pathogens like HIV: the activation and expansion of rare naïve B cells with the potential to develop into broadly neutralizing antibodies (bNAbs) [55] [14]. This approach operates on the principle that the immune system can be strategically guided through a stepwise immunization process using specifically engineered immunogens that sequentially shepherd B cell maturation along predetermined pathways [14] [12]. Unlike traditional empirical vaccine approaches that largely failed to elicit protection against HIV, germline-targeting employs rational immunogen design based on atomic-level structural knowledge of viral proteins and their interactions with bNAbs [55] [1].
The strategy addresses a critical observation from HIV research: while most people infected with HIV develop strain-specific antibodies, only approximately 15% of individuals naturally produce bNAbs, and even then, only after years of chronic infection [14]. This delay occurs because bNAbs require extensive somatic hypermutation to achieve breadth and potency, and their precursor B cells are exceptionally rare in the naïve B cell repertoire [55] [1]. Germline-targeting vaccine designs aim to imitate and accelerate this natural evolutionary process by initiating responses from these rare precursors and then guiding them through sequential maturation steps using a series of booster immunogens with increasing similarity to native viral proteins [2] [12].
Comparative Analysis of Vaccine Strategies
Table 1: Key Characteristics of Major Vaccine Strategies for Complex Pathogens
| Strategy Feature | Germline-Targeting | Mutation-Guided Lineage | Lineage-Agnostic |
|---|---|---|---|
| Primary Approach | Structure-based design to activate rare naïve B cell precursors | Computational reconstruction of bnAb maturation pathways | Engagement of diverse naïve B cells recognizing bnAb targets |
| Immunogen Sequence | Predefined series of distinct immunogens | Immunogens designed to promote key improbable mutations | Sequential heterologous Env trimers |
| B Cell Targeting | Highly specific to precursors with defined genetic signatures | Focused on specific bnAb lineages | Broad engagement of polyclonal repertoire |
| Maturation Guidance | Stepwise shepherding using increasingly native-like immunogens | Emphasis on early acquisition of critical mutations | Affinity maturation focused on conserved epitopes |
| Key Challenges | Requires extensive structural knowledge; genetic restrictions | Limited by completeness of lineage history data | Less control over final antibody specificity |
Table 2: Performance Comparison of Vaccine Strategies in Recent Clinical Trials
| Trial/Study | Strategy | Target | Response Rate | Key Findings |
|---|---|---|---|---|
| IAVI G001 [1] [4] | Germline-targeting | VRC01-class precursors | 35 of 36 participants (97%) | Successful priming of rare naïve B cells; dose effect confounded by IGHV1-2 genotype |
| IAVI G002 [2] | Germline-targeting + heterologous boost | VRC01-class maturation | 17 of 17 participants (100%) | >80% showed "elite" responses with multiple helpful mutations after prime-boost |
| IAVI G003 [2] | Germline-targeting | VRC01-class in African populations | 17 of 18 participants (94%) | Similar immunogenicity across continents; supports global applicability |
| HVTN 133 [14] | MPER-targeting | Membrane Proximal External Region | Majority after 2-3 doses | Neutralized 15% of tier 2 HIV strains; trial halted due to PEG reaction |
Experimental Evidence and Protocols
Key Clinical Trial Designs and Outcomes
The IAVI G001 trial (NCT03547245) served as a critical proof-of-concept for germline-targeting, testing the eOD-GT8 60mer nanoparticle immunogen delivered with AS01B adjuvant [1] [4]. This Phase I trial employed a randomized, placebo-controlled design with 48 participants receiving vaccinations at weeks 0 and 8. The primary endpoint was the activation and expansion of VRC01-class B cells, defined by the use of IGHV1-2*02 or *04 heavy chains and 5-amino acid light chain CDR3 regions [4]. Researchers employed high-throughput B cell sorting and sequencing to quantify precursor frequencies, which reached median frequencies of 0.09% in the low dose group and 0.13% in the high dose group among memory B cells [4]. Subsequent analysis revealed that an observed dose effect was actually confounded by IGHV1-2 genotype distribution, with participants carrying the *02 allele showing significantly higher precursor frequencies regardless of dose level [4].
The IAVI G002 and G003 trials (NCT05001373, NCT05414786) advanced this approach by utilizing mRNA platforms for delivery and introducing heterologous boosting strategies [2]. These trials implemented a prime-boost regimen where the initial eOD-GT8 60mer priming immunogen was followed by a specifically designed booster immunogen (core-g28v2 60mer) [2] [14]. The experimental protocol involved longitudinal blood sampling to track B cell maturation through memory B cell cultures, monoclonal antibody isolation, and detailed characterization using biolayer interferometry, neutralization assays, and cryo-electron microscopy [1] [2]. Remarkably, in G002, all participants receiving both prime and boost developed VRC01-class responses, with over 80% showing "elite" responses characterized by multiple critical mutations associated with bnAb development [2].
Analytical Methodologies for B Cell Repertoire Analysis
Advanced B cell repertoire analysis techniques have been essential for evaluating germline-targeting vaccines. The field has developed standardized pipelines for deep sequencing of immunoglobulin genes from sorted B cell populations, with particular emphasis on IGHV genotyping at nucleotide-level precision [1] [4]. The IAVI G001 trial implemented personalized genotyping using IgM libraries and the germline allele inference tool IgDiscover to determine the exact IGHV1-2 alleles for each participant [4]. This revealed nine different IGHV1-2 genotypes among the 48 participants, consisting of combinations of *02, *04, *05, and *06 alleles, plus the *02_S4953 variant [4].
Researchers quantified B cell responses using unique molecular identifiers (UMIs) during cDNA synthesis to accurately count mRNA molecules and correct for amplification bias [4]. This allowed precise measurement of allele-specific expression frequencies in the naive repertoire, revealing that *02 allele usage was approximately 3.3% compared to just 0.7% for *04 alleles in heterozygous individuals [4]. The analysis further extended to counting unique heavy chain complementarity determining region 3 (HCDR3) sequences within IGHV1-2 mRNAs, providing a measure of the number of unique IGHV1-2 B cells in each personalized library [4]. These sophisticated methodologies enabled the correlation between germline genotype and vaccine response, demonstrating that *02 homozygotes had approximately twice the frequency of allele-specific unique precursors as heterozygotes [4].
Diagram 1: Germline-Targeting Sequential Immunization Workflow
Strengths of Germline-Targeting Approach
Precision B Cell Targeting and Engineering
Germline-targeting demonstrates exceptional precision in B cell activation, enabling researchers to specifically engage rare precursor B cells that constitute as few as 1 in 300,000 naïve B cells [12]. This precision stems from structure-based immunogen designs that incorporate specific epitopes with optimized affinity for the B cell receptors of targeted precursors [55] [14]. The approach has proven highly reproducible across diverse populations, as evidenced by the IAVI G003 trial where the eOD-GT8 60mer primer successfully activated VRC01-class B cells in 94% of African participants, demonstrating comparable efficacy to the North American cohort in G002 [2]. This cross-population consistency is critical for developing globally effective vaccines and suggests that the fundamental immunogenetic elements required for response are distributed across human populations.
