Dysregulated Apoptosis in Stage IV Breast Cancer: Biochemical Pathways, Therapeutic Targeting, and Overcoming Treatment Resistance
This article provides a comprehensive analysis of the biochemical processes of apoptosis in stage IV breast cancer, addressing the needs of researchers and drug development professionals.
Dysregulated Apoptosis in Stage IV Breast Cancer: Biochemical Pathways, Therapeutic Targeting, and Overcoming Treatment Resistance
Abstract
This article provides a comprehensive analysis of the biochemical processes of apoptosis in stage IV breast cancer, addressing the needs of researchers and drug development professionals. It explores the foundational science of intrinsic and extrinsic apoptotic pathways, highlighting key players like cytochrome c, caspases, and TP53. The content covers advanced methodological approaches for studying apoptosis, including liquid biopsies and multiplex assays, and investigates major clinical challenges such as therapeutic resistance driven by redox imbalances and defective TP53 signaling. Furthermore, it offers a comparative evaluation of emerging therapeutic strategies that target apoptotic pathways, including novel compounds and nanotechnologies, to overcome resistance in metastatic disease.
Core Apoptotic Machinery in Metastatic Breast Cancer: Deconstructing the Mitochondrial and Death Receptor Pathways
The Central Role of the Mitochondrial (Intrinsic) Pathway and Cytochrome c Release
Within the context of Stage IV breast cancer research, the mitochondrial (intrinsic) pathway of apoptosis represents a critical frontier in understanding treatment resistance and developing novel therapeutic strategies. This in-depth technical guide elucidates the core mechanisms of cytochrome c release, its regulation by the BCL-2 protein family, and the subsequent caspase activation cascade. We synthesize current research findings, present quantitative data from key studies, and provide detailed experimental methodologies for investigating this pathway. The whitepaper further explores the pathway's clinical relevance in advanced breast cancer, including subtype-specific alterations and emerging therapeutic approaches that target mitochondrial apoptosis to overcome treatment resistance in metastatic disease.
Stage IV, or metastatic, breast cancer is characterized by the spread of cancer cells to distant organs, making it notoriously difficult to treat. A hallmark of this advanced disease is the evasion of programmed cell death, or apoptosis, which allows cancer cells to survive despite therapeutic interventions and metabolic stresses. The mitochondrial pathway, also known as the intrinsic pathway, is a principal mechanism of apoptosis initiation in response to cellular damage, oxidative stress, and oncogenic signaling. In breast cancer, the dysregulation of this pathway contributes significantly to treatment resistance and disease progression.
The intrinsic pathway is meticulously regulated by the B-cell lymphoma 2 (BCL-2) family of proteins and centers on mitochondrial outer membrane permeabilization (MOMP), a decisive event leading to the release of cytochrome c and other pro-apoptotic factors from the mitochondrial intermembrane space. Once released into the cytosol, cytochrome c initiates the formation of the apoptosome and activation of caspase proteases, executing the cell death program. Understanding the precise molecular mechanisms governing this pathway provides crucial insights for developing targeted therapies aimed at reactivating apoptosis in treatment-resistant breast cancer cells.
Molecular Mechanisms of the Intrinsic Pathway
Key Regulatory Proteins and Cytochrome c Release
The mitochondrial pathway of apoptosis is rigorously controlled by interactions between pro- and anti-apoptotic members of the BCL-2 protein family. The equilibrium between these proteins determines cellular fate by regulating mitochondrial outer membrane integrity.
BCL-2 Family Proteins: This family comprises three distinct groups based on function and BCL-2 homology (BH) domains. Anti-apoptotic proteins (e.g., BCL-2, BCL-xL) preserve mitochondrial integrity by sequestering pro-apoptotic members. Pro-apoptotic effector proteins (BAX, BAK) directly execute MOMP. BH3-only proteins (e.g., BIM, PUMA, NOXA) act as sentinels that sense cellular stress and initiate apoptosis by neutralizing anti-apoptotic proteins or directly activating BAX/BAK [1].
Mitochondrial Outer Membrane Permeabilization (MOMP): Upon activation by BH3-only proteins, BAX and BAK undergo conformational changes, oligomerize, and integrate into the outer mitochondrial membrane. This process forms macropores that facilitate the release of cytochrome c and other intermembrane space proteins into the cytosol [2] [1]. MOMP propagation through the cytoplasm is regulated by casein kinase II (CK2), representing a critical control point in apoptosis initiation [2].
Cytochrome c Release and Apoptosome Formation: Cytochrome c is a nuclear-encoded hemoprotein located in the mitochondrial intermembrane space, where it functions as an essential electron carrier in the respiratory chain. Its release into the cytosol represents a pivotal commitment to apoptosis. Cytosolic cytochrome c binds to Apaf-1 (apoptotic protease-activating factor 1) in an ATP-dependent manner, forming the heptameric apoptosome complex. This complex recruits and activates procaspase-9, which then cleaves and activates downstream effector caspases-3 and -7, culminating in the systematic dismantling of the cell [3] [4].
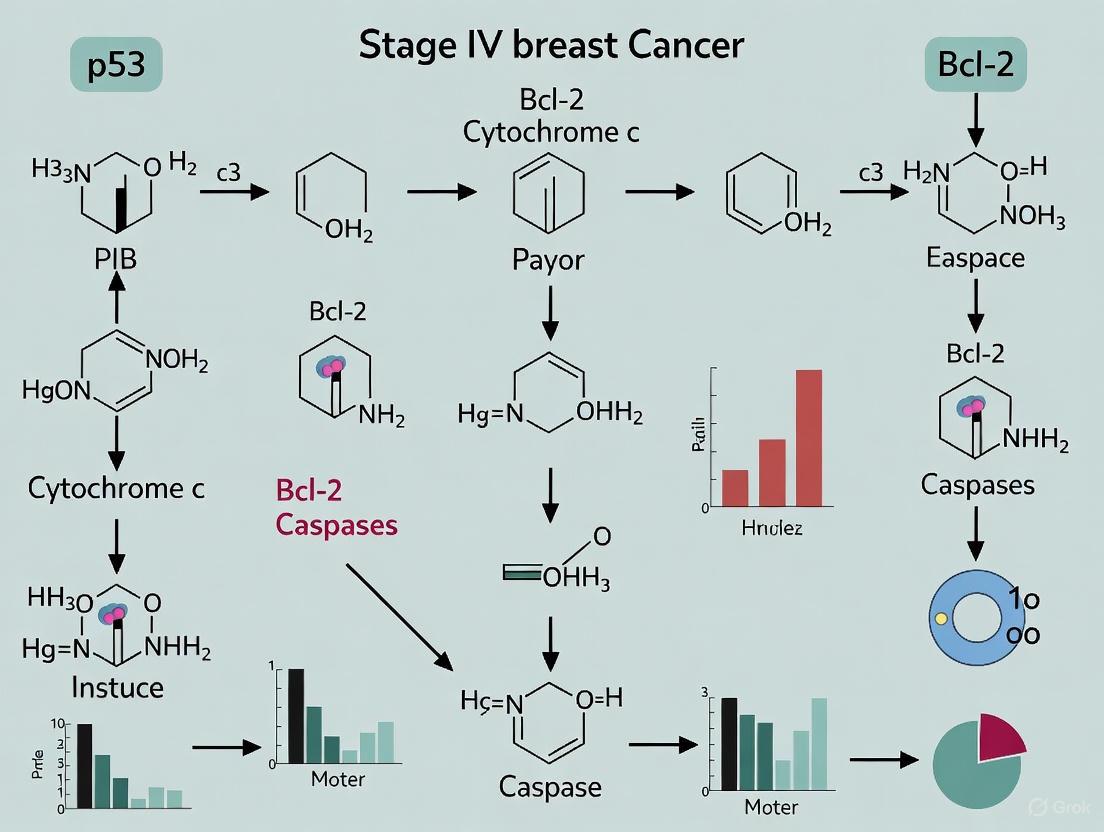
Visualizing the Intrinsic Apoptotic Pathway
The following diagram illustrates the sequential molecular events of the mitochondrial apoptosis pathway, from initial stress signals to caspase activation.
Quantitative Analysis of Pathway Activation
Experimental Findings in Breast Cancer Models
Research across various breast cancer models has quantified the activation of the intrinsic pathway following different treatments. The table below summarizes key quantitative findings from recent studies.
Table 1: Quantitative Measures of Intrinsic Pathway Activation in Breast Cancer Models
| Cell Line / Model | Treatment/Intervention | Key Apoptotic Markers Measured | Quantitative Findings | Citation |
|---|---|---|---|---|
| MCF-7 (ER+) | Scrophularia variegata extract (48h) | Caspase-3, Caspase-9 | Significant dose-dependent increase in caspase-3 and caspase-9 activity. | [5] |
| MDA-MB-231 (TNBC) | Graphene Oxide (GO) 48h | Caspase-9, Caspase-3/7, Cytochrome c | Increased activation of caspase-9 and caspase-3/7; increased levels of cytosolic cytochrome c. | [6] |
| LTED MCF-7 (Anti-hormone resistant) | 17β-estradiol (E2) | Fas death receptor, Cytochrome c, Bcl-2 | Release of cytochrome c; alterations in Bcl-2 expression. | [7] |
| HER2+ Breast Cancer | Erastin & RSL3 (Ferroptosis inducers) | Lipid peroxidation, GPX4 inhibition | Induction of ferroptosis, a non-apoptotic cell death linked to mitochondrial dysfunction. | [8] |
Biomarkers of Mitochondrial Apoptosis
The activation of the intrinsic pathway can be monitored through specific biochemical biomarkers. The following table outlines critical biomarkers and their significance in detecting and quantifying apoptosis.
Table 2: Key Biomarkers for the Mitochondrial Apoptotic Pathway
| Biomarker | Assay/Method | Biological Significance in Apoptosis | |
|---|---|---|---|
| Cytochrome c Release | Western Blot (cytosolic vs. mitochondrial fractions), Immunofluorescence | Primary trigger for apoptosome formation; commitment point to apoptosis. | [3] [4] |
| Caspase-9 Activation | Colorimetric/Fluorometric Assay, Western Blot (cleaved form) | Initiator caspase of the intrinsic pathway; indicates apoptosome activity. | [5] [3] |
| Caspase-3/7 Activation | Colorimetric/Fluorometric Assay, Western Blot (cleaved form), FAM-DEVD-FMK Assay | Key executioner caspases; definitive markers of ongoing apoptosis. | [3] [6] |
| BAX/BAK Oligomerization | Cross-linking + Western Blot, Proximity Ligation Assay | Direct evidence of pro-apoptotic effector protein activation at mitochondria. | [1] |
| Mitochondrial Membrane Potential (ΔΨm) JC-1, TMRM staining, Flow Cytometry | Early event in intrinsic apoptosis; indicates loss of mitochondrial health. | [6] | |
| Phosphatidylserine Externalization | Annexin V-FITC/PI Staining, Flow Cytometry | Mid-stage marker of apoptosis; loss of plasma membrane asymmetry. | [5] [6] |
Detailed Experimental Protocols
Protocol 1: Detecting Cytochrome c Release via Western Blot
This protocol is adapted from methodologies used in recent studies to assess cytochrome c translocation from mitochondria to the cytosol [5] [6].
Principle: Following MOMP, cytochrome c is released into the cytosol. Cellular fractionation separates the cytosolic component from mitochondria, allowing for the specific detection of released cytochrome c by immunoblotting.
Reagents Required:
- Cell Lysis Buffer: 20 mM HEPES (pH 7.5), 10 mM KCl, 1.5 mM MgCl2, 1 mM EDTA, 1 mM EGTA, 250 mM sucrose, supplemented with protease inhibitors.
- Digitonin (for gentle plasma membrane permeabilization)
- Mitochondrial Lysis Buffer: RIPA Buffer
- Antibodies: Anti-cytochrome c antibody, Anti-COX IV antibody (mitochondrial loading control), Anti-β-tubulin antibody (cytosolic loading control).
Procedure:
- Harvesting: Collect treated and control cells (e.g., 5 x 10^6 cells) by trypsinization and centrifugation.
- Plasma Membrane Permeabilization: Wash cell pellet with ice-cold PBS. Resuspend pellet in 1 mL of Cell Lysis Buffer containing 0.015% digitonin. Incubate on ice for 10 minutes with gentle agitation.
- Cytosolic Fraction Isolation: Centrifuge the lysate at 10,000 x g for 5 minutes at 4°C. Carefully transfer the supernatant (cytosolic fraction) to a new pre-chilled microcentrifuge tube.
- Mitochondrial Fraction Isolation: Wash the remaining pellet (containing intact mitochondria) with ice-cold PBS. Lyse the mitochondrial pellet in 100 μL of Mitochondrial Lysis Buffer for 30 minutes on ice. Centrifuge at 12,000 x g for 15 minutes at 4°C to remove insoluble debris. Collect the supernatant (mitochondrial fraction).