The strategy also enables unprecedented control over B cell maturation pathways through carefully designed sequential immunization regimens [2] [14]. The IAVI G002 trial demonstrated that heterologous boosting with a specifically engineered follow-up immunogen (core-g28v2 60mer) could drive VRC01-class B cells toward more mature states, with over 80% of participants developing "elite" responses containing multiple critical mutations associated with bnAb development [2]. This "shepherding" effect represents a significant advancement in vaccine design, moving beyond simple antigen presentation to active guidance of immune responses along predefined trajectories [12]. The modular nature of the approach allows for iterative improvements at each stage of the immunization sequence as new structural and immunological insights emerge.
Platform Versatility and Technological Integration
Germline-targeting has demonstrated remarkable adaptability across vaccine delivery platforms. The successful translation from protein-based formulations in IAVI G001 to mRNA delivery in IAVI G002 and G003 highlights this versatility [1] [2]. The mRNA platform offers particular advantages for germline-targeting applications, including rapid immunogen prototyping and manufacturing flexibility, which accelerates the iterative design-test-redesign cycles essential for optimizing sequential immunization regimens [2]. Notably, the G002 trial found that mRNA delivery not only effectively primed VRC01-class precursors but actually induced greater numbers of mutations in IGHV1-2-using antibodies compared to protein immunization [1], suggesting potential advantages for driving the somatic hypermutation required for bnAb development.
The approach has effectively integrated cutting-edge structural biology techniques with advanced computational immunology and deep sequencing methodologies [1] [4]. This integration enables unprecedented resolution in monitoring vaccine-induced immune responses, right down to tracking individual B cell lineages and their evolutionary trajectories [1] [4]. The incorporation of personalized immunoglobulin genotyping allows researchers to account for individual genetic variation in vaccine response and optimize immunogen designs for population-level coverage [4]. Furthermore, the precise epitope-focused nature of germline-targeting immunogens avoids the induction of many non-neutralizing or strain-specific antibodies that typically dominate responses to conventional vaccines, potentially leading to more efficient focusing of immune responses on conserved vulnerable sites [55] [14].
Limitations and Challenges
Genetic Restrictions and Population Coverage
A significant limitation of germline-targeting approaches is their dependence on specific immunoglobulin gene variants present in the human population [4]. The requirement for particular IGHV alleles was starkly demonstrated in the IAVI G001 trial, where the single non-responder was found to have an IGHV1-2 05/06 genotype lacking the necessary 02 or *04 alleles required for VRC01-class B cell development [4]. Further analysis revealed substantial allelic variation in response potency, with IGHV1-202 alleles associated with approximately 4-fold higher precursor frequencies (3.3% mRNA expression) compared to *04 alleles (0.7% expression) in heterozygous individuals [4]. This genetic restriction poses challenges for universal population coverage, as the necessary alleles may vary in frequency across different ethnic and geographic groups.
The relative rarity of bnAb-precursor B cells in the naive repertoire presents another fundamental challenge [1] [4]. Even in individuals with permissive genotypes, the precursor frequencies for specific bnAb classes remain exceptionally low, creating a competitive disadvantage during immune responses where more abundant B cell specificities may dominate [55] [14]. This challenge was evident in studies targeting the MPER region of gp41, where researchers observed that 10E8 precursor B cells initially migrated to germinal centers but were soon displaced by higher affinity B cell competitors, with only a single MPER precursor clone able to establish long-term germinal center residency and maturation [14]. This germinal center competition creates a bottleneck that may require additional engineering to overcome, possibly through further optimization of immunogen affinity or timing of administration.
Implementation Complexity and Safety Considerations
The multi-step immunization requirement presents substantial practical challenges for clinical development and eventual deployment [14] [12]. Unlike conventional vaccines that often employ simple prime-boost regimens with the same immunogen, germline-targeting requires a series of distinct immunogens that must be administered in precise sequence to properly guide B cell maturation [12]. Each immunogen in the sequence represents a separate pharmaceutical entity that must undergo individual safety testing and manufacturing process development, significantly increasing the complexity and cost of vaccine development [14]. The optimal timing between immunization steps remains unclear, with intervals needing to balance sufficient time for germinal center reactions against practical vaccination schedules.
Safety considerations have emerged in clinical trials, particularly skin reactions observed in the IAVI G002 trial where 18% of participants experienced itching and urticaria, with 10% developing chronic urticaria lasting six weeks or longer [2]. While these reactions were generally manageable with antihistamines and ultimately resolved, they occurred at higher rates than observed with other Moderna mRNA vaccines [2]. Additionally, the HVTN 133 trial evaluating an MPER-targeting immunogen was halted when one participant developed an anaphylactic reaction to the polyethylene glycol (PEG) in the vaccine formulation [14]. These observations highlight the need for continued safety monitoring and potentially reformulating immunogens to improve their tolerability profiles, such as developing PEG-free alternatives [14].
Table 3: Key Research Reagent Solutions for Germline-Targeting Vaccine Development
| Research Reagent | Primary Function | Example Applications |
|---|---|---|
| eOD-GT8 60mer [4] [14] | Priming immunogen for VRC01-class precursors | IAVI G001, G002, G003 trials for initial B cell activation |
| Core-g28v2 60mer [2] [14] | Booster immunogen for VRC01-class maturation | IAVI G002 trial heterologous boost |
| BG505 SOSIP GT1.1 [1] | Native-like trimer for multiple precursor types | Simultaneous targeting of VRC01-class and apex-specific B cells |
| N332-GT5 [14] | Priming immunogen for BG18-class bnAbs | Preclinical studies for glycan-V3 bnAb lineage |
| IGHV Genotyping Tools (e.g., IgDiscover) [4] | Nucleotide-level immunoglobulin allele determination | Participant stratification and response analysis in clinical trials |
| Unique Molecular Identifiers (UMIs) [4] | Accurate B cell frequency quantification | Precursor frequency measurement in naive repertoire |
Diagram 2: B Cell Repertoire Analysis Workflow
Future Directions and Research Applications
The promising results from recent clinical trials have established germline-targeting as a validated framework for addressing complex pathogens, with several clear directions for advancement [2]. Next-generation efforts will focus on expanding the targeted epitopes beyond the CD4-binding site to include additional vulnerable sites such as the V2 apex, V3-glycan patch, fusion peptide, and MPER region [1] [14]. Since HIV vaccine efficacy will likely require targeting multiple independent epitopes to prevent viral escape, researchers are developing complementary germline-targeting immunogens for different bnAb classes that could ultimately be combined in multivalent vaccine regimens [1] [12]. The recent development of N332-GT5 for BG18-class bnAbs and various MPER-targeting immunogens represents progress toward this epitope diversification [14].
Future clinical trials will explore optimized immunization schedules, including dose adjustments, timing intervals, and heterologous boosting sequences [2]. A follow-up study is already planned in South Africa to evaluate the prime-boost approach tested in G002 at a lower dose, building on the "elite" responses observed in the boosted group [2]. Additionally, researchers will investigate strategies to mitigate adverse effects such as urticaria while maintaining immunogenicity [2]. The application of germline-targeting principles to other challenging pathogens beyond HIV represents another exciting frontier, with potential applications for universal influenza vaccines, pan-coronavirus vaccines, and vaccines against other antigenically variable pathogens [6]. The integration of mRNA technology with structure-based immunogen design creates a powerful platform for rapidly responding to emerging viral threats [6] [2].