- Protein Quantification and Western Blot: Determine protein concentration of both fractions using a BCA assay. Load equal amounts of protein (e.g., 20-30 μg) from cytosolic and mitochondrial fractions onto an SDS-PAGE gel. Transfer to a PVDF membrane and probe with anti-cytochrome c antibody. Use COX IV as a marker for the mitochondrial fraction and β-tubulin for the cytosolic fraction to confirm fractionation purity.
Expected Outcome: In healthy cells, cytochrome c is localized exclusively in the mitochondrial fraction. In apoptotic cells, a significant increase in cytochrome c signal will be observed in the cytosolic fraction.
Protocol 2: Caspase Activity Assay
This protocol details the measurement of caspase-9 and caspase-3/7 activity using fluorometric substrates, a common technique in apoptosis research [5] [6].
Principle: Activated caspases cleave specific peptide sequences. The cleavage of a synthetic substrate conjugated to a fluorophore (e.g., AFC or AMC) releases the fluorophore, generating a fluorescent signal proportional to caspase activity.
Reagents Required:
- Caspase Lysis Buffer
- Substrates: LEHD-AFC (for Caspase-9), DEVD-AFC (for Caspase-3/7)
- Fluorometer or fluorescence-capable plate reader
Procedure:
- Lysate Preparation: Lyse treated and control cells in Caspase Lysis Buffer for 30 minutes on ice. Clarify by centrifugation at 12,000 x g for 15 minutes at 4°C.
- Reaction Setup: In a 96-well plate, combine 50 μg of total protein lysate with 200 μL of reaction buffer containing 50 μM of the respective substrate (LEHD-AFC or DEVD-AFC).
- Incubation and Measurement: Incubate the reaction mixture at 37°C for 1-2 hours. Measure the fluorescence (excitation ~400 nm, emission ~505 nm) at regular intervals.
- Data Analysis: Calculate caspase activity as the change in fluorescence per unit time, normalized to the protein concentration and control sample readings.
Expected Outcome: Cells undergoing intrinsic apoptosis will show a significant, time- and dose-dependent increase in fluorescence for both caspase-9 and caspase-3/7 compared to untreated controls.
Visualizing the Experimental Workflow
The following diagram outlines the core experimental workflow for investigating the mitochondrial pathway of apoptosis, from cell treatment to key readouts.
The Scientist's Toolkit: Key Research Reagents
Successful investigation of the mitochondrial pathway requires a suite of specific reagents and tools. The following table catalogs essential research solutions for studying intrinsic apoptosis.
Table 3: Essential Research Reagents for Investigating the Mitochondrial Pathway
| Reagent / Assay Kit | Vendor Examples | Specific Function in Apoptosis Research | |
|---|---|---|---|
| FITC Annexin V / PI Apoptosis Detection Kit | BD Pharmingen | Differentiates between live (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), and late apoptotic/necrotic (Annexin V+/PI+) cells by detecting phosphatidylserine externalization and membrane integrity. | [5] [6] |
| JC-1 MitoScreen Kit | BD Pharmingen | Measures mitochondrial membrane potential (ΔΨm). Healthy mitochondria show red J-aggregates; depolarized mitochondria show green monomeric fluorescence. | [6] |
| FAM-FLICA Caspase Assays | ImmunoChemistry Technologies | Uses fluorescently labeled inhibitors of caspases (FLICA) that covalently bind to active caspase enzymes, allowing detection via flow cytometry or fluorescence microscopy. | [6] |
| Caspase Colorimetric Assay Kits | R&D Systems, Abcam | Utilizes specific peptide substrates (e.g., DEVD-pNA for caspase-3) linked to a chromophore p-nitroaniline (pNA). Cleavage releases pNA, measurable by spectrophotometry. | [5] |
| BCA Protein Assay Kit | Thermo Scientific | Accurately determines protein concentration in cell lysates, essential for normalizing data in Western blot and enzymatic activity assays. | [6] |
| Anti-Cytochrome c Antibody | Cell Signaling Technology | Detects cytochrome c release in fractionation studies or its subcellular localization via immunofluorescence. | [6] |
| Anti-BCL-2 Family Antibodies | Cell Signaling Technology, Santa Cruz Biotechnology | A panel of antibodies is required to assess the expression levels and conformational states of pro- and anti-apoptotic BCL-2 family proteins. | [7] [1] |
| N-acetylcysteine (NAC) | Merck | A common antioxidant used to investigate the role of oxidative stress in triggering the intrinsic pathway, as it scavenges reactive oxygen species (ROS). | [6] |
Clinical Implications and Therapeutic Targeting
The mitochondrial apoptotic pathway is a major focus for therapeutic innovation in Stage IV breast cancer. Its core components represent promising targets for overcoming treatment resistance.
BCL-2 Inhibition: Venetoclax, a selective BCL-2 inhibitor, has shown efficacy in hematological malignancies and is under investigation for breast cancer, particularly in combination with other agents to sensitize resistant cells [1]. By blocking the pro-survival function of BCL-2, these "BH3 mimetics" free up activators like BIM to trigger BAX/BAK-mediated apoptosis.
Targeting Mitochondrial Metabolism: The recognition of metabolic reprogramming in cancer has shifted attention to mitochondrial vulnerabilities. Drugs that inhibit oxidative phosphorylation or disrupt mitochondrial membrane potential are being explored to selectively eliminate cancer cells, especially those reliant on mitochondrial energy production [2].
Subtype-Specific Strategies: The regulatory dynamics of the intrinsic pathway vary between breast cancer subtypes. In HER2-positive breast cancer, combinations of HER2 inhibitors with pro-apoptotic agents can enhance ferroptosis sensitivity [8]. In estrogen receptor-positive (ER+) cancers that have developed resistance to anti-estrogens, high-dose estrogen can paradoxically induce apoptosis via the intrinsic pathway, a process involving Fas death receptors and cytochrome c release [7].
Novel Inducers: Research into natural compounds and nanomaterials continues to identify new activators of the mitochondrial pathway. For instance, Scrophularia variegata extract and graphene oxide have demonstrated the ability to induce caspase-9-dependent apoptosis in breast cancer cell lines, offering new avenues for drug development [5] [6].
Understanding and targeting the mitochondrial pathway of apoptosis remains a cornerstone of oncological research. As techniques for probing mitochondrial biology advance and novel therapeutic agents continue to be developed, reactivating this fundamental cell death process holds significant promise for improving outcomes in patients with advanced breast cancer.
Death Receptor (Extrinsic) Signaling and Caspase-8 Activation Cascades
In the context of stage IV breast cancer, the dysregulation of programmed cell death (PCD) represents a fundamental mechanism underlying both tumor progression and therapeutic resistance. The extrinsic apoptosis pathway, initiated by extracellular death ligands, constitutes a critical surveillance mechanism that can be harnessed for therapeutic intervention. Caspase-8, an initiator caspase within this pathway, serves as the molecular gatekeeper of extrinsic apoptosis, integrating death signals from the tumor microenvironment and initiating a proteolytic cascade that culminates in cellular dismantling [9] [10]. In breast malignancies, particularly those exhibiting resistance to conventional therapies, understanding the precise molecular architecture of caspase-8 activation provides crucial insights for developing novel treatment strategies. This technical guide delineates the core mechanisms of death receptor signaling and caspase-8 activation cascades, with specific emphasis on their implications for advanced breast cancer research and drug development.
Molecular Architecture of Death Receptor Signaling
Core Components of the Death-Inducing Signaling Complex (DISC)
The extrinsic apoptosis pathway initiates at the plasma membrane, where ligand-mediated trimerization of death receptors (DRs) such as FAS, TNFR1, DR4, and DR5 recruits adapter proteins and procaspases into a multimolecular complex known as the Death-Inducing Signaling Complex (DISC) [9] [11]. The assembly proceeds through highly specific domain interactions:
- Death Domain (DD) Interactions: The homotypic interaction between the death domains of activated death receptors and the adapter protein FADD (Fas-Associated protein with Death Domain) [11].
- Death Effector Domain (DED) Interactions: FADD subsequently recruits procaspase-8 via homotypic DED interactions, forming the core DISC structure [9] [11].
Table 1: Core Components of the Death-Inducing Signaling Complex (DISC)
| Component | Structure | Function in DISC | Regulatory Factors |
|---|---|---|---|
| Death Receptors | Transmembrane proteins with extracellular ligand-binding domains and intracellular death domains | Receptor for extracellular death ligands (e.g., FasL, TRAIL); initiates DISC assembly | Membrane localization, ligand availability, receptor mutations |
| FADD | Adapter protein containing death domain and death effector domain | Bridges death receptors and procaspase-8 via domain interactions | Phosphorylation status, cellular localization |
| Procaspase-8 | Zymogen with two N-terminal DEDs and C-terminal protease domain | Initiator caspase activated within DISC; triggers downstream apoptotic cascade | c-FLIP isoforms, phosphorylation at tyrosine 380 |
| c-FLIP | Catalytically inactive homolog of caspase-8 | Modulates caspase-8 activation; anti-apoptotic at high concentrations, pro-apoptotic at low concentrations | Expression levels, isoform ratio (c-FLIPL vs c-FLIPS) |
Mechanisms of Caspase-8 Activation
Within the DISC, procaspase-8 activation occurs through a meticulously orchestrated process involving proximity-induced dimerization and interdomain autoproteolysis. Recent structural biology insights have revealed that caspase-8 activation requires the formation of specific oligomeric structures termed DED filaments [9]. The activation mechanism proceeds through distinct steps:
- Induced Proximity: DISC assembly brings multiple procaspase-8 molecules into close proximity, facilitating their interaction [9].
- Dimerization and Trans-autocatalytic cleavage: Procaspase-8 molecules form homodimers, undergoing trans-autocatalytic cleavage at specific aspartic residues between the large (p18) and small (p10) subunits [11].
- Maturation: The fully processed caspase-8 heterotetramer (p18₂-p10₂) is released into the cytosol as the active enzyme [9] [12].
Critical to this process is the regulatory influence of c-FLIP (cellular FLICE-inhibitory protein), which exists in long (c-FLIPL) and short (c-FLIPS) isoforms. c-FLIPL can form heterodimers with procaspase-8, exhibiting a dual function: at low concentrations, it enhances caspase-8 activation, while at high concentrations, it inhibits apoptosis. In contrast, c-FLIPS primarily exerts anti-apoptotic effects by competitively inhibiting procaspase-8 recruitment to the DISC [11].
Figure 1: Death Receptor Signaling and Caspase-8 Activation Cascade. The diagram illustrates the sequential molecular events from death ligand binding through caspase-8 activation to downstream apoptotic execution.
Caspase-8 in Breast Cancer: Therapeutic Implications and Resistance Mechanisms
Subcellular Localization and Compartmentalization of Activity
Spatiotemporal regulation of caspase-8 activity represents a critical layer of control in apoptotic signaling. Advanced imaging techniques utilizing FRET-based biosensors and localization probes have demonstrated that caspase-8 exhibits significantly higher proteolytic activity at the plasma membrane compared to the cytosol following CD95 activation [12]. This compartmentalization is governed by cleavage of the caspase-8 prodomain, with the fully processed form being released into the cytosol. This spatial regulation may serve to restrict enzymatic activity prior to mitochondrial pathway engagement, thereby functioning as a safeguard against inadvertent apoptosis induction [12]. In breast cancer cells, manipulation of this subcellular localization – such as targeting caspase-8 substrates to the plasma membrane – can significantly accelerate cell death, suggesting potential therapeutic avenues for overcoming resistance [12].
Resistance Mechanisms in Breast Cancer
Therapeutic resistance in stage IV breast cancer frequently involves disruption of extrinsic apoptosis signaling through multiple molecular mechanisms:
- c-FLIP Overexpression: Elevated expression of c-FLIP, particularly the c-FLIPS isoform, competitively inhibits procaspase-8 recruitment to the DISC, effectively blocking initiation of the apoptotic cascade [11].
- Epigenetic Modifications: Aberrant DNA methylation and histone modifications can reprogram gene expression networks, suppressing pro-apoptotic genes while enhancing anti-apoptotic pathways [13].
- Receptor Mutations and Downregulation: Genetic alterations in death receptors or decreased surface expression limit ligand binding and DISC assembly [13].
- Caspase-8 Mutations: While relatively rare, functional mutations in caspase-8 can impair its proteolytic activity or recruitment to the DISC [9].