The demonstrated success in initiating bnAb pathways in humans provides a foundational breakthrough that validates years of basic research in structural immunology and B cell biology [2]. As the field advances, the focus will shift toward refining and optimizing the later stages of the bnAb maturation process, developing improved boosting immunogens, and ultimately demonstrating protective efficacy in large-scale trials [2] [12]. While significant challenges remain, the germline-targeting approach has transformed HIV vaccine development from empirical testing to rational design, creating a systematic pathway toward one of the most elusive goals in modern medicine [2] [14].
Lineage-Based Strategy Effectiveness in Controlling Pandemic Phases
In the continuous battle against rapidly evolving viral pathogens, two sophisticated vaccine strategies have emerged as frontrunners: germline-targeting for viruses like HIV and lineage-based approaches for antigens with substantial diversity like SARS-CoV-2. While germline-targeting aims to guide the immune system through a stepwise process to produce broadly neutralizing antibodies against highly mutable targets, lineage-based strategies adopt a more direct approach by regularly updating vaccine formulations to match currently circulating viral strains. This analysis provides a comprehensive comparison of the lineage-based strategy's effectiveness throughout the COVID-19 pandemic, examining its performance across different viral evolutionary phases and its role within the broader context of advanced vaccine development.
Experimental and Observational Methodologies for Evaluating Lineage-Based Vaccines
Genomic Surveillance and Viral Sequencing: Studies tracking vaccine effectiveness against emerging variants rely on robust genomic surveillance systems. For SARS-CoV-2, this typically involves whole genome sequencing of virus samples from positive cases. The study from Addis Ababa collected nasopharyngeal swabs from participants who tested positive via rapid diagnostic test, with RNA extraction performed using the MagaBio plus Virus DNA/RNA Purification Kit II on a Bio-Rad Automated Extraction System. Reverse transcription quantitative polymerase chain reaction (RT-qPCR) determined Cycle threshold values before sequencing, enabling the identification of specific variants and sub-lineages [66]. Similar methodologies are employed by CDC's IVY network, which conducts central RT-PCR testing at Vanderbilt University Medical Center followed by whole genome sequencing at the University of Michigan [48].
Vaccine Effectiveness (VE) Studies: Test-negative case-control designs have become the standard for evaluating COVID-19 vaccine effectiveness. This approach compares the odds of vaccination between individuals with laboratory-confirmed SARS-CoV-2 infection (case-patients) and those with similar symptoms but negative test results (controls). The VISION network, for instance, analyzes data from electronic health records across 373 emergency departments/urgent care facilities and 241 hospitals, with vaccination status verified through state registries, EHRs, and medical claims [48]. These studies typically estimate VE using odds ratios adjusted for potential confounders such as age, geographic location, and time.
Neutralization Assays: Laboratory-based assessment of vaccine-induced immunity often involves neutralization assays using pseudoviruses or live virus isolates. These assays measure the capacity of serum from vaccinated individuals to prevent viral entry into susceptible cells, providing a correlate of protection. The reduction in neutralization potency against variants like XBB and BA.2.86 is quantified through half-maximal inhibitory dilution (ID50) titers compared to the ancestral strain [67].
Table 1: Key Methodological Approaches in Lineage-Based Vaccine Evaluation
| Method Type | Primary Objective | Key Procedures | Data Outputs |
|---|---|---|---|
| Genomic Surveillance | Track viral evolution and variant prevalence | Whole genome sequencing, phylogenetic analysis | Variant distribution, mutation profiles, lineage prevalence |
| Test-Negative Design | Estimate real-world vaccine effectiveness | Compare vaccination status in test-positive vs test-negative individuals | Vaccine effectiveness (VE) percentages against infection, hospitalization, death |
| Neutralization Assays | Measure functional antibody responses | Pseudovirus or live virus neutralization assays | Neutralization titers, fold-reduction compared to reference strain |
| Cohort Studies | Assess durability of protection | Longitudinal follow-up of vaccinated cohorts | Waning immunity rates, breakthrough infection incidence |
Quantitative Effectiveness of Lineage-Based Vaccines Against SARS-CoV-2 Variants
The lineage-based strategy for COVID-19 vaccines has demonstrated variable effectiveness depending on the specific variant, time since vaccination, and clinical endpoint measured. During the Omicron phase, particularly against the XBB sublineages, monovalent vaccines based on the ancestral strain showed substantially reduced effectiveness. However, updated formulations targeting more recent variants have restored significant protection.
The CDC's interim estimates for the 2024-2025 COVID-19 vaccine formula during September 2024-January 2025 demonstrated 33% effectiveness (95% CI = 28%-38%) against COVID-19-associated emergency department or urgent care visits among adults aged ≥18 years during the first 7-119 days after vaccination [48]. More importantly for public health outcomes, effectiveness against hospitalization was 45%-46% among immunocompetent adults aged ≥65 years, and 40% (95% CI = 21%-54%) for immunocompromised adults in the same age group [48].
Breakthrough infections with Omicron subvariants have been frequently observed despite vaccination. A study in Addis Ababa found the XBB.1.5 lineage was equally prevalent in both vaccinated (47.2%) and unvaccinated (52.8%) individuals, indicating substantial immune evasion [66]. The study also noted that 25% of samples exhibited high viral loads (Ct values 13-15), demonstrating continued transmissibility despite vaccination [66].
Table 2: Lineage-Based Vaccine Effectiveness Against SARS-CoV-2 Variants
| Variant Phase | Vaccine Formulation | VE Against Infection | VE Against Hospitalization | Key Mutations Affecting VE |
|---|---|---|---|---|
| Original & Early VOCs | Ancestral (Wuhan) | 85-95% | >95% | D614G (Clade G) |
| Delta (B.1.617.2) | Ancestral (Wuhan) | 40-80% | 80-90% | L452R, T478K, P681R |
| Omicron BA.1/BA.2 | Ancestral (Wuhan) | 10-40% | 55-80% | G339D, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, S477N, T478K, E484A, Q493R, Q498R, N501Y, Y505H |
| Omicron XBB | Bivalent (BA.4/BA.5) | 20-40% | 50-70% | F486P, F456L, R346T |
| Omicron JN.1/KP.2 | 2024-2025 Monovalent | 30-50% | 40-60% | L455S (JN.1), R346T, F456L, Q493E (KP.2) |
The progression from ancestral to variant-targeted vaccines illustrates the core premise of the lineage-based strategy: regular updates can partially restore protection against evolving viruses. The 2024-2025 formulations targeting JN.1-derived lineages (KP.2 for Moderna and Pfizer; JN.1 for Novavax) represent the ongoing implementation of this approach [67].
Conceptual Workflow of Lineage-Based Vaccine Strategy
The lineage-based approach follows a systematic cycle of surveillance, evaluation, and reformulation, as illustrated in the following workflow:
Comparative Analysis: Germline-Targeting vs. Lineage-Based Strategies
While this analysis focuses on lineage-based approaches, understanding its contrast with germline-targeting strategies provides valuable context for vaccine development professionals. Germline-targeting represents a more complex, multi-step approach designed to overcome the challenge of elicting broadly neutralizing antibodies (bNAbs) against highly mutable pathogens like HIV.