Table 2: Caspase-8-Mediated Apoptosis Assays and Their Application in Breast Cancer Research
| Assay Method | Target Readout | Application in Breast Cancer Research | Technical Considerations |
|---|---|---|---|
| FRET-Based Biosensors | Caspase-8 activation kinetics in single living cells | Quantitative analysis of spatiotemporal caspase-8 dynamics; drug screening | High sensitivity for minute caspase dynamics; requires specialized equipment [14] |
| Annexin V/PI Staining | Phosphatidylserine externalization (early apoptosis) and membrane integrity | Detection of early apoptotic events in response to therapeutic agents; combination with death receptor agonists | Distinguishes early apoptosis (Annexin V+/PI-) from late apoptosis/necrosis (Annexin V+/PI+); flow cytometry or microscopy [15] [10] |
| TUNEL Assay | DNA fragmentation (late apoptosis) | Confirmation of apoptotic cell death in tumor specimens and cell cultures | Robust detection but not apoptosis-specific; requires morphological correlation [15] [10] |
| Caspase Activity Assays | Caspase-8, -3/7, -9 proteolytic activity | Mechanistic studies of apoptotic pathways activated by novel therapeutics | Luminescent (Caspase-Glo) or colorimetric substrates; can be adapted for high-throughput screening [15] [16] |
| Western Blot Analysis | Caspase-8 processing and cleavage of substrates | Verification of caspase-8 activation and downstream signaling | Detects procaspase-8 cleavage and appearance of active fragments; can assess BID cleavage [15] |
Quantitative Analysis and Mathematical Modeling of Caspase-8 Function
Mathematical modeling has emerged as a powerful tool for elucidating the quantitative aspects of caspase-8 function within apoptotic signaling networks. Computational approaches based on mass-conservation principles and kinetic rate laws have been employed to formulate ordinary differential equations describing the temporal evolution of caspase activation [17]. These models have yielded critical insights, including:
- Prediction of the minimal concentration of caspase-8 required to initiate apoptotic signaling [14].
- Identification of threshold mechanisms in CD95-induced apoptosis [9].
- Simulation of qualitative strategies for preventing caspase activation, with potential applications in therapeutic development [17].
Quantitative experimental validation of mathematical models using high-sensitivity FRET-based biosensors has enabled researchers to redefine the kinetics, dynamics, and selectivity in apoptotic signaling pathways following caspase-8 activation [14]. These integrated computational-experimental approaches are particularly valuable for understanding the heterogeneous responses to death receptor targeting therapies in breast cancer populations.
Experimental Approaches for Investigating Caspase-8 Signaling in Breast Cancer
Establishing Model Systems for Therapeutic Screening
Multiple experimental approaches have been developed to investigate caspase-8-mediated apoptosis in breast cancer models:
Cell Line Models: Breast cancer cell lines with distinct molecular subtypes (e.g., T-47D, MCF-7, MDA-MB-231) provide platforms for evaluating subtype-specific apoptotic responses [15] [16]. For instance, studies with T-47D cells have demonstrated caspase-8 activation following treatment with Vitex rotundifolia fractions, indicating engagement of the extrinsic pathway [15].
Compound Screening: Natural products and derived compounds represent valuable tools for probing death receptor pathways. Black turtle bean extracts have shown efficacy in activating caspase-8 and inducing apoptosis through both extrinsic and intrinsic pathways in MCF-7 and MDA-MB-231 cells [16]. Similarly, Vitex rotundifolia fractions F2 and F3 triggered apoptotic cell death in T-47D cells via activation of caspases-8, -9 and -3/7, accompanied by Bax upregulation and Bcl-2 downregulation [15].
Methodological Framework for DISC Analysis
Comprehensive analysis of DISC composition and function employs a multidisciplinary approach:
- Immunoprecipitation: Isolation of native DISC complexes following receptor activation using receptor-specific antibodies [9].
- Western Blotting: Identification of DISC components (FADD, caspase-8, c-FLIP) and assessment of caspase-8 processing [9] [15].
- Quantitative Proteomics: Stoichiometric analysis of DISC composition, revealing precise molecular ratios within the complex [9].
- Structural Biology Techniques: Cryo-EM studies have elucidated the architecture of caspase-8 tandem DED filaments, providing insights into assembly and regulation mechanisms of the DISC [9].
Figure 2: Experimental Workflow for Analyzing Caspase-8-Mediated Apoptosis in Breast Cancer Models. The diagram outlines the key steps from therapeutic intervention through apoptotic signaling to analytical measurement.
The Scientist's Toolkit: Essential Reagents and Methodologies
Table 3: Research Reagent Solutions for Studying Death Receptor Signaling
| Reagent/Category | Specific Examples | Research Application | Experimental Notes |
|---|---|---|---|
| Death Receptor Agonists | Recombinant TRAIL, FasL, Agonistic antibodies (e.g., anti-DR5) | Direct activation of extrinsic apoptosis pathway; screening for sensitizing agents | Can exhibit cell type-specific toxicity; often used in combination therapies |
| Caspase Inhibitors | z-IETD-fmk (caspase-8 inhibitor), z-VAD-fmk (pan-caspase inhibitor) | Mechanistic studies to confirm caspase-8-specific effects; control experiments | Potential off-target effects at higher concentrations; use appropriate controls [14] |
| Natural Product Extracts | Vitex rotundifolia fractions, Black turtle bean (BTB) extracts | Screening for novel apoptosis-inducing compounds; combination therapy approaches | Standardized extraction and characterization essential for reproducibility [15] [16] |
| Apoptosis Detection Kits | Annexin V-FITC/PI kits, Caspase-Glo assays, TUNEL assay kits | Quantification of apoptotic response; high-throughput screening | Multiparametric analysis recommended for conclusive apoptosis assessment [15] [10] |
| Cell Line Models | T-47D, MCF-7, MDA-MB-231, BT-474 | Subtype-specific mechanistic studies; drug screening | Molecular characterization essential (receptor status, genetic background) [15] [16] |
| Antibodies for Western Blot | Anti-caspase-8, Anti-FADD, Anti-BID, Anti-cleaved caspase-3 | Analysis of pathway activation and protein processing | Validation of antibody specificity crucial; assess both procaspase and cleaved forms |
Concluding Perspectives and Future Directions
The intricate molecular machinery governing death receptor signaling and caspase-8 activation represents a promising therapeutic frontier in stage IV breast cancer research. As drug development professionals confront the challenges of tumor heterogeneity and treatment resistance, innovative strategies targeting the extrinsic apoptosis pathway continue to emerge. Future directions include the development of direct caspase-8 activators, c-FLIP antagonists, combinatorial regimens that sensitize tumor cells to death receptor engagement, and integration with immunotherapeutic approaches. The continued elucidation of caspase-8's non-apoptotic functions in inflammation, necroptosis regulation, and immune modulation further expands its therapeutic relevance [11]. As research advances, leveraging the precise mechanistic understanding of caspase-8 activation cascades will undoubtedly yield novel therapeutic opportunities for overcoming treatment resistance in advanced breast cancer.
In stage IV breast cancer, the dysregulation of programmed cell death (apoptosis) is a critical mechanism enabling tumor survival, progression, and resistance to therapy. Two central regulators of this process are the BCL-2 family of proteins and the TP53 tumor suppressor. The BCL-2 family governs the mitochondrial (intrinsic) apoptotic pathway, determining cellular commitment to death through complex protein interactions [18]. Meanwhile, the TP53 protein acts as a guardian of the genome, integrating stress signals and deciding whether a cell should repair DNA damage or undergo apoptosis [19]. In advanced breast cancer, both systems are frequently compromised; TP53 is mutated in 20-40% of cases, and anti-apoptotic BCL-2 members like MCL1 are often amplified, leading to therapeutic resistance and disease progression [20] [19]. Understanding the intricate dynamics between these regulatory components is essential for developing novel treatments for metastatic breast cancer.
Core Molecular Mechanisms
The BCL-2 Protein Family: Regulators of Mitochondrial Apoptosis
The BCL-2 protein family constitutes the critical control point for the intrinsic apoptotic pathway, operating through a tightly regulated balance between pro-survival and pro-death signals [18].
- Structural Organization: All BCL-2 family members share homology within up to four BCL-2 homology (BH) domains (BH1-BH4). Anti-apoptotic proteins (e.g., BCL-2, BCL-xL, MCL-1, BCL-w, BCL2-A1) typically contain all four domains, which form a hydrophobic groove for binding pro-apoptotic partners. Pro-apoptotic members are divided into effectors (BAX, BAK) containing BH1-3 domains, and BH3-only proteins (BIM, BID, PUMA, NOXA, BAD, BIK, HRK) that function as initiators [18].
- Mechanism of Mitochondrial Outer Membrane Permeabilization (MOMP): In healthy cells, anti-apoptotic proteins bind and sequester the effectors BAK (resident on mitochondria) and BAX (cytosolic). Upon apoptotic stimuli, BH3-only proteins are activated and engage in two complementary mechanisms: 1) "Direct activation," where activator BH3-only proteins (BIM, tBID, PUMA) bind to and conformationally activate BAX/BAK, and 2) "Derepression," where sensitizer BH3-only proteins (BAD, NOXA, BIK) bind anti-apoptotic proteins, displacing the activators [18]. Activated BAX and BAK oligomerize to form pores in the mitochondrial outer membrane, leading to MOMP and release of cytochrome c, which triggers caspase activation and irreversible cell death [18].
- Cellular Decision Making: The cell's fate hinges on the complex interactions between these three subgroups. The concentration and binding affinities of these proteins create a rheostat system that determines susceptibility to apoptosis [18].
TP53 Tumor Suppressor: Guardian of the Genome
The TP53 tumor suppressor gene encodes the p53 protein, a transcription factor that maintains genomic integrity by responding to diverse cellular stresses, including DNA damage, oncogene activation, and hypoxia [19].
- Normal Function and Activation: In unstressed cells, p53 levels are kept low through continuous degradation mediated by MDM2. Following stress, particularly DNA damage, post-translational modifications stabilize p53. The protein then acts as a sequence-specific transcription factor, binding to target genes and regulating their expression [19]. Its key functions include:
- Cell Cycle Arrest: Transactivation of p21 and other genes to halt the cell cycle and allow time for DNA repair.
- DNA Repair: Activation of DNA repair pathway genes.
- Apoptosis: Induction of pro-apoptotic genes, including members of the BCL-2 family like BAX, PUMA, and NOXA, which promote MOMP [19].
- Integration with Apoptotic Pathways: p53 directly connects DNA damage to the intrinsic apoptotic pathway by transcriptionally upregulating pro-apoptotic BCL-2 family members. It can also promote apoptosis through transcription-independent mechanisms by directly interacting with BCL-2 family proteins at the mitochondria [21].
Table 1: Functional Classification of Key BCL-2 Family Proteins in Breast Cancer
| Protein | Function | Role in Apoptosis | Expression in Breast Cancer |
|---|---|---|---|
| BCL-2 | Anti-apoptotic | Binds and inhibits BAX/BAK activation | Associated with ER+ status, improved survival [21] |
| MCL-1 | Anti-apoptotic | Inhibits BAX/BAK; regulated by multiple pathways | Commonly amplified; associated with therapeutic resistance [20] [18] |
| BCL-xL | Anti-apoptotic | Inhibits BAX/BAK activation | Overexpression linked to high grade and metastasis [22] |
| BAX/BAK | Pro-apoptotic Effector | Forms mitochondrial pores, executes MOMP | Reduced BAX linked to poor chemo response [21] |
| BIM, PUMA | BH3-only Activator | Directly activates BAX/BAK | Critical for apoptosis initiation; regulated by p53 (PUMA) [18] |
| BAD, NOXA | BH3-only Sensitizer | Binds anti-apoptotic proteins, displaces activators | Neutralizes anti-apoptotic proteins, promoting death [18] |
Alterations in Advanced Breast Cancer
TP53 Mutational Spectrum and Clinical Impact
Somatic TP53 mutations occur in 20-40% of breast cancers, making them one of the most frequent genetic events in the disease [19]. These mutations are not uniformly distributed across molecular subtypes; they are most common in triple-negative breast cancer (TNBC) and HER2-positive subtypes, and are associated with more aggressive disease and poorer prognosis [23] [19].
- Mutation Types and Consequences: Most TP53 mutations are missense mutations within the DNA-binding domain (exons 5-8), leading to the production of a full-length but functionally impaired protein. These mutants often lack sequence-specific DNA binding ability and are thus unable to transactivate target genes. Some mutations result in a "gain-of-function" phenotype, where the mutant p53 protein acquires new oncogenic activities that promote tumorigenesis, invasion, and metastasis [23] [24].
- Impact on Treatment Response: Tumors with TP53 mutations are more likely to be resistant to a range of therapies, including certain chemotherapeutic drugs and radiotherapy. This is largely due to the inability to trigger apoptosis in response to treatment-induced DNA damage [19].
- Isoform Complexity: The discovery of p53 isoforms, such as the internally spliced Δp53, adds a layer of regulatory complexity. Δp53 lacks parts of the DNA-binding domain and the nuclear localization signal, resulting in a protein with altered promoter selectivity and transactivation capacity compared to full-length p53. Co-expression of both isoforms occurs in breast tumors, and "mutational hybrid" tumors (with mutated full-length p53 but wild-type Δp53) may have distinct clinical behaviors [24].
Dysregulation of the BCL-2 Family
In breast cancer, the precise balance between pro- and anti-apoptotic BCL-2 family members is disrupted, creating a state where cells are primed for survival despite internal damage or external death signals.