Germline-targeting vaccines utilize a series of specifically engineered immunogens to guide rare B-cell precursors through the maturation pathway required to produce bNAbs. The initial "priming" immunogen (e.g., eOD-GT8 60mer) is designed to activate naive B cells with B-cell receptors capable of developing into bNAb producers [1] [14]. Subsequent "boosting" immunogens (e.g., core-g28v2 60mer) then shepherd these activated B-cells toward broader neutralization capabilities [14]. This approach has shown promise in early clinical trials, with the IAVI G001 trial demonstrating that 35 of 36 participants (97%) generated detectable IgG B cells expressing VRC01-class B cell receptor precursors after two eOD-GT8 immunizations [14].
In contrast, lineage-based vaccines against SARS-CoV-2 employ a more direct approach of regularly updating the vaccine antigen to match currently circulating strains. This strategy has proven effective at reducing severe disease across multiple variant phases but requires continual monitoring and reformulation.
Table 3: Germline-Targeting vs. Lineage-Based Vaccine Strategies
| Parameter | Germline-Targeting Approach | Lineage-Based Approach |
|---|---|---|
| Primary Target Pathogens | HIV (highly variable envelope proteins) | SARS-CoV-2, Influenza (antigenically drifting viruses) |
| Timeframe | Long-term development (years) | Rapid response (months) |
| Key Mechanism | Stepwise B-cell maturation using sequential immunogens | Regular updates to match circulating strain spike proteins |
| Immune Response Goal | Broadly neutralizing antibodies against conserved epitopes | Strain-specific neutralizing antibodies |
| Update Frequency | Fixed regimen once developed | Periodic (annual or as needed) |
| Clinical Trial Status | Early phase (IAVI G001, G002, HVTN 133) | Extensive phase 3 and real-world effectiveness data |
| Advantages | Potential for broad protection, less frequent boosting | Rapid deployment, established regulatory pathway |
| Limitations | Complex development, unproven efficacy in humans | Continuous surveillance needed, chasing evolution |
Implementation of lineage-based vaccine strategies requires specialized reagents and methodologies. The following toolkit outlines critical resources for researchers in this field:
Table 4: Essential Research Reagents for Lineage-Based Vaccine Studies
| Reagent/Resource | Primary Function | Specific Examples | Application Context |
|---|---|---|---|
| Viral Transport Media (VTM) | Preserve specimen integrity during transport | Commercial VTM with protein stabilizers | Clinical sample collection for sequencing |
| RNA Extraction Kits | Nucleic acid purification for sequencing | MagaBio plus Virus DNA/RNA Purification Kit II [66] | RT-qPCR and whole genome sequencing |
| RT-qPCR Assays | Viral detection and quantification | CDC-approved SARS-CoV-2 assays with Ct value determination | Viral load assessment in breakthrough infections |
| Whole Genome Sequencing Platforms | Comprehensive genomic analysis | Illumina, Oxford Nanopore technologies | Variant identification and lineage assignment |
| Pseudovirus Neutralization Assays | Measure neutralizing antibodies without BSL-3 | Lentivirus-based spike pseudotyped particles | Vaccine immunogenicity assessment |
| Protein-Based Serological Assays | Detect binding antibodies to specific antigens | SARS-CoV-2 spike protein ELISA, multiplex immunoassays | Immune response characterization |
| Reference Viral Strains | Standardized controls for assays | BEI Resources reference strains | Assay calibration and cross-study comparisons |
The lineage-based strategy has proven to be an effective approach for controlling the COVID-19 pandemic across multiple variant phases, particularly in preventing severe outcomes like hospitalization despite reduced efficacy against infection with immune-evasive variants like XBB and JN.1. The continued evolution of SARS-CoV-2 underscores the necessity of adaptive vaccination strategies and next-generation vaccine platforms to maintain protection [66] [67].
While lineage-based approaches provide a pragmatic solution for antigens with substantial diversity, they represent one pole in the spectrum of vaccine strategies. Germline-targeting approaches aim for more universal protection but face significant development challenges. Future directions may involve combining elements of both strategies—using lineage-based methods for immediate response while pursuing germline-targeting for longer-term, broader protection. The continuous genomic surveillance and regular vaccine updates that define the lineage-based approach will remain essential tools for managing COVID-19 while research advances on more universal coronavirus vaccine platforms [66] [67].
Methodological Insights from Comparative Vaccine Effectiveness Studies
Vaccine development has evolved from empirical approaches to sophisticated rational design, particularly for challenging pathogens like HIV and rapidly mutating viruses like SARS-CoV-2. Two predominant strategies have emerged: germline-targeting vaccines that aim to initiate rare, precursor B cells and guide their maturation toward broadly neutralizing antibodies, and lineage-based vaccines that target circulating viral strains and are updated periodically based on surveillance data [1]. The former represents a proactive approach designed to elicit broad protection against highly variable pathogens, while the latter embodies a reactive strategy that adapts to viral evolution. Each paradigm employs distinct methodological frameworks for assessing vaccine effectiveness, from controlled clinical trials measuring precise immunological endpoints to real-world observational studies tracking protection against clinical outcomes. This review systematically compares these methodological approaches, their experimental protocols, and the resulting effectiveness data to inform future vaccine development.
Germline-Targeting HIV Vaccine Strategy
Strategic Rationale and Immunogen Design
The germline-targeting approach addresses a fundamental challenge in HIV vaccinology: the rarity of B cell precursors capable of developing into broadly neutralizing antibodies (bNAbs) and the unusual characteristics of these antibodies, which typically require high levels of somatic hypermutation (SHM) to achieve breadth [68] [1]. This strategy involves structure-based reverse engineering of immunogens that can bind to and prime naïve B cells carrying B cell receptors with genetic signatures that have potential to develop into bNAbs against conserved HIV envelope epitopes [1]. The foundational principle is that sequential immunization with specifically designed immunogens can guide these rare B cell lineages through the necessary maturation pathway that naturally occurs only after years of chronic infection in a small subset of individuals [68].
Key methodological considerations in germline-targeting immunogen design include:
- Epitope focusing: Engineering immunogens to expose conserved neutralization epitopes while minimizing immunodominant non-neutralizing regions
- Germline affinity optimization: Enhancing binding to inferred germline antibodies through computational design and in vitro screening
- Multivalent presentation: Utilizing self-assembling nanoparticles to display multiple copies of immunogens for improved B cell activation
Table 1: Key Germline-Targeting HIV Vaccine Candidates in Clinical Development
| Vaccine Candidate | Target Epitope | Platform | Clinical Trial Identifier | Key Findings |
|---|---|---|---|---|
| eOD-GT8 60-mer [68] | CD4-binding site | Recombinant protein nanoparticle + AS01B adjuvant | IAVI G001 (NCT03547245) | 97% (35/36) recipients produced VRC01-class B cell responses; substantial SHM acquired |
| eOD-GT8 60-mer [1] | CD4-binding site | mRNA-LNP | IAVI G002 (NCT05001373), IAVI G003 (NCT05414786) | VRC01-class precursor priming at least as effective as protein platform; greater SHM observed |
| 426 c.Mod.Core [1] | CD4-binding site | Nanoparticle + 3M-052-AF/aluminum hydroxide adjuvants | HVTN 301 (NCT05471076) | 38 monoclonal antibodies isolated; similarities to VRC01 reactivity observed |
| BG505 SOSIP GT1.1 [1] | CD4-binding site & V2 apex | Native-like trimer | Preclinical (macaque study) | Expanded VRC01-class B cells accumulated mutations toward bNAbs after 3 immunizations |
Experimental Protocols and Assessment Methodologies
Clinical evaluation of germline-targeting vaccines employs sophisticated immunological assays to measure the precise B cell responses these vaccines are designed to elicit. The IAVI G001 trial provides a representative methodological framework [68]. This randomized, double-blind, placebo-controlled phase I clinical trial enrolled 48 participants who received two administrations of either placebo, low-dose vaccine, or high-dose vaccine at 8-week intervals. The primary endpoints included safety, tolerability, and specific immunogenicity measures.