- MCL1 Amplification: MCL1 is the most frequently amplified anti-apoptotic BCL-2 family member in breast cancer, a finding consistently observed in both patient samples and cell line models [20]. Its unique regulation by numerous oncogenic signaling pathways (e.g., PI3K/AKT, MEK/ERK) and its rapid turnover make it a critical survival factor in cancer cells. Basal-like breast cancer cell lines show particular sensitivity to MCL1 inhibition [20] [18].
- Therapeutic Resistance: Overexpression of anti-apoptotic proteins like BCL-2, BCL-xL, and MCL-1 is a established mechanism of resistance to chemotherapy, radiotherapy, and targeted therapies. These proteins effectively neutralize the cell's death machinery, even when treatments successfully activate BH3-only proteins [18] [22]. The ratio of pro-apoptotic to anti-apoptotic proteins, such as the BAX/BCL-2 ratio, is a key determinant of a tumor's apoptotic threshold and treatment sensitivity [21] [22].
Table 2: TP53 Mutation Types and Their Functional Consequences in Breast Cancer
| Mutation Type | Frequency | Molecular Consequence | Impact on p53 Function |
|---|---|---|---|
| Missense | Most Common (~75%) | Single amino acid change, often in DNA-binding domain | Altered conformation, loss of DNA binding; can lead to dominant-negative or gain-of-function effects [23] [19] |
| Nonsense | Less Common | Introduction of premature stop codon | Truncated, unstable protein; complete loss of function (null allele) [24] |
| Frameshift | Less Common | Insertion/deletion causing shift in reading frame | Truncated, dysfunctional protein; complete loss of function [24] |
| Splice Site | Less Common | Disruption of mRNA splicing | Production of abnormal protein isoforms; loss of function [24] |
Diagram 1: TP53 signaling in response to DNA damage. Wild-type p53 activation leads to cell fate decisions, while mutant p53 results in survival and genomic instability.
Experimental Analysis and Methodologies
Quantifying Apoptotic Function in Breast Cancer Models
To study BCL-2 family dynamics and p53 function, researchers employ a suite of biochemical, molecular, and cell-based assays.
BH3 Profiling: This functional assay measures mitochondrial priming—how close a cell is to the apoptotic threshold. Isolated mitochondria or permeabilized cells are exposed to synthetic BH3 peptides that mimic specific BH3-only proteins. The amount of cytochrome c released is quantified, revealing the cell's dependence on specific anti-apoptotic proteins (e.g., sensitivity to HRK peptide indicates BCL-2/BCL-xL dependence, while NOXA sensitivity indicates MCL-1 dependence) [20] [18].
- Protocol Outline:
- Cell Preparation: Isolate tumor cells or use established cell lines.
- Permeabilization: Treat cells with digitonin to create pores in the plasma membrane.
- BH3 Peptide Incubation: Expose permeabilized cells to a panel of BH3 peptides.
- Cytochrome c Detection: After incubation, fix cells and stain with anti-cytochrome c antibody. Measure release via flow cytometry or ELISA.
- Data Analysis: Compare cytochrome c release profiles to determine anti-apoptotic dependencies.
- Protocol Outline:
Analysis of TP53 Mutation Status and Expression:
- DNA Sequencing: The gold standard for identifying TP53 mutations. Sanger or next-generation sequencing of exons 4-9 (the DNA-binding domain) detects the majority of pathogenic mutations [23] [24].
- Immunohistochemistry (IHC): Commonly used as a surrogate for mutation detection. Mutant p53 protein is often stabilized and accumulates to high levels detectable by IHC. However, some mutations (nonsense, frameshift) lead to protein truncation and absence of staining, making interpretation nuanced [21].
- Quantitative RT-PCR for p53 Isoforms: To measure expression of full-length p53 and its isoforms (like Δp53). Specific primers are designed to distinguish between different splice variants. Expression levels can be correlated with clinical parameters and treatment response [24].
Investigating Drug Sensitivities and Dependencies
The Cancer Cell Line Encyclopedia (CCLE) and Genomics of Drug Sensitivity in Cancer (GDSC) platforms provide large-scale resources to correlate molecular aberrations with drug response. Experimental workflow typically involves:
- Cell Line Panel Selection: Utilizing a diverse set of breast cancer cell lines representing different subtypes (Luminal, HER2+, Basal-like) [20].
- Molecular Characterization: Profiling cell lines for genetic alterations (e.g., MCL1 amplification, TP53 mutation) and baseline protein expression [20].
- Viability Assays: Treating cell lines with increasing concentrations of BH3 mimetics (e.g., ABT-199/venetoclax for BCL-2, S63845 for MCL-1) or standard chemotherapies. Cell viability is measured after 72-96 hours using assays like CellTiter-Glo [20].
- Dependency Analysis: Using CRISPR or RNAi screens to identify genes essential for cell survival. Cell lines dependent on MCL1 show marked sensitivity to its genetic knockdown or pharmacological inhibition [20].
Diagram 2: Mechanism of action for BH3 mimetic drugs. These therapeutics displace pro-apoptotic proteins from their anti-apoptotic counterparts, triggering mitochondrial apoptosis.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying Apoptosis in Breast Cancer
| Reagent / Tool | Primary Function | Application in Breast Cancer Research |
|---|---|---|
| BH3 Mimetics (Venetoclax, S63845, A1331852) | Small molecule inhibitors that selectively bind and neutralize specific anti-apoptotic BCL-2 proteins [20]. | Used to determine anti-apoptotic dependencies (e.g., MCL1 vs. BCL-2) in different breast cancer subtypes and to overcome therapeutic resistance [20] [18]. |
| BH3 Profiling Peptides | Synthetic peptides corresponding to the BH3 domains of native BH3-only proteins (e.g., BIM, BAD, HRK, NOXA) [18]. | Functional assay to measure mitochondrial priming and identify which anti-apoptotic protein(s) a tumor cell is dependent on for survival [20]. |
| p53 Pathway Modulators (Nutlins, APR-246) | Nutlins inhibit MDM2 to stabilize p53. APR-246 reactivates mutant p53 and induces oxidative stress [23]. | Investigated as strategies to restore p53 function in wild-type or mutant p53 contexts, respectively, to trigger apoptosis in resistant cells [23]. |
| Cancer Cell Line Encyclopedia (CCLE) | A comprehensive resource of genomic data from ~1000 human cancer cell lines, including breast cancer [20]. | Provides baseline genetic information (mutations, copy number alterations) for selecting relevant models and correlating molecular features with drug response. |
| Genomics of Drug Sensitivity in Cancer (GDSC) | A database of drug sensitivity and molecular markers for a wide panel of cancer cell lines [20]. | Used to identify correlations between BCL-2 family protein expression or TP53 status and sensitivity to various chemotherapeutic and targeted agents. |
Therapeutic Implications and Future Directions
The intricate interplay between BCL-2 family proteins and TP53 presents both challenges and opportunities for treating stage IV breast cancer.
- Targeting Anti-Apoptotic Dependencies: The development of BH3 mimetics has enabled precision targeting of apoptotic pathways. While the BCL-2 inhibitor venetoclax is effective in hematological malignancies, solid tumors like breast cancer often show greater dependence on MCL-1 or BCL-xL. This underscores the need for biomarker-driven patient selection. Basal-like breast cancers, which frequently harbor MCL1 amplifications and express high levels of BIM, may be particularly susceptible to MCL1 inhibitors [20] [18].
- Overcoming TP53-Mediated Resistance: Reactivating mutant p53 or inhibiting its downstream effects is a major therapeutic goal. Compounds like APR-246 (PRIMA-1Met) can refold certain mutant p53 proteins into a functional conformation and have entered clinical trials. Alternatively, targeting downstream effectors common to both wild-type and mutant p53 pathways, such as the pro-apoptotic proteins PUMA or BAX, could bypass the need for functional p53 [23].
- Rational Combination Therapies: Given the complexity of apoptotic regulation, monotherapies are often insufficient. Promising strategies include:
- BCL-2 Inhibition + Endocrine Therapy: Enhancing cell killing in hormone receptor-positive breast cancer.
- MCL1 Inhibition + Chemotherapy: Overcoming chemotherapy resistance conferred by MCL1 upregulation.
- BH3 Mimetics + Targeted Agents: Co-targeting survival pathways (e.g., PI3K/AKT) that regulate MCL-1 stability can synergize to induce apoptosis [20] [18] [22].
- Novel Cell Death Mechanisms: Recent research has identified non-apoptotic programmed cell death pathways like ferroptosis, an iron-dependent form of death driven by lipid peroxidation. Inducing ferroptosis represents a promising strategy to eliminate apoptosis-resistant breast cancer cells, particularly in TNBC, and is an exciting frontier for future drug development [8].
Understanding the dynamic regulation of the BCL-2 family and TP53 tumor suppressor, and their complex interactions in the context of advanced breast cancer, is fundamental to developing more effective, targeted therapies that can overcome treatment resistance and improve outcomes for patients with metastatic disease.
In stage IV breast cancer, the biochemical process of apoptosis is not an isolated event but part of a complex network of regulated cell death (RCD) pathways that interact through sophisticated crosstalk mechanisms. This intricate interplay between different cell death modalities—particularly PANoptosis, autophagy, and ferroptosis—significantly influences tumor progression, therapeutic resistance, and metastatic behavior. The tumor microenvironment (TME), dominated by stromal components like cancer-associated fibroblasts (CAFs), creates a dynamic signaling network that modulates these cell death pathways through paracrine signaling, exosome transfer, and direct cell interactions [25]. Understanding these interactions provides crucial insights for developing novel therapeutic strategies against advanced breast cancer, where conventional apoptosis-inducing treatments often fail due to emergent resistance mechanisms and adaptive survival pathways.
The conceptual framework of cell death crosstalk represents a paradigm shift in oncology, moving beyond viewing cell death pathways as independent linear cascades toward recognizing them as integrated networks with shared regulators, mutual inhibition, and synergistic activation. In stage IV breast cancer, this network exhibits unique characteristics influenced by the metastatic microenvironment, oxidative stress conditions, and accumulated genetic alterations that redefine cellular death thresholds [26]. This review comprehensively examines the molecular architecture of crosstalk between apoptosis, PANoptosis, autophagy, and ferroptosis, with specific emphasis on the implications for therapeutic development in advanced breast cancer.
Molecular Mechanisms of Cell Death Pathways
Apoptosis: The Canonical Programmed Cell Death Pathway
Apoptosis represents the best-characterized form of programmed cell death, playing a fundamental role in maintaining tissue homeostasis and eliminating damaged cells. In breast cancer, apoptosis occurs through two main signaling pathways: the extrinsic (death receptor-mediated) and intrinsic (mitochondrial) pathways [27]. The extrinsic pathway initiates when extracellular death ligands—including Fas ligand (FasL), tumor necrosis factor (TNF)-α, and TNF-related apoptosis-inducing ligand (TRAIL)—bind to their corresponding death receptors such as Fas receptor (FasR), TNFR1, DR4, and DR5 [27]. This ligand-receptor interaction triggers the assembly of the death-inducing signaling complex (DISC), which recruits and activates caspase-8. Activated caspase-8 then cleaves and activates executioner caspase-3, leading to the characteristic morphological changes of apoptosis, including cellular shrinkage, chromatin condensation, and DNA fragmentation [27].
The intrinsic pathway activates in response to intracellular stress signals such as DNA damage, oxidative stress, and endoplasmic reticulum dysfunction [27]. These stressors trigger the activation of the tumor suppressor p53, which promotes transcription of pro-apoptotic Bcl-2 family proteins, including Bad and Bid, that antagonize anti-apoptotic proteins such as Bcl-2 and Bcl-xL [27]. The resulting oligomerization of Bax and Bak on the outer mitochondrial membrane increases permeability, facilitating the release of cytochrome c (CytC) into the cytoplasm [27]. CytC then forms the apoptosome complex with apoptotic protease activating factor 1 (Apaf-1) and procaspase-9, leading to caspase-9 activation, which subsequently activates caspase-3 [27].
In triple-negative breast cancer (TNBC), apoptosis resistance emerges through multiple mechanisms, including upregulation of anti-apoptotic proteins, downregulation of pro-apoptotic proteins, and differential expression of Bcl-2 family members [27]. The overexpression of MUC1 in TNBC activates NF-κB signaling, leading to enhanced transcription of Bcl-2 and further inhibition of cytochrome c release [27]. Additionally, activation of the EGFR/PI3K/Akt signaling pathway promotes survival and suppresses apoptotic signaling [27].
PANoptosis: An Integrated Cell Death Framework
PANoptosis represents a novel inflammatory cell death pathway that integrates components from apoptosis, pyroptosis, and necroptosis [28] [26]. This unified cell death concept is orchestrated by the PANoptosome complex, which serves as a molecular scaffold for simultaneous activation of multiple cell death pathways [26]. To date, four primary types of PANoptosomes have been identified: the ZBP1-PANoptosome (containing ZBP1, NLRP3, ASC, caspase-1, caspase-6, caspase-8, RIPK1, and RIPK3), AIM2-PANoptosome (containing AIM2, Pyrin, ZBP1, ASC, caspase-1, caspase-8, FADD, RIPK1, and RIPK3), and RIPK1-PANoptosome [26].
The PANoptosis pathway exemplifies the profound crosstalk between different cell death modalities, where activation of one pathway can simultaneously engage others through shared molecular components. Caspase-8 functions as a critical molecular switch in PANoptosis, enabling transition between apoptotic, necroptotic, and pyroptotic pathways [29]. Similarly, c-Myc can inhibit necroptosis while facilitating connections between pyroptosis and apoptosis via caspase-8 and caspase-3 [29]. This integrated cell death mechanism provides a robust defense against pathogens and damaged cells but also presents complex challenges in cancer therapy, where manipulation of one death pathway may trigger compensatory activation of others.
Table 1: Key Molecular Components of PANoptosis
| Component | Role in PANoptosis | Associated Pathways |
|---|---|---|
| Caspase-8 | Molecular switch between apoptosis, necroptosis, and pyroptosis | Apoptosis, Necroptosis, Pyroptosis |
| ZBP1 | Sensor of nucleic acids, nucleates PANoptosome complex | Innate immunity, Viral response |
| RIPK1 | Regulates cell survival and death decisions | Apoptosis, Necroptosis |
| RIPK3 | Mediates necroptotic signaling | Necroptosis |
| NLRP3 | Inflammasome component | Pyroptosis |
| ASC | Adaptor protein bridging sensors and effectors | Pyroptosis |
| Caspase-1 | Executer of pyroptosis | Pyroptosis |
| Caspase-6 | Apoptotic caspase engaged in PANoptosis | Apoptosis |
Autophagy: The Dual-Role Degradation Pathway
Autophagy is a catabolic process that degrades and recycles obsolete, damaged, or harmful macromolecular assemblies through lysosomal degradation [30]. This process begins with vesicle nucleation, where macromolecular assemblies targeted for degradation become surrounded by isolation membranes called phagophores [30]. The nucleation step is executed by a protein complex containing class III phosphatidylinositol-3-kinase (PI3Kc3 or VPS34), its regulatory subunit (p150 or VPS15), and the BCL-2 interacting protein Beclin 1 (ATG6) [30]. The core complex further associates with various modulators including Ambra 1, ATG14, UVRAG, Vmp1, Bif-1, and Rubicon, forming complexes with distinct functions in membrane trafficking processes [30].
The phagophore membranes subsequently enlarge and fuse at their edges to form multi-layered vesicles called autophagosomes, a process mediated by two ubiquitin-like conjugation systems [30]. In one system, ATG12 conjugates to ATG5 through the sequential activity of E1-like enzyme ATG7 and E2-like enzyme ATG10 [30]. The ATG12-ATG5 conjugate then forms a multimeric complex with ATG16. In the parallel system, ATG8/LC3 is conjugated to phosphatidylethanolamine through the protease ATG4, E1-like enzyme ATG7, and E2-like enzyme ATG3 [30]. The mature autophagosomes eventually fuse with lysosomes to create autophagolysosomes, where the encapsulated contents are degraded by lysosomal enzymes and the resulting metabolites are recycled [30].
In cancer, autophagy plays a paradoxical dual role [30] [31]. During early tumorigenesis, autophagy functions as a tumor suppressor by degrading potentially oncogenic molecules and preventing the accumulation of damaged organelles [30]. However, in advanced stages like stage IV breast cancer, autophagy promotes tumor cell survival by ameliorating stress in the microenvironment, facilitating metabolic adaptation, and supporting growth under nutrient deprivation [31]. This context-dependent functionality makes autophagy a challenging therapeutic target that requires careful modulation rather than simple inhibition or activation.
Ferroptosis: Iron-Dependent Lipid Peroxidation
Ferroptosis is an iron-dependent form of regulated cell death characterized by the accumulation of lipid-based reactive oxygen species (ROS) [32]. Unlike other cell death modalities, ferroptosis exhibits unique morphological features, including mitochondrial shrinkage with increased membrane density and reduction of mitochondrial cristae, without chromatin condensation or plasma membrane breakdown [32]. The biochemical hallmarks of ferroptosis include the loss of lipid peroxide repair capacity by glutathione peroxidase 4 (GPX4), the availability of redox-active iron, and the oxidation of polyunsaturated fatty acid (PUFA)-containing phospholipids [32].
The ferroptosis pathway is primarily regulated through system xc-, a cystine/glutamate antiporter that imports cystine for glutathione (GSH) synthesis [32]. GSH serves as an essential cofactor for GPX4, which converts lipid hydroperoxides to lipid alcohols, thereby preventing lethal lipid peroxidation [32]. Inhibition of system xc- (by erastin) or direct targeting of GPX4 (by RSL3) disrupts this protective mechanism, leading to iron-dependent lipid peroxidation and cell death [32]. Additional regulators include NCOA4, which mediates ferritinophagy to increase cellular labile iron levels, and ACSL4, which enriches cellular membranes with long polyunsaturated n-6 fatty acids that are susceptible to peroxidation [32].
In breast cancer, ferroptosis sensitivity varies between subtypes, with triple-negative breast cancer (TNBC) demonstrating heightened vulnerability compared to ER-positive subtypes [32] [27]. This differential sensitivity offers therapeutic opportunities, particularly for TNBC where targeted treatment options are limited. Drug-tolerant persister breast cancer cells develop dependency on GPX4, making them vulnerable to ferroptosis induction, suggesting a promising approach to overcome therapy resistance [32].
Table 2: Characteristic Features of Different Cell Death Modalities
| Feature | Apoptosis | PANoptosis | Autophagy | Ferroptosis |
|---|---|---|---|---|
| Morphology | Chromatin condensation, membrane blebbing, apoptotic bodies | Combined features of apoptosis, pyroptosis, and necroptosis | Double-membraned autophagosomes, autolysosomes | Mitochondrial shrinkage, increased membrane density |
| Key Mediators | Caspases, Bcl-2 family, cytochrome c | PANoptosome complex, caspase-8, RIPK1, RIPK3 | ATG proteins, Beclin-1, LC3 | GPX4, system xc-, lipid ROS, iron |
| Inflammation | Non-inflammatory | Highly inflammatory | Generally anti-inflammatory | Immunogenic |
| Role in Cancer | Tumor suppressor | Context-dependent | Dual role (suppressor and promoter) | Context-dependent |
| Biomarkers | Cleaved caspases, PARP cleavage, Annexin V | Combined markers from multiple pathways | LC3-I/II conversion, p62 degradation | Lipid peroxides, GSH depletion, ACSL4 |
Mechanisms of Crosstalk Between Cell Death Pathways
Molecular Nodes of Convergence
The crosstalk between different cell death pathways occurs through shared molecular nodes that can initiate, modulate, or execute multiple death programs simultaneously. The tumor suppressor p53 represents a critical convergence point, directly regulating both apoptotic and ferroptotic pathways [33]. In apoptosis, p53 activates transcription of pro-apoptotic genes including Puma/Bbc3 and Noxa/Pmaip [33]. Simultaneously, p53 promotes ferroptosis by suppressing expression of the anti-ferroptosis protein SLC7A11 (a subunit of system xc-) and upregulating SAT1, which leads to increased expression of the pro-ferroptotic protein ALOX15 [33]. This dual regulation enables coordinated activation of distinct death modalities in response to cellular stress.
Caspase-8 serves as another crucial molecular integrator, particularly in PANoptosis, where it functions as a switch between apoptotic, necroptotic, and pyroptotic pathways [29]. The ability of caspase-8 to cleave and activate multiple substrates, including crosstalk with caspase-3 and gasdermin proteins, enables this protease to coordinate different death programs based on cellular context and stimulus [29]. Additionally, the efflux of potassium ions induced by apoptosis has been demonstrated to enhance activation of inflammasomes and pyroptosis, conferring immunogenicity to chemotherapy [29].
Reactive oxygen species (ROS) represent a fundamental biochemical convergence point for multiple cell death pathways [26]. In apoptosis, ROS function as signaling molecules that promote mitochondrial outer membrane permeabilization [27]. In ferroptosis, ROS specifically drive iron-dependent lipid peroxidation [32]. PANoptosis integrates ROS signaling from multiple sources, including mitochondrial electron transport, NADPH oxidase (NOX) activity, and arachidonic acid metabolism through lipoxygenase (LOX) and cyclooxygenase (COX) pathways [26]. The antioxidant defense system, comprising superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPX), and glutathione reductase (GR), attempts to maintain redox homeostasis and determines cell fate decisions at this convergence point [26].
Organellar Platforms for Crosstalk
Intracellular organelles serve as physical platforms that facilitate crosstalk between different cell death pathways. Mitochondria integrate apoptotic, ferroptotic, and autophagic signaling through multiple mechanisms [33]. In apoptosis, mitochondria release cytochrome c to activate the apoptosome [27]. In ferroptosis, mitochondria generate lipid peroxides that drive iron-dependent death [32]. Mitophagy, the selective autophagic degradation of mitochondria, can suppress both apoptosis and ferroptosis by removing damaged mitochondria, while insufficient mitophagy can promote cell death through ROS accumulation [29].
The endoplasmic reticulum (ER) provides another crucial platform, particularly for the crosstalk between autophagy and apoptosis [30]. ER stress activates the unfolded protein response, which can simultaneously induce autophagy through IRE1 and PERK signaling while triggering apoptosis via CHOP activation [30]. The ER also serves as a membrane source for autophagosome formation and regulates calcium signaling that impacts both apoptotic and necroptotic pathways [30].
Lysosomes physically connect autophagy and ferroptosis through ferritinophagy, the autophagic degradation of ferritin that releases iron and promotes ferroptosis [29]. Cancer cells can counteract this connection by promoting iron export through prominin2-mediated formation of ferritin-containing multivesicular bodies and exosomes, thereby inhibiting ferroptosis [32]. This organellar coordination enables cells to integrate diverse stress signals and mount appropriate death responses based on stimulus intensity, duration, and context.
Transcriptional and Epigenetic Regulation
The crosstalk between cell death pathways extends to transcriptional and epigenetic levels, creating durable adaptive responses that influence therapeutic outcomes in stage IV breast cancer. Transcriptomic analyses reveal significant overlap between ferroptosis and apoptosis responses, with common upregulated genes including NRF2 targets that mitigate oxidative stress in both pathways [33]. However, death module-specific genes can classify transcriptomic responses with high accuracy (AUC = 0.84-0.9), enabling precise identification of activated death pathways in experimental and clinical settings [33].
Epigenetic mechanisms, including noncoding RNAs, DNA methylation, and histone modifications, mediate sophisticated regulation of cell death crosstalk in breast cancer [26]. Specific microRNAs can simultaneously regulate components of multiple death pathways, creating coordinated responses to therapeutic interventions. The development of "epigenetic triggers" that selectively prime resistant cells for programmed cell death execution represents an emerging therapeutic approach for advanced breast cancer [26].
The conceptual framework of a "redox-programmed cell death axis" has been proposed to explain how ROS metabolic imbalance coordinates crosstalk between different death modalities in breast cancer [26]. This axis integrates production and elimination of ROS with multiple PCD pathways, creating a network that determines cell fate decisions in response to therapy, microenvironmental stresses, and oncogenic signaling. Understanding the molecular thresholds that determine shifts from pro-survival signaling to lethal PCD execution within this axis represents a crucial research direction for improving breast cancer treatment [26].
Experimental Approaches for Studying Cell Death Crosstalk
Transcriptomic Analysis and Classification
Investigating crosstalk between cell death pathways requires sophisticated experimental approaches that can distinguish between different death modalities and their interactions. Transcriptomic analysis has emerged as a powerful method for characterizing death-specific responses and identifying crosstalk mechanisms [33]. However, comparing transcriptomic landscapes between different death modules presents challenges due to remarkable variability caused by diverse inducers, biological models, and experimental settings [33].
To overcome these challenges, researchers have employed innovative approaches including analysis of multiple transcriptomic datasets (23 for ferroptosis inducers and 26 for apoptosis inducers) to identify death module-specific genes versus common genes shared by both pathways [33]. Two complementary methods have proven effective: (1) frequency-based identification of genes significantly upregulated in at least 40% of datasets for each death module, and (2) fold-change-based comparison of gene expression between ferroptosis and apoptosis datasets [33]. These approaches have identified reliable transcriptomic classifiers that can distinguish between death modules with high accuracy (area under the curve = 0.84-0.9) [33].
Programming a continuous transcriptomic landscape between ferroptosis and apoptosis represents another advanced methodological approach [33]. This strategy involves titrating drug combinations (such as JQ1 and bortezomib) to induce a gradual transition from one death modality to another in the same biological model, enabling identification of a "Gradient Gene Set" (GGS) that captures the transcriptomic shift between death pathways [33]. The GGS of 306 genes, particularly a refined subset of 15-24 biomarkers, can classify ferroptosis and apoptosis with high accuracy (AUC = 0.88) and has been validated in cultured cells and mouse models of breast cancer [33].