Key methodological components included:
- Serological analysis: Measurement of immunoglobulin G antibodies targeting the CD4bs epitope using binding assays
- Memory B cell characterization: Quantification of CD4bs-specific IgG memory B cells in peripheral blood using flow cytometry
- Germinal center monitoring: Assessment of germinal center B cell responses in lymph nodes
- BCR sequencing: Single-cell sorting of CD4bs-specific B cells followed by B cell receptor sequence analysis to identify VRC01-class characteristics
- SHM quantification: Analysis of mutation frequency in immunoglobulin variable regions
These methodologies revealed that the germline-targeting approach successfully activated genetically diverse B cell precursors that shared properties with mature bNAbs and acquired substantial somatic hypermutation—key milestones toward bnAb induction [68].
Lineage-Based COVID-19 Vaccine Strategy
Strategic Rationale and Platform Implementation
Lineage-based vaccine strategies employ a different methodological framework, focusing on regular updates to vaccine formulations that match currently circulating viral variants. This approach has been extensively implemented for COVID-19 vaccines, where mRNA platforms enable rapid adaptation to new SARS-CoV-2 variants [65]. The strategic foundation is that neutralizing antibodies against contemporaneous strains will provide effective protection, even as the virus evolves, though protection may wane over time and require updated formulations [69].
The methodological approach to lineage-based vaccines includes:
- Global variant surveillance: Continuous genomic monitoring to identify emerging variants of concern
- Strain selection: Periodic determination of which variant(s) to include in updated formulations
- Rapid manufacturing: Utilization of flexible platforms like mRNA-LNP for quick production updates
- Real-world effectiveness monitoring: Ongoing assessment of vaccine performance against clinical outcomes
Table 2: Effectiveness of Lineage-Based COVID-19 Vaccines Against Clinical Outcomes
| Vaccine Formulation | Study Design | Population | Effectiveness Against ED/UC Visits | Effectiveness Against Hospitalization | Effectiveness Against Death |
|---|---|---|---|---|---|
| 2024-2025 COVID-19 Vaccine [70] | Observational cohort | U.S. Veterans | 29.3% (95% CI: 19.1-39.2) | 39.2% (95% CI: 21.6-54.5) | 64.0% (95% CI: 23.0-85.8) |
| 2024-2025 COVID-19 Vaccine [69] | Observational cohort | General population | 45.1% at 4 weeks39.1% at 20 weeks | 57.5% at 4 weeks34.0% at 20 weeks | Combined with hospitalization |
| 2024-2025 COVID-19 Vaccine [48] | Test-negative case-control | Adults ≥18 years | 33% (95% CI: 28-38) | 45-46% (immunocompetent adults ≥65) | Not separately reported |
| LP.8.1-adapted 2025-2026 Formula [65] | Phase 3 clinical trial cohort | Adults 65+ and 18-64 with risk conditions | Not reported | Not reported | Not reported |
Experimental Protocols and Assessment Methodologies
Lineage-based vaccine evaluation employs different methodological approaches, focusing predominantly on real-world effectiveness studies and immunobridging trials. The 2024-2025 COVID-19 vaccine studies illustrate these methodologies well [70] [48]. These studies typically use large-scale observational designs rather than placebo-controlled trials, as ethical considerations preclude withholding available vaccines from at-risk populations.
Key methodological components include:
- Test-negative designs: Case-control approaches where individuals presenting with COVID-like illness are tested and classified as cases (positive) or controls (negative), with vaccination status compared between groups
- Electronic health record analysis: Leveraging large healthcare systems like the Veterans Affairs database to assess outcomes in vaccinated versus unvaccinated cohorts
- Immune response correlation: Measuring neutralizing antibody titers against target variants as a surrogate endpoint
- Time-stratified analysis: Assessing waning protection by measuring effectiveness at different intervals post-vaccination
The VISION network methodology provides a representative example [48]. This network incorporates electronic health records from 373 emergency departments/urgent care centers and 241 hospitals across eight states. The analysis includes adults with COVID-like illness who received molecular SARS-CoV-2 testing, with vaccination data ascertained from state immunization registries and electronic health records. Multivariable logistic regression models adjust for potential confounders including age, geographic region, and underlying health conditions.
Comparative Methodological Frameworks
Assessment Endpoints and Outcome Measures
The two vaccine strategies employ fundamentally different assessment methodologies reflective of their distinct goals and stages of development. Germline-targeting HIV vaccines focus on mechanistic immunological endpoints that validate the underlying approach of guiding B cell maturation, while lineage-based COVID-19 vaccines measure clinical outcomes that demonstrate real-world protection.
Table 3: Methodological Comparison of Vaccine Assessment Approaches
| Assessment Dimension | Germline-Targeting HIV Vaccines | Lineage-Based COVID-19 Vaccines |
|---|---|---|
| Primary Endpoints | VRC01-class B cell response rates, SHM levels, bnAb precursor characteristics | Vaccine effectiveness against ED visits, hospitalizations, death |
| Trial Designs | Randomized, placebo-controlled Phase I trials (e.g., IAVI G001) | Observational cohorts, test-negative designs, immunobridging studies |
| Key Assays | B cell sorting, BCR sequencing, binding antibody profiles | Neutralization assays, electronic health record analysis, case ascertainment |
| Timeframe | Years (sequential immunization required) | Months (rapid deployment of updated formulations) |
| Population Sizes | Dozens to hundreds of participants | Tens to hundreds of thousands of participants |
| Regulatory Pathway | Investigational (proof-of-concept focus) | Licensed platform (strain updates) |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 4: Key Research Reagents and Methodologies in Vaccine Assessment
| Reagent/Methodology | Application | Technical Function | Representative Use |
|---|---|---|---|
| eOD-GT8 60-mer immunogen [68] | Germline-targeting priming | Engineered nanoparticle presenting 60 copies of eOD-GT8 to activate VRC01-class B cell precursors | IAVI G001 trial priming immunogen |
| AS01B adjuvant system [68] | Enhancing immune responses to protein subunit vaccines | Liposomal formulation containing two immune enhancers (MPL and QS-21) | Used with eOD-GT8 60-mer in IAVI G001 trial |
| mRNA-LNP platform [1] [65] | Vaccine delivery | Lipid nanoparticles protecting and delivering mRNA encoding target immunogens | Moderna's mRNA-1644 in IAVI G002/G003 trials; Pfizer-BioNTech COVID-19 vaccines |
| Single-cell BCR sequencing [68] | B cell response characterization | High-throughput sequencing of B cell receptors from sorted antigen-specific B cells | Identification of VRC01-class B cells in vaccine recipients |
| Test-negative design [48] | Real-world vaccine effectiveness | Case-control methodology comparing vaccination status between test-positive cases and test-negative controls | VISION network assessment of COVID-19 vaccine effectiveness |
| Biomarker panels for mRNA vaccine efficacy [71] | Predictive biomarker identification | Mechanistic modeling of tumor-immune interactions to identify predictive biomarkers | Computational modeling of optimal conditions for mRNA vaccine efficacy |
The comparative analysis of methodological approaches reveals how vaccine strategy dictates assessment methodology. Germline-targeting vaccines require sophisticated immunological techniques to validate their precise mechanism of action at the B cell level, while lineage-based vaccines employ large-scale observational frameworks to confirm real-world protection against clinical endpoints. Each methodology presents distinct advantages: germline-targeting assessment provides deep mechanistic insights but limited immediate clinical relevance, while lineage-based evaluation offers practical effectiveness data but less insight into long-term immunological development.
Future vaccine development may integrate elements from both approaches—using germline-targeting principles to design broadly protective vaccines while employing lineage-based methodologies for periodic boosting against emerging variants. The methodological frameworks described herein provide complementary tools for this integrated approach, offering both the precision to guide specific immune responses and the scalability to assess population-level protection. As novel vaccine platforms continue to evolve, these comparative methodologies will remain essential for validating both mechanistic action and practical effectiveness across diverse vaccine strategies.
Synthesizing Correlates of Protection Across Different Vaccine Platforms
The development of effective vaccines, particularly against challenging pathogens like HIV, requires a deep understanding of correlates of protection (CoPs)—the measurable immune responses that reliably predict protection against infection or disease. For decades, vaccine development was largely empirical. However, the emergence of novel vaccine platforms and sophisticated immunogen design has transformed the field, enabling a more systematic approach to eliciting precise immune responses. This guide objectively compares the performance of two leading, innovative strategies: germline-targeting and lineage-based vaccine approaches. Both aim to overcome one of the greatest hurdles in vaccinology—inducing broadly neutralizing antibodies (bNAbs) against highly variable viruses like HIV—but they employ distinct mechanistic pathways and thus establish different correlates of protection [1] [5].
The genetic diversity of HIV and its rapid mutation rate have rendered traditional vaccine approaches insufficient. The modest success of the RV144 trial, which demonstrated a 31.2% reduction in infection risk, highlighted the need for strategies that could induce more potent and broad immunity [22] [5]. This has propelled research into structure-based immunogen design. The germline-targeting strategy focuses on priming rare precursor B cells that possess the inherent potential to develop into bNAb-producing lineages. In contrast, the lineage-based strategy aims to guide the affinity maturation process of activated B cells by using a series of immunogens based on the evolutionary pathway of known bNAbs [1]. Understanding the CoPs associated with each strategy—from the initial expansion of antigen-specific B cell precursors to the somatic hypermutation profiles and final antibody breadth—is critical for evaluating their performance and guiding the future of vaccine development against HIV and other intractable pathogens.
Comparative Analysis of Vaccine Strategic Platforms
The table below summarizes the core principles, technological basis, and key immune correlates of the two main advanced vaccine strategies.
Table 1: Platform Comparison: Germline-Targeting vs. Lineage-Based Vaccines
| Feature | Germline-Targeting Strategy | Lineage-Based Strategy |
|---|---|---|
| Core Principle | Structure-based reverse engineering to prime rare naive B cells with bNAb potential [1]. | Guided affinity maturation using immunogens based on the reconstructed history of known bNAbs [1]. |
| Technological Basis | Engineered immunogens (e.g., eOD-GT8, 426c.Mod.Core) with enhanced affinity for germline B cell receptors (BCRs) [1] [4]. | Sequential immunogens designed to select for key improbable mutations required for neutralization breadth [1]. |
| Key Immune Correlates | Expansion and activation of specific precursor B cells (e.g., IGHV1-2*02 using B cells for VRC01-class) [1] [4]. | Somatic hypermutation (SHM) accumulation, particularly of critical mutations; phylogenetic tree diversification [1] [5]. |
| Quantitative Correlates | Frequency of antigen-specific memory B cells (e.g., >0.1% in IAVI G001 trial) [1] [4]. | Affinity maturation metrics, neutralization breadth and potency against heterologous viral panels [1]. |
| Dependence on Human Genetics | High; requires permissive immunoglobulin alleles (e.g., IGHV1-2*02 or *04 for VRC01-class) [4]. | Moderate; depends on the ability of the host immune system to recapitulate a predefined maturation path. |
| Example Candidates | eOD-GT8 60mer, 426c.Mod.Core, BG505 SOSIP GT1.1 [1]. | Strategies utilizing a series of native-like Env trimers to guide maturation [1]. |
Experimental Protocols and Supporting Data
Germline-Targeting Clinical Trials and Immune Profiling
Protocol: IAVI G001 Trial (eOD-GT8 60mer) The IAVI G001 phase 1 clinical trial serves as a foundational protocol for evaluating germline-targeting vaccines. The trial administered the eOD-GT8 60mer immunogen, a self-assembling nanoparticle, with AS01B adjuvant at weeks 0 and 8 to healthy, HIV-negative adults [1] [4]. The key experimental steps for immune monitoring were:
- Blood Sample Collection: Peripheral blood mononuclear cells (PBMCs) were collected from participants at baseline and multiple time points post-vaccination (weeks 4, 8, 10, and 16) [4].
- B Cell Sorting and Repertoire Analysis: Antigen-specific memory B cells were isolated using fluorophore-labeled eOD-GT8 probes. Single-cell RNA sequencing was performed on sorted B cells to obtain paired heavy- and light-chain variable region sequences [1] [4].
- IGHV Genotyping: Personalized immunoglobulin genotyping was conducted for each participant using IgM libraries from PBMCs and the germline allele inference tool IgDiscover. This allowed for nucleotide-level identification of alleles like IGHV1-2*02 and *04 [4].
- Antibody Characterization: Monoclonal antibodies derived from vaccine-induced B cells were expressed and characterized for binding affinity to the immunogen using Biolayer Interferometry (BLI) and for neutralization capacity in in vitro neutralization assays [1].
Data and Outcomes: The trial demonstrated a 97% response rate, with VRC01-class B cells detected in 35 of 36 recipients [1]. The frequency of these B cells among memory B cells reached a median of 0.13% in the high-dose group [4]. A critical finding was the profound impact of human genetic variation. One non-responder lacked the necessary IGHV1-202 or *04 alleles. Furthermore, the IGHV1-202 allele was associated with a ~4-fold higher frequency of naive precursor B cells in the germline repertoire compared to the IGHV1-2*04 allele, directly influencing the magnitude of the vaccine-induced response [4].
Mutation-Guided Lineage Design and Sequential Immunization
Protocol: Mutation-Guided B Cell Lineage Approach This strategy relies on deep sequencing and computational reconstruction of B cell lineages to design boosting immunogens. The general workflow is:
- bNAb Lineage Isolation and Reconstruction: bNAbs are first isolated from individuals with chronic HIV infection. Their B cell receptor ancestors are computationally reconstructed to map the maturation pathway, identifying key "improbable" mutations essential for breadth [1].
- Immunogen Design: A series of immunogens are designed based on intermediate ancestors in the lineage. These immunogens are structurally optimized to bind to and select for B cell clones that have acquired the desired mutations [1].