Table 3: Research Reagent Solutions for Studying Cell Death Crosstalk
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Ferroptosis Inducers | Erastin, RSL3, Sulfasalazine (SAS) | Inhibit system xc- or GPX4 to induce ferroptosis |
| Apoptosis Inducers | TRAIL, TNF-α, ABT-263 (Navitoclax) | Activate death receptors or inhibit Bcl-2 |
| Autophagy Modulators | Chloroquine, Bafilomycin A1 (inhibitors); Rapamycin (inducer) | Modulate autophagic flux |
| PANoptosis Components | Z-VAD-FMK (pan-caspase inhibitor), Necrostatin-1 (RIPK1 inhibitor) | Dissect contribution of specific pathways in PANoptosis |
| Iron Chelators | Deferoxamine, Deferiprone | Confirm iron dependence in ferroptosis |
| Antioxidants | Ferrostatin-1, Liproxstatin-1, Vitamin E | Inhibit lipid peroxidation in ferroptosis |
| Transcriptomic Tools | RNA sequencing, Gene expression classifiers (GGS) | Identify death modality and crosstalk mechanisms |
| Cell Death Assays Annexin V/PI staining, Caspase activity assays, Lipid peroxidation probes (C11-BODIPY) | Quantify specific death modalities and concurrent activation |
Pharmacological and Genetic Approaches
Dissecting cell death crosstalk requires targeted interventions that specifically modulate individual pathways while monitoring effects on other death modalities. Pharmacological approaches utilize selective inhibitors and inducers for each pathway, including ferrostatin-1 and liproxstatin-1 for ferroptosis inhibition, Z-VAD-FMK for caspase-dependent apoptosis inhibition, necrostatin-1 for necroptosis inhibition, and chloroquine for autophagy inhibition [29] [32]. These tools enable researchers to determine the contribution of specific pathways to cell death in different contexts.
Genetic approaches provide complementary strategies through knockout, knockdown, or overexpression of key regulatory genes. For example, FDX1 knockout has been used to validate its essential role in cuproptosis [28], while GPX4 knockout cells demonstrate the essential function of this enzyme in preventing ferroptosis [32]. CRISPR/Cas9 screens have identified seven key genes that promote cuproptosis (FDX1, LIPT1, LIAS, DLD, DLAT, PDHA1, and PDHB), providing genetic evidence for this novel death pathway and its potential crosstalk with other modalities [28].
Combined pharmacological and genetic approaches are particularly powerful for establishing causal relationships in death pathway crosstalk. For instance, studies demonstrating that ferroptosis inducers (erastin) can upregulate pyroptosis-associated proteins, while ferroptosis inhibitors can suppress pyroptosis, provide compelling evidence for interconnection between these pathways [29]. Similarly, the observation that lipopolysaccharide (LPS), a classic pyroptosis inducer, can also trigger ferroptosis indicates bidirectional crosstalk between these inflammatory death pathways [29].
Advanced Imaging and Multiparameter Assessment
Advanced imaging techniques enable real-time monitoring of multiple cell death parameters in live cells, providing dynamic information about crosstalk kinetics and sequence. Fluorescent probes for specific death markers—such as Annexin V for apoptosis, C11-BODIPY for lipid peroxidation in ferroptosis, LysoTracker for lysosomal integrity, and LC3-GFP for autophagy flux—can be combined to visualize concurrent activation of different pathways in the same cells [32].
Multiparameter flow cytometry represents another powerful approach for quantifying the coexistence of different death modalities in cell populations. This technique can simultaneously measure caspase activation, membrane integrity, lipid peroxidation, and mitochondrial membrane potential in thousands of individual cells, providing statistical power for analyzing heterogeneous responses [32]. Combined with genetic barcoding, this approach enables high-throughput screening of chemical libraries or genetic perturbations for effects on cell death crosstalk.
Electron microscopy remains invaluable for characterizing the ultrastructural features associated with different death modalities, particularly for distinguishing between ferroptosis (shrunken mitochondria with condensed membranes), apoptosis (nuclear condensation and apoptotic bodies), and autophagic cell death (abundant autophagosomes) [32]. Correlative light and electron microscopy (CLEM) combines the molecular specificity of fluorescence imaging with the ultrastructural context of EM, providing unprecedented insights into the subcellular organization of death pathway crosstalk.
Therapeutic Implications for Stage IV Breast Cancer
Overcoming Therapy Resistance
The crosstalk between cell death pathways has profound implications for overcoming therapy resistance in stage IV breast cancer. Traditional treatments primarily engage apoptotic pathways, but cancer cells frequently develop resistance through upregulation of anti-apoptotic proteins, impaired caspase activation, or enhanced survival signaling [34] [27]. Leveraging alternative death pathways provides promising strategies to bypass these resistance mechanisms.
Inducing ferroptosis represents a particularly promising approach for eliminating apoptosis-resistant cancer cells, especially in triple-negative breast cancer (TNBC) where ferroptosis sensitivity is heightened [32] [27]. Drug-tolerant persister cells—a major reservoir for relapse—develop dependency on GPX4, making them vulnerable to ferroptosis induction [32]. Combination therapies that simultaneously inhibit GPX4 and system xc- can effectively target these resistant populations. Additionally, pharmacological iron chelators or antioxidants can modulate ferroptosis sensitivity, providing strategies to enhance therapeutic selectivity and reduce off-target effects [32].
Modulating autophagy presents another therapeutic opportunity, though its dual role in cancer necessitates context-dependent strategies [30] [31]. In early treatment phases, autophagy inhibition may enhance cell death by preventing stress adaptation, while in advanced stages, strategic autophagy induction might promote autophagic cell death or enhance immunogenicity [31]. The integration of autophagy modifiers with conventional chemotherapy, targeted therapy, or immunotherapy represents an active area of clinical investigation for advanced breast cancer [34].
Combination Therapy Strategies
Rational combination therapies that simultaneously target multiple cell death pathways offer enhanced efficacy and reduced resistance compared to monotherapies. The combination of apoptosis inducers with ferroptosis activators can produce synergistic effects, particularly in heterogeneous tumors containing both apoptosis-sensitive and apoptosis-resistant subpopulations [33] [32]. For example, BH3 mimetics that inhibit anti-apoptotic Bcl-2 proteins can sensitize cancer cells to ferroptosis inducers, creating a dual death activation strategy [33].
Combining death receptor agonists with autophagy modulators represents another promising approach for HER2-positive breast cancer, where autophagy activation contributes to resistance against HER2-targeted therapies like trastuzumab and lapatinib [34]. Simultaneous inhibition of protective autophagy and activation of death receptor signaling can overcome this resistance mechanism and restore therapeutic sensitivity [34].
Nanoparticle-based delivery systems provide innovative platforms for implementing sophisticated combination strategies that target cell death crosstalk [28] [26]. Engineering "PCD-cascade nanoparticles" that leverage tumor microenvironment signals to sequentially activate multiple death pathways represents a cutting-edge approach [26]. These systems can be designed to release different therapeutic payloads in response to specific tumor microenvironment conditions, such as low pH, elevated ROS, or specific enzyme activities, enabling spatially and temporally controlled activation of complementary death mechanisms [26].
Biomarker-Driven Patient Stratification
The development of reliable biomarkers for different cell death pathways enables patient stratification and treatment personalization in stage IV breast cancer. Transcriptomic classifiers, such as the Gradient Gene Set (GGS) that distinguishes ferroptosis from apoptosis, can identify tumors with inherent sensitivity to specific death modalities [33]. Similarly, gene expression signatures for autophagy dependence or PANoptosis competence could guide selection of appropriate targeted therapies [26].
Imaging biomarkers represent another promising approach for non-invasive assessment of cell death activation in tumors. Advanced magnetic resonance imaging (MRI) techniques sensitive to iron metabolism could monitor ferroptosis induction, while positron emission tomography (PET) tracers targeting caspase activation or membrane phospholipid changes could assess apoptotic response [32]. These imaging biomarkers would enable real-time monitoring of treatment efficacy and adaptive therapy modification.
Liquid biopsy approaches that detect cell death-specific markers in circulation provide minimally invasive tools for tracking therapeutic response and emergence of resistance [26]. Differences in the surface composition and molecular cargo of vesicles released during different forms of cell death could serve as specific biomarkers for determining which death pathways are activated in response to therapy [32]. Integrating these circulating biomarkers with tumor genotyping would create comprehensive profiles for precision medicine in advanced breast cancer.
Visualizing Signaling Pathways and Experimental Workflows
Diagram 1: Cell Death Crosstalk Network. This diagram illustrates the molecular connections and crosstalk between apoptosis, PANoptosis, ferroptosis, and autophagy. Key convergence points include p53, ROS, and mitochondrial dysfunction, which coordinate activity across different death pathways. Dashed lines represent crosstalk connections, while solid lines show direct pathway progression.
Diagram 2: Experimental Workflow for Studying Cell Death Crosstalk. This diagram outlines a comprehensive approach for investigating interactions between different cell death pathways, including model selection, pathway perturbation, multiparameter monitoring, and integrated analysis to elucidate crosstalk mechanisms.
The crosstalk between PANoptosis, autophagy, ferroptosis, and apoptosis represents a complex regulatory network that profoundly influences therapeutic responses in stage IV breast cancer. Rather than operating in isolation, these pathways form an integrated system with shared molecular regulators, organellar platforms, and adaptive responses that determine cell fate decisions. Understanding this crosstalk provides critical insights for developing novel therapeutic strategies that simultaneously target multiple death pathways to overcome resistance mechanisms in advanced breast cancer.
The future of targeting cell death crosstalk lies in developing biomarker-driven combination therapies, sophisticated nanoparticle delivery systems, and dynamic treatment adaptations based on real-time monitoring of death pathway activation. As research continues to unravel the complexities of this crosstalk network, new opportunities will emerge for precision medicine approaches that leverage the unique cell death vulnerabilities of individual tumors, ultimately improving outcomes for patients with stage IV breast cancer.
Subtype-Specific Apoptotic Dysregulation in HER2-Positive and Triple-Negative Breast Cancer (TNBC)
Apoptotic dysregulation is a fundamental hallmark of cancer, enabling malignant cells to evade programmed cell death and sustain uncontrolled proliferation. In breast cancer, the specific mechanisms of apoptosis evasion vary significantly across molecular subtypes, presenting distinct therapeutic challenges and opportunities. This review provides an in-depth analysis of the subtype-specific apoptotic alterations in HER2-positive and Triple-Negative Breast Cancer (TNBC), two particularly aggressive forms of the disease. HER2-positive breast cancer, characterized by amplification of the HER2/neu oncogene, constitutes approximately 15-30% of breast cancers and demonstrates particular apoptotic resistance mechanisms [35] [36]. TNBC, defined by the absence of estrogen receptor (ER), progesterone receptor (PR), and HER2 expression, represents 15-20% of cases and exhibits its own unique apoptotic dysregulation patterns [27]. Understanding these distinct mechanistic pathways is crucial for developing targeted therapeutic strategies, especially in the context of advanced stage IV disease where apoptotic resistance often dictates treatment failure and mortality.
HER2-Positive Breast Cancer: Apoptotic Dysregulation Mechanisms
HER2 Signaling Biology and Network Architecture
HER2 (human epidermal growth factor receptor 2), also known as ERBB2, is a transmembrane receptor tyrosine kinase that functions as a master regulator of proliferative and survival signaling [35]. Unlike other EGFR family members, HER2 has no known direct ligand and instead functions as the preferred dimerization partner for other HER family receptors [36]. In HER2-positive breast cancer, gene amplification leads to massive protein overexpression with up to 2 million receptors expressed at the tumor cell surface, creating potent signaling hubs that dominantly drive anti-apoptotic programming [35]. The HER2 signaling network operates through a three-layer architecture: an input layer of membrane receptors and ligands, a core processing layer of protein kinases, and an output layer of transcription factors regulating cellular functions [35].
Table 1: Key Anti-Apoptotic Signaling Pathways Activated by HER2
| Signaling Pathway | Mechanism of Activation | Key Anti-Apoptotic Effects |
|---|---|---|
| PI3K-AKT | HER2-HER3 heterodimers recruit and activate PI3K; HER2 phosphorylation creates docking sites | Phosphorylates/inactivates pro-apoptotic proteins; activates MDM2 to degrade p53; enhances anti-apoptotic protein synthesis |
| Ras-MAPK | GRB2-SOS complex recruitment activates Ras; sequential kinase activation | Promotes transcription of anti-apoptotic genes; enhances cell cycle progression |
| JAK-STAT | Direct phosphorylation by HER2 or secondary cytokine activation | Induces transcription of survival genes; promotes cell proliferation |
Specific Mechanisms of Apoptotic Suppression
HER2 overexpression orchestrates a multi-faceted anti-apoptotic program through several interconnected mechanisms that impact both intrinsic and extrinsic apoptotic pathways. The primary function of HER2 signaling is suppressing apoptosis to enhance cell survival, giving rise to uncontrolled proliferation and tumor growth [37].