- Sequential Immunization in Animal Models: Preclinical studies typically involve priming with a germline-targeting immunogen, followed by sequential boosts with the designed ancestor immunogens.
- Longitudinal Immune Monitoring: Serum is collected regularly to monitor the evolution of neutralization breadth. B cells are isolated at endpoints for detailed phylogenetic analysis to confirm that the vaccine-induced lineage recapitulates the desired maturation path [1].
Supporting Preclinical Data: Studies in animal models, such as those presented by Rogier Sanders, show that sequential immunization with native-like trimer immunogens like BG505 SOSIP GT1.1 can lead to the expansion of VRC01-class B cells that accumulate several mutations associated with mature bNAbs, indicating progression along a desired maturation pathway [1].
Table 2: Key Quantitative Correlates from Clinical and Preclinical Studies
| Vaccine Strategy | Trial / Model | Key Quantitative Correlate | Reported Value |
|---|---|---|---|
| Germline-Targeting | IAVI G001 (eOD-GT8) | Frequency of VRC01-class B cells among MBCs [4] | 0.09% - 0.13% (median) |
| Germline-Targeting | IAVI G001 (eOD-GT8) | Precursor frequency in naive repertoire (IGHV1-2*02 vs. *04) [4] | ~3.2% vs. ~0.8% (mRNA expression) |
| Germline-Targeting | HVTN 301 (426c.Mod.Core) | Induction of VRC01-class B cell precursors [1] | 38 monoclonal antibodies isolated & characterized |
| Lineage-Based | Preclinical (BG505 SOSIP GT1.1) | Accumulation of SHMs associated with bNAbs [1] | Substantial mutation accumulation reported |
Visualizing Strategic Workflows and Immune Correlates
The following diagrams illustrate the logical workflows and critical immune correlates for the two vaccine strategies.
The Scientist's Toolkit: Essential Research Reagents
Successful research and development in this field rely on a suite of specialized reagents and technologies. The following table details key materials and their applications in evaluating vaccine-induced immune responses.
Table 3: Essential Research Reagent Solutions for Advanced Vaccine Development
| Research Reagent / Tool | Function & Application | Example Use Case |
|---|---|---|
| Fluorophore-Lagged Antigen Probes | Label antigen baits for sorting antigen-specific B cells from PBMCs via flow cytometry [1]. | Identification of VRC01-class B cells in IAVI G001 using eOD-GT8 probes [1] [4]. |
| Single-Cell B Cell Receptor Sequencing | Provides paired heavy- and light-chain variable region sequences from single B cells for lineage and mutation analysis [1]. | Clonal analysis of vaccine-induced B cells to confirm VRC01-class characteristics and SHM [4]. |
| Biolayer Interferometry (BLI) | Measures real-time binding kinetics (affinity/avidity) between antibodies and antigens [1]. | Characterizing binding affinity of isolated monoclonal antibodies to the immunogen eOD-GT8 [1]. |
| IGHV Genotyping Tools (e.g., IgDiscover) | Infers personal germline immunoglobulin alleles from sequencing data with nucleotide-level precision [4]. | Determining IGHV1-2 allele status of trial participants to link genotype to response [4]. |
| In Vitro Neutralization Assays | Quantifies the potency and breadth of antibodies or serum against a panel of heterologous viral pseudotypes. | Assessing whether vaccine-induced antibodies can neutralize diverse HIV strains [1] [5]. |
| Native-like Env Trimers | Stable, structure-preserved HIV envelope glycoproteins that display bNAb epitopes; used as immunogens or probes [1] [5]. | Boosting immunogens in sequential vaccination regimens (e.g., BG505 SOSIP) [1]. |
The comparative analysis of germline-targeting and lineage-based vaccine strategies reveals a complementary relationship rather than a strict hierarchy. The germline-targeting approach excels at solving the initial problem of activating exceedingly rare B cell precursors, with the frequency of expanded precursor B cells serving as a primary early correlate. Its performance is highly dependent on human genetics, necessitating patient stratification or immunogen designs with broader allelic coverage [4]. The lineage-based approach addresses the subsequent challenge of guiding affinity maturation along a path that leads to breadth, with the accumulation of specific somatic hypermutations and the development of neutralization breadth as its critical correlates.
Current evidence suggests that a synergistic combination of these strategies may be the most promising path forward. A germline-targeting immunogen can serve as a precise primer, while a series of lineage-based boosts shepherd the activated B cell lineage toward becoming broad and potent neutralizers. Future research must focus on refining these strategies, particularly on designing immunogens that can overcome human genetic restrictions and on optimizing the timing and composition of sequential immunization regimens. The correlates of protection defined here will be essential in benchmarking the success of these next-generation vaccines, ultimately bringing us closer to a globally effective HIV vaccine and informing the development of vaccines against other evolving pathogens.
Conclusion
Germline-targeting and lineage-based vaccine strategies represent complementary pillars of next-generation immunology. Germline-targeting offers a promising path to address historically intractable pathogens like HIV by guiding the immune system to produce broadly protective antibodies. In contrast, lineage-based strategies provide a robust framework for managing rapidly evolving viruses such as SARS-CoV-2 through periodic updates. Future directions should focus on refining sequential immunization regimens, improving the durability of responses, and developing cross-reactive vaccines. The integration of insights from both approaches, supported by advanced platforms like mRNA technology, will be crucial for developing versatile, effective vaccines against future pandemic threats. Continued investment in basic science and innovative clinical trial designs is essential to translate these sophisticated strategies into public health tools.
References
- 1. Optimizing human B cell repertoire analyses to interpret ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271457/]
- 2. Two HIV vaccine trials show proof of concept for pathway to ... [https://www.iavi.org/press-release/two-hiv-vaccine-trials-show-proof-of-concept-for-pathway-to-broadly-neutralizing-antibodies/]
- 3. mRNA HIV vaccine clears hurdles in proof-of-concept ... [https://www.bioxconomy.com/modalities/mrna-hiv-vaccine-clears-hurdles-in-proof-of-concept-clinical-trials]
- 4. Human immunoglobulin gene allelic variation impacts ... [https://www.nature.com/articles/s41541-024-00811-5]
- 5. Progress and Challenges in HIV-1 Vaccine Research [https://www.mdpi.com/2076-393X/13/2/148]
- 6. Novel Strategies for Developing Next-Generation Vaccines to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474351/]
- 7. De-risking vaccine development: lessons, challenges, and ... [https://www.nature.com/articles/s41541-025-01211-z]
- 8. B-cell–lineage immunogen design in vaccine development ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3512202/]
- 9. Targeting HIV-1 immune escape mechanisms [https://www.sciencedirect.com/science/article/pii/S0944501325001855]
- 10. Exploring synergies between B- and T-cell vaccine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10881492/]
- 11. Germline-targeting Strategies to Induce bNAbs against HIV-1 [https://pubmed.ncbi.nlm.nih.gov/40511646/]
- 12. A step in the right direction [http://www.iavi.org/iavi-report/a-step-in-the-right-direction/]
- 13. Exploring synergies between B- and T-cell vaccine ... [https://www.nature.com/articles/s41541-024-00818-y]
- 14. Is germline targeting the future of HIV vaccine development? [https://www.aidsmap.com/news/jun-2024/germline-targeting-future-hiv-vaccine-development]
- 15. Simultaneous induction of multiple classes of broadly ... [https://pubmed.ncbi.nlm.nih.gov/41105754/]
- 16. Moving from Empirical to Rational Vaccine Design in the ' ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6789792/]
- 17. Vaccine Development Throughout History - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8386248/]
- 18. Vaccine Adjuvants: From Empirical to a More Rational ... [https://www.xiahepublishing.com/2472-0712/ERHM-2024-00002]
- 19. Strategies For Eliciting Multiple Lineages of Broadly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9227958/]
- 20. Comparative Immunogenicity and Effectiveness of mRNA- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8689763/]
- 21. Rapid evaluation of COVID-19 vaccine effectiveness ... [https://www.nature.com/articles/s41591-022-01877-1]
- 22. Progress and Recent Developments in HIV Vaccine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298520/]
- 23. A first-in-human germline-targeting HIV nanoparticle vaccine ... [https://pubmed.ncbi.nlm.nih.gov/37224227/]
- 24. Comparison of homologous and heterologous vaccination ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1596265/full]
- 25. heterologous prime-boost vaccination: Topics by Science.gov [https://www.science.gov/topicpages/h/heterologous+prime-boost+vaccination]
- 26. Heterologous prime-boost vaccination drives stromal ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597417/full]
- 27. Heterologous mucosal vaccine boosting enhances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574661/]
- 28. Intravenous heterologous prime-boost vaccination ... [https://www.sciencedirect.com/science/article/pii/S2211124723006101]
- 29. Serological insights from SARS-CoV-2 heterologous prime ... [https://www.nature.com/articles/s41598-024-84392-2]
- 30. The Future of mRNA Vaccines: Potential Beyond COVID-19 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179814/]
- 31. mRNA Vaccines vs. Traditional VaccinesClinical Research ... [https://clinicalresearchrva.com/mrna-vaccines-vs-traditional-vaccines-a-scientific-comparison-for-richmonds-clinical-research-community/]
- 32. a comprehensive review of mRNA vaccine technology and ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-025-02645-6]
- 33. mRNA Vaccines: Current Applications and Future Directions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572956/]
- 34. Comparing Moderna's mRNA-1083 and Pfizer's dual-target ... [https://www.nature.com/articles/s41541-025-01145-6]
- 35. SARS-CoV-2 mRNA vaccines sensitize tumours to immune ... [https://www.nature.com/articles/s41586-025-09655-y]
- 36. ESMO 2025: mRNA-based COVID vaccines generate ... [https://www.mdanderson.org/newsroom/research-newsroom/-esmo-2025--mrna-based-covid-vaccines-generate-improved-response.h00-159780390.html]
- 37. Study finds COVID-19 mRNA vaccine sparks immune ... [https://ufhealth.org/news/2025/study-finds-covid-19-mrna-vaccine-sparks-immune-response-to-fight-cancer]
- 38. Types of data requested to inform December 2025 COVID- ... [https://www.who.int/news/item/29-09-2025-types-of-data-requested-to-inform-december-2025-covid-19-vaccine-antigen-composition-deliberations]
- 39. Influenza Vaccine Composition for the 2025-2026 U.S. ... [https://www.fda.gov/vaccines-blood-biologics/influenza-vaccine-composition-2025-2026-us-influenza-season]
- 40. COVID-19 Vaccines (2025-2026 Formula) for Use in the ... [https://www.fda.gov/vaccines-blood-biologics/industry-biologics/covid-19-vaccines-2025-2026-formula-use-united-states-beginning-fall-2025]
- 41. Reproducible and later vaccine strain selection can ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638742/]
- 42. 2025–2026 Flu Season | Influenza (Flu) [https://www.cdc.gov/flu/season/2025-2026.html]
- 43. With an absent CDC and mismatched 'subclade K' flu strain ... [https://www.cidrap.umn.edu/influenza-vaccines/absent-cdc-and-mismatched-subclade-k-flu-strain-experts-face-upcoming-season]
- 44. A new flu virus variant and lagging vaccinations may mean ... [https://www.cnn.com/2025/11/18/health/new-flu-variant-subclade-k]
- 45. Progress and Challenges in HIV-1 Vaccine Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11860913/]
- 46. Staying Up to Date with COVID-19 Vaccines [https://www.cdc.gov/covid/vaccines/stay-up-to-date.html]
- 47. HIV Vaccines [https://www.iavi.org/our-work/hiv-vaccines/]
- 48. Interim Estimates of 2024–2025 COVID-19 Vaccine ... [https://www.cdc.gov/mmwr/volumes/74/wr/mm7406a1.htm]
- 49. Pan-neutralizing, germline-encoded antibodies against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9650492/]
- 50. Comparative Effectiveness of COVID-19 Vaccines in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9973705/]
- 51. A vaccine strategy for inducing broadly neutralizing ... [https://www.nature.com/articles/s41587-024-02289-x]
- 52. Immune counter-evolution: immortalized B cell clones can ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1648717/full]
- 53. for HIV-1 Strategies that... | Nature Reviews Immunology vaccines [https://www.nature.com/articles/s41577-022-00753-w?error=cookies_not_supported&code=0e36fdaf-9518-4949-807e-0ccd8dc4a242]
- 54. Vaccination induces broadly neutralizing antibody ... [https://www.nature.com/articles/s41590-024-01833-w]
- 55. Germline Targeting Immunogens - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5741082/]
- 56. (PDF) Priming a broadly neutralizing antibody response to HIV-1 using... [https://www.academia.edu/122379386/Priming_a_broadly_neutralizing_antibody_response_to_HIV_1_using_a_germline_targeting_immunogen]
- 57. HIV-1 VACCINES . Priming a broadly neutralizing antibody response to... [https://pubmed.ncbi.nlm.nih.gov/26089355/]
- 58. Effectiveness of 2024–2025 COVID-19 Vaccination Against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12424867/]
- 59. Will Host Genetics Affect the Response to SARS-CoV-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8962369/]
- 60. Influenza B vaccine lineage selection—An optimized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4793086/]
- 61. Germline-targeting HIV vaccination induces neutralizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11783328/]
- 62. Host Genetic Variation Impacts SARS-CoV-2 Vaccination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10821422/]
- 63. HIV broadly neutralizing antibody precursors to the Apex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453070/]
- 64. HIV-1 envelope trimer vaccine induces sex-associated ... [https://www.nature.com/articles/s41467-025-65101-7]
- 65. Pfizer and BioNTech Announce Topline Data ... [https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-announce-topline-data-demonstrating]
- 66. Genome diversity of SARS-CoV-2 lineages associated with... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11107-x]
- 67. Beyond the Pandemic Era: Recent Advances and Efficacy of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031379/]
- 68. First clinical study of germline-targeting strategy: One step closer to a successful bnAb-based HIV vaccine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9898727/]
- 69. New 2025 data shows COVID-19 vaccines provide ... [https://sph.unc.edu/sph-news/new-2025-data-shows-covid-19-vaccines-provide-effective-durable-protection/]
- 70. Association of 2024-2025 Covid-19 Vaccine with ... [https://pubmed.ncbi.nlm.nih.gov/41061231/]
- 71. Biomarkers of mRNA vaccine efficacy derived from ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013163]