Mitochondrial (Intrinsic) Pathway Regulation: HER2 activation profoundly influences the Bcl-2 family protein equilibrium, shifting the balance toward survival. HER2-mediated activation of PI3K-AKT signaling leads to increased expression of anti-apoptotic Bcl-2 family members including Bcl-2, Bcl-xL, and Mcl-1 [37]. These proteins sequester pro-apoptotic factors like Bax and Bak, preventing mitochondrial outer membrane permeabilization and subsequent cytochrome c release. Recent evidence also suggests HER2 can directly translocate to the mitochondria to inhibit cytochrome c release through mechanisms independent of its signaling function [37].
Death Receptor (Extrinsic) Pathway Modulation: HER2 signaling attenuates cellular responsiveness to extracellular death signals. HER2 activation suppresses cellular reaction to death ligands, especially TRAIL (TNF-related apoptosis-inducing ligand)-induced apoptosis [37]. This occurs through multiple mechanisms including downregulation of death receptors and upregulation of intracellular FLICE-inhibitory proteins (FLIPs) that compete with caspase-8 activation at the death-inducing signaling complex (DISC).
p53 Pathway Interference: HER2 disrupts p53-mediated apoptosis through AKT-mediated upregulation of MDM2, the primary negative regulator of p53 [37]. MDM2 ubiquitinates p53, targeting it for proteasomal degradation and effectively neutralizing this critical tumor suppressor pathway. Additionally, HER2 can modulate p53 transcriptional activity through phosphorylation events that alter its DNA-binding affinity.
Caspase Inhibition via Survivin: Survivin expression is frequently increased with HER2 overexpression, leading to direct inhibition of caspase activation and creation of an additional blockade in the apoptotic execution phase [37]. Survivin, a member of the inhibitor of apoptosis (IAP) family, is notably overexpressed in many cancers and represents a significant therapeutic target.
Experimental Models and Methodologies
HER2 Signaling Inhibition Studies: Investigation of HER2-mediated apoptotic dysregulation employs various experimental approaches targeting the HER2 pathway. The monoclonal antibody trastuzumab binds the extracellular domain of HER2, initiating internalization and degradation while also recruiting immune effector cells through antibody-dependent cellular cytotoxicity (ADCC) [35] [36]. Trastuzumab treatment increases p27, a cyclin-dependent kinase inhibitor that halts cell proliferation [36]. Research methodologies include immunoprecipitation of HER2 complexes followed by Western blot analysis for downstream signaling components, proliferation assays (MTT, XTT), and apoptosis detection (Annexin V staining, caspase activation assays) in HER2-positive cell lines such as SKBR-3 and BT-474 [37] [35].
Tyrosine Kinase Inhibitor Approaches: Small molecule tyrosine kinase inhibitors including lapatinib, neratinib, and tucatinib target the intracellular kinase domain of HER2, blocking downstream signaling regardless of dimerization status [36]. These agents are particularly valuable for studying signaling dynamics and have demonstrated efficacy against trastuzumab-resistant tumors in preclinical models. Experimental protocols typically involve dose-response studies with concurrent assessment of phosphorylation status (pHER2, pAKT, pERK) and apoptotic markers to establish mechanism-based relationships.
Antibody-Drug Conjugate Mechanisms: Ado-trastuzumab emtansine (T-DM1) and trastuzumab deruxtecan represent advanced therapeutic approaches that combine HER2 targeting with cytotoxic payload delivery [37] [36]. These compounds enable precise investigation of apoptotic induction in HER2-overexpressing cells through internalization of potent chemotherapeutic agents. Methodologies for studying these agents include trafficking studies with fluorescently labeled antibodies, assessment of DNA damage markers for payload mechanism analysis, and comparison of apoptotic indices between conventional HER2-targeting and ADC approaches.
Diagram 1: HER2-Mediated Apoptotic Suppression Signaling Network. HER2 activation triggers multiple downstream pathways that collectively suppress apoptosis through regulation of Bcl-2 family proteins, p53 degradation, and survivin upregulation.
Triple-Negative Breast Cancer: Apoptotic Dysregulation Mechanisms
TNBC Landscape and Apoptotic Alterations
Triple-negative breast cancer is characterized by the absence of estrogen receptor, progesterone receptor, and HER2 expression, creating a therapeutic landscape devoid of established targeted approaches [27]. TNBC accounts for approximately 15-20% of all invasive breast cancer cases and is associated with heightened invasion, metastasis, recurrence, and poor survival [27]. The apoptotic dysregulation in TNBC involves distinct mechanisms from HER2-positive disease, with particular emphasis on death receptor signaling, p53 pathway mutations, and emerging programmed cell death modalities. TNBC exhibits substantial heterogeneity at both intertumoral and intratumoral levels, manifesting in divergent clinical, pathological, histological, and molecular profiles that complicate therapeutic targeting [27].
Death Receptor Signaling Alterations
The extrinsic apoptotic pathway demonstrates significant alteration in TNBC, particularly in metastatic progression. Research has revealed that metastatic TNBC tumor cells exhibit greater resistance to apoptosis induction compared to their primary tumor counterparts, with death receptor-5 (DR-5) playing a pivotal role [38]. In studies using a 4T1 syngeneic mouse model of breast cancer, metastatic tumor cells extracted from lung tissue demonstrated significantly higher resistance to curcumin-induced apoptosis compared to primary tumor cells [38]. This correlated with reduced DR-5 upregulation in metastatic cells following curcumin treatment, suggesting death receptor dysregulation as a mechanism of apoptotic resistance in advanced disease.
Quantitative analysis demonstrated that primary tumor cells treated with 120 μM curcumin showed significantly higher DR-5 gene expression upregulation (3.8-fold increase) compared to metastatic cells (1.5-fold increase) [38]. This differential death receptor expression provides important insights into the molecular mechanism of apoptosis resistance of metastatic tumor cells and can inform targeted therapeutic strategies for combatting metastatic TNBC.
TP53 Mutations and Calcium Signaling Dysregulation
TP53 mutations occur in the majority of TNBC cases, disrupting p53's role in DNA repair and apoptosis [39]. Beyond its canonical transcriptional functions, p53 influences calcium signaling through store-operated calcium entry (SOCE), a critical pathway for cell survival and death [39] [40]. Recent research has revealed a novel link between specific TP53 mutation types and calcium signaling dysregulation in TNBC, with important implications for apoptotic sensitivity.
Table 2: TP53 Mutation-Specific Effects on Calcium Signaling and Apoptosis in TNBC
| TP53 Mutation Type | Store-Operated Calcium Entry | CACNA1D Expression | Apoptotic Sensitivity |
|---|---|---|---|
| Wild-type | Normal SOCE | Normal expression | Standard apoptotic response |
| R273H Missense | Similar to wild-type | Moderate reduction | Moderate resistance |
| Frameshift mutations | Significantly reduced | Markedly downregulated | High resistance |
| Stop mutations | Significantly reduced | Markedly downregulated | High resistance |
Bioinformatic analysis of TNBC datasets revealed significant downregulation of CACNA1D (encoding CaV1.3, an L-type voltage-gated calcium channel) in TP53-mutant TNBCs [39] [40]. Functional studies demonstrated that TNBC cell lines harboring frameshift and stop TP53 mutations exhibited reduced store-operated calcium entry, lower CACNA1D expression, and resistance to thapsigargin-induced apoptosis compared to wild-type cells [39]. In contrast, cells with the TP53 R273H missense mutation demonstrated similar calcium signaling and proliferation to TP53 wild-type cells, indicating mutation-specific effects [39].
Treatment with the p53 reactivator COTI-2 restored CACNA1D expression and SOCE in frameshift and stop mutant cells, enhancing apoptotic sensitivity [39]. Combined treatment with COTI-2 and thapsigargin resulted in a synergistic increase in apoptosis, highlighting the therapeutic potential of targeting both TP53 dysfunction and calcium signaling [39].
Non-Coding RNA Regulation of Apoptosis
Long non-coding RNAs (lncRNAs) represent another layer of apoptotic regulation in TNBC, offering potential therapeutic targets. The lncRNA GAS5 (growth-arrest specific transcript 5) is significantly downregulated in TNBC cells treated with paclitaxel or cisplatin, and its low expression correlates with reduced apoptosis under stress conditions [41]. Clinically, GAS5 expression levels in TNBC patients associate with tumor resistance to paclitaxel and cisplatin [41].
Mechanistic studies reveal that GAS5 promotes apoptosis by directly binding to miR-378a-5p, functioning as a molecular sponge to sequester this microRNA and prevent its repression of the SUFU (Suppressor of Fused) gene [41]. SUFU, a component of the Hedgehog signaling pathway, demonstrates previously unappreciated pro-apoptotic functions in this context. Experimental validation using RNA immunoprecipitation confirmed direct binding between GAS5 and miR-378, while Western blot and flow cytometry analyses demonstrated that the miR-378a-5p target SUFU promotes GAS5-induced apoptosis of TNBC cells [41]. In vivo studies using subcutaneous xenograft models established that GAS5 overexpression enhances TNBC sensitivity to paclitaxel, confirming its therapeutic potential [41].
Alternative Programmed Cell Death Pathways
Beyond classical apoptosis, TNBC demonstrates significant alterations in multiple programmed cell death pathways that contribute to its pathological behavior and therapeutic resistance [27]. The intricate interplay among these pathways provides a rich foundation for novel therapeutic interventions.
Ferroptosis: This iron-dependent form of cell death driven by lipid peroxidation is increasingly recognized as critical in TNBC pathogenesis [27]. Ferroptosis can directly kill tumor cells and modulate the tumor microenvironment to suppress progression. TNBC cells demonstrate varying susceptibility to ferroptosis inducers based on their metabolic programming and antioxidant capacity.
Necroptosis: This programmed form of necrosis has emerged as a pivotal compensatory mechanism in TNBC, particularly when apoptotic pathways are impaired [27]. Activation of necroptosis has been linked to improved responsiveness in resistant tumor phenotypes, suggesting its therapeutic induction could bypass apoptotic resistance mechanisms.
Pyroptosis: This lytic and inflammatory form of cell death exhibits dual roles in TNBC [27]. While it can eliminate tumor cells, it may also promote tumor growth under certain conditions through inflammatory microenvironment modulation.
Autophagy: Plays a paradoxical role in TNBC, functioning as both a pro-survival mechanism through intracellular component recycling and a cell death pathway when excessively activated [27]. The determination between these opposing outcomes depends on contextual factors including metabolic stress, therapeutic exposure, and tumor stage.
Diagram 2: TNBC Apoptotic Resistance Mechanisms. Multiple molecular alterations including TP53 mutations, death receptor-5 dysregulation, and lncRNA GAS5 downregulation collectively contribute to apoptosis resistance, while alternative programmed cell death pathways offer potential therapeutic alternatives.
Comparative Analysis of Apoptotic Dysregulation
Side-by-Side Mechanistic Comparison
The apoptotic dysregulation patterns in HER2-positive and TNBC demonstrate fundamentally distinct architectures despite sharing the common endpoint of cell death evasion. HER2-positive breast cancer employs a dominantly oncogene-driven strategy centered on hyperactive membrane signaling that coordinately suppresses multiple apoptotic pathways. In contrast, TNBC utilizes a more heterogeneous pattern of alterations spanning genomic, epigenetic, and metabolic domains without a single driver comparable to HER2 amplification.
Table 3: Comprehensive Comparison of Apoptotic Dysregulation in HER2-Positive vs. TNBC
| Characteristic | HER2-Positive Breast Cancer | Triple-Negative Breast Cancer |
|---|---|---|
| Primary drivers | HER2 oncogene amplification | TP53 mutations; diverse alterations |
| Key dysregulated pathways | PI3K-AKT; Ras-MAPK | Death receptor signaling; calcium homeostasis |
| Bcl-2 family regulation | Increased Bcl-2, Bcl-xL, Mcl-1 | Variable; context-dependent |
| p53 status | Wild-type but functionally inactivated | Mutated in >80% of cases |
| Death receptor signaling | Suppressed TRAIL response | DR-5 dysregulation in metastasis |
| Non-apoptotic PCD engagement | Limited | Significant (ferroptosis, necroptosis) |
| Non-coding RNA involvement | Less characterized | GAS5/miR-378a-5p/SUFU axis |
| Metabolic reprogramming | Secondary to signaling activation | Direct apoptotic modulation |
| Therapeutic targeting | HER2-directed antibodies, TKIs, ADCs | Chemotherapy; emerging targeted approaches |
| Apoptotic resistance mechanisms | Redundant signaling; receptor mutations | Multifactorial; tissue-context dependent |
Therapeutic Implications and Resistance Mechanisms
The distinct apoptotic dysregulation mechanisms in these subtypes directly inform therapeutic strategy and resistance patterns. In HER2-positive disease, targeted therapies including trastuzumab, pertuzumab, and antibody-drug conjugates like T-DM1 directly address the oncogenic driver but face resistance through multiple mechanisms including HER2 extracellular domain mutations (p95), PI3K pathway mutations, and activation of compensatory survival pathways [37] [35] [36]. Next-generation approaches include irreversible pan-ERBB inhibitors and combination therapies targeting both HER2 and apoptotic regulatory proteins [37].
For TNBC, the therapeutic landscape remains more challenging due to the absence of a single dominant driver. Conventional chemotherapy remains the mainstay but with limited efficacy due to frequent multidrug resistance [27]. Emerging strategies focus on targeting vulnerable points in the apoptotic machinery including DR-5 agonists, p53 reactivators like COTI-2, and modulation of alternative cell death pathways such as ferroptosis [39] [27] [38]. The recent integration of immunotherapy with apoptosis-inducing regimens shows particular promise for TNBC, potentially enhancing immune recognition through exposure of damage-associated molecular patterns during immunogenic cell death [27].
Experimental Approaches and Methodologies
Core Apoptosis Assessment Techniques
Morphological Assessment: The gold standard for apoptosis detection remains morphological assessment by electron or light microscopy examining chromatin condensation, nuclear fragmentation, cell shrinkage, and plasma membrane blebbing [21]. While highly specific, this approach is time-consuming and requires significant expertise, limiting its throughput capacity.
TUNEL Assay: Terminal deoxyribonucleotidyl transferase-mediated dUTP nick end labelling detects DNA fragmentation by incorporating labelled nucleotides onto the 3'-ends of DNA fragments [21]. This technique can be applied to formalin-fixed, paraffin-embedded clinical tissue and allows simultaneous examination of cell morphology, though it requires careful differentiation from necrotic cells.
Flow Cytometry Approaches: Annexin V/propidium iodide staining enables quantification of phosphatidylserine externalization as an early apoptotic marker while distinguishing late apoptosis and necrosis [38]. This method provides robust quantitative data and can be combined with intracellular staining for additional parameters. Caspase activity assays using fluorescent substrates offer specific detection of apoptotic execution phase activation.
Live-Cell Imaging: The Incucyte system and similar platforms enable real-time monitoring of apoptosis using fluorescent caspase substrates or membrane integrity markers, providing kinetic data throughout experimental timecourses [39]. This approach is particularly valuable for assessing the temporal dynamics of apoptotic response to therapeutic interventions.
Specialized Methodologies for Subtype-Specific Investigation
HER2 Signaling Analysis: Co-immunoprecipitation of HER2 receptor complexes followed by phosphotyrosine Western blotting identifies downstream signaling partners [35]. Proximity ligation assays can visualize receptor dimerization status in situ, while targeted phosphoprotein arrays provide comprehensive signaling pathway activation profiling.
Calcium Imaging: Fura-2AM ratiometric imaging enables quantitative assessment of store-operated calcium entry in TNBC models, particularly relevant for investigating TP53 mutation effects on calcium homeostasis [39]. This methodology can be combined with pharmacological modulators of specific calcium channels to dissect contribution mechanisms.
Metastatic Cell Isolation: For TNBC metastasis studies, enzymatic digestion (collagenase type IV) of primary tumors and metastatic organs (e.g., lung tissue) followed by differential centrifugation enables isolation of metastatic cells for comparative analysis with their primary tumor counterparts [38]. This approach permits direct investigation of apoptosis resistance mechanisms acquired during metastatic progression.
lncRNA Functional Analysis: RNA immunoprecipitation confirms direct binding between lncRNAs (e.g., GAS5) and their miRNA targets (e.g., miR-378a-5p) [41]. Dual luciferase reporter assays validate functional targeting, while gain- and loss-of-function approaches using overexpression vectors and siRNA establish phenotypic consequences.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating Apoptotic Dysregulation in Breast Cancer Subtypes
| Reagent/Category | Specific Examples | Research Applications | Subtype Relevance |
|---|---|---|---|
| HER2-targeting agents | Trastuzumab, Lapatinib, Neratinib | HER2 signaling inhibition; therapeutic mechanism studies | HER2-positive |
| Apoptosis inducers | Curcumin, Cisplatin, Paclitaxel | Apoptotic pathway activation; resistance mechanisms | Both (context-dependent) |
| Small molecule inhibitors | COTI-2, Thapsigargin, Erastin | p53 reactivation; calcium modulation; ferroptosis induction | TNBC focus |
| Antibodies for detection | Anti-HER2, Anti-DR-5, Anti-cleaved caspase-3 | Target expression validation; apoptotic status assessment | Both |
| Cell lines | SKBR-3 (HER2+), MDA-MB-231 (TNBC), 4T1 (murine TNBC) | In vitro mechanistic studies; drug screening | Both |
| Animal models | 4T1 syngeneic model, Patient-derived xenografts | Metastatic progression; therapeutic efficacy | Both |
| Molecular biology tools | GAS5 overexpression vectors, miR-378a-5p mimics/inhibitors | lncRNA functional studies; gene regulation mechanisms | TNBC focus |
| Calcium signaling probes | Fura-2AM, Fluo-4 | Store-operated calcium entry measurement; signaling dynamics | TNBC focus |
| Apoptosis detection kits | Annexin V/Pl, TUNEL, Caspase-Glo | Apoptotic quantification and characterization | Both |
HER2-positive and triple-negative breast cancers employ distinct yet equally effective strategies for evading apoptotic cell death, reflecting their fundamentally different molecular identities and pathological behaviors. HER2-positive disease utilizes a coordinated, oncogene-driven program that dominantly suppresses both intrinsic and extrinsic apoptotic pathways through redundant signaling mechanisms. In contrast, TNBC employs a more heterogeneous set of alterations spanning genomic, epigenetic, and metabolic domains, creating a multifaceted apoptotic resistance landscape. The continued elucidation of these subtype-specific mechanisms, particularly in the context of advanced stage IV disease, promises to inform novel therapeutic strategies that specifically target the unique apoptotic vulnerabilities of each subtype. Future research directions should prioritize understanding the temporal evolution of apoptotic resistance during disease progression, developing reliable predictive biomarkers for apoptotic-targeting agents, and designing innovative combination approaches that simultaneously engage multiple cell death pathways to overcome resistance.
Advanced Methodologies for Apoptosis Research: From Biomarker Detection to Therapeutic Application
In stage IV breast cancer, the dysregulation of apoptosis, or programmed cell death, is a hallmark of disease progression and treatment resistance [21]. The core biochemical process of apoptosis involves a cascade of molecular events, primarily executed by caspases and tightly regulated by the TP53 tumor suppressor gene. Modern diagnostic platforms allow researchers to precisely quantify key biomarkers within this pathway, providing critical insights into tumor biology and therapeutic efficacy. This technical guide details the application of Immunohistochemistry (IHC) for detecting cleaved caspases as a direct measure of apoptosis execution, Next-Generation Sequencing (NGS) for identifying TP53 mutations that disrupt apoptotic initiation, and Droplet Digital PCR (ddPCR) for the ultrasensitive quantification of tumor-specific alterations in circulating tumor DNA (ctDNA). Together, these platforms form a powerful toolkit for advancing research into the apoptotic process in advanced breast cancer.
Core Biomarkers and Their Significance
Table 1: Key Apoptosis-Related Biomarkers in Stage IV Breast Cancer Research
| Biomarker | Molecular Function | Significance in Stage IV Breast Cancer | Detection Platform |
|---|---|---|---|
| Cleaved Caspase-3 | Key executioner caspase; cleaves structural and repair proteins, leading to cell death [42] [43]. | Direct marker of ongoing apoptosis; used to study response to chemo-, radio-, and endocrine therapy [21]. | IHC, Western Blot, IF/ICC |
| TP53 Gene | Tumor suppressor; transcription factor that responds to cellular stress (e.g., DNA damage) by inducing cell cycle arrest or apoptosis [44] [21]. | Mutated in ~30% of breast cancers overall and 60-80% of triple-negative breast cancer (TNBC); confers poor prognosis and treatment resistance [45]. | NGS, ddPCR |
| Bcl-2 Family | Regulators of mitochondrial apoptosis; includes pro-apoptotic (e.g., Bax) and anti-apoptotic (e.g., Bcl-2) proteins [21]. | Balance between pro- and anti-apoptotic members determines cell fate. Bcl-2 expression is linked to hormone receptor status [21] [46]. | IHC, qPCR |
| Circulating Tumor DNA (ctDNA) | Cell-free fragmented tumor-derived DNA in blood plasma [47]. | Contains tumor-specific mutations (e.g., in TP53); enables non-invasive "liquid biopsy" for monitoring tumor load and evolution in real-time [47] [48] [45]. | ddPCR, NGS |
Platform 1: Immunohistochemistry (IHC) for Cleaved Caspases
Technical Principle and Workflow
IHC leverages antibody-antigen interactions to visually localize specific proteins, such as cleaved caspase-3, within formalin-fixed paraffin-embedded (FFPE) tissue sections. The detection of the cleaved (activated) form, rather than the full-length protein, provides a specific snapshot of cells undergoing apoptosis.
Detailed IHC Protocol for Cleaved Caspase-3
The following protocol is adapted from commercial antibody datasheets and research publications [42] [43].
- Tissue Preparation: Cut 4-5 µm sections from FFPE breast cancer tissue blocks. Adhere to positively charged slides and dry.
- Deparaffinization and Rehydration: Immerse slides in xylene (or substitute) followed by a graded series of ethanol (100%, 95%, 70%) and finally distilled water.
- Antigen Retrieval: Perform heat-induced epitope retrieval using a pressure cooker or decloaking chamber with Tris-EDTA buffer (pH 9.0) or citrate buffer (pH 6.0) for 20 minutes [42]. Allow slides to cool to room temperature.
- Blocking: Incubate sections with a protein block (e.g., 3% BSA in PBS) for 10-30 minutes to reduce non-specific background staining.
- Primary Antibody Incubation: Apply the anti-cleaved caspase-3 antibody (e.g., Proteintech 25128-1-AP or Cell Signaling Technology #9661) at a recommended dilution of 1:400 in antibody diluent [43]. Incubate overnight at 4°C in a humidified chamber.
- Washing: Rinse slides gently with PBS containing 0.025% Triton X-100 (PBS-T) three times for 5 minutes each.
- Secondary Antibody Incubation: Apply a species-appropriate horseradish peroxidase (HRP)-conjugated polymer secondary antibody for 30-60 minutes at room temperature.
- Detection: Visualize the signal using a chromogen substrate such as 3,3'-Diaminobenzidine (DAB), which produces a brown precipitate at the antigen site. Counterstain with hematoxylin to visualize nuclei.
- Dehydration and Mounting: Dehydrate slides through graded alcohols and xylene, then mount with a permanent mounting medium.
- Analysis: Examine slides under a light microscope. Apoptotic cells will show distinct brown cytoplasmic staining. Quantification can be performed by counting positive cells in multiple high-power fields or by using digital image analysis software.
Figure 1: IHC Workflow for Detecting Cleaved Caspase-3
Research Reagent Solutions
Table 2: Key Reagents for Cleaved Caspase-3 IHC
| Reagent | Function | Example Product / Specification |
|---|---|---|
| Anti-Cleaved Caspase-3 Antibody | Primary antibody that specifically binds to the activated fragment of caspase-3 (Asp175). Does not recognize full-length caspase-3 [42] [43]. | Rabbit monoclonal (CST #9661) or polyclonal (Proteintech 25128-1-AP). |
| Antigen Retrieval Buffer | Unmasks epitopes cross-linked by formalin fixation. | Tris-EDTA (pH 9.0) or Citrate (pH 6.0) buffer. |
| HRP-Labeled Polymer Secondary Antibody | Amplifies signal for detection; conjugated to multiple HRP molecules. | Anti-Rabbit IgG HRP Polymer. |
| DAB Chromogen | Enzyme substrate that produces an insoluble brown precipitate upon reaction with HRP. | 3,3'-Diaminobenzidine tetrahydrochloride. |
Platform 2: Next-Generation Sequencing (NGS) for TP53 Mutations
Technical Principle and Workflow
NGS enables the comprehensive profiling of the TP53 gene across all exons to identify diverse mutation types, including single nucleotide variants (SNVs), insertions-deletions (indels), and copy number variations, which are common in breast cancer [44] [45]. Targeted NGS panels focus sequencing power on TP53 and other cancer-relevant genes, providing deep coverage and high sensitivity for detecting variants, even in samples with low tumor purity.
Detailed NGS Protocol for TP53 Mutation Analysis
This protocol outlines a standard workflow for targeted NGS from FFPE tissue [44] [48] [45].
- DNA Extraction: Isolate high-quality genomic DNA from FFPE breast cancer tissue sections or fresh-frozen tissue using a commercial kit. Quantify DNA using a fluorometric method (e.g., Qubit) and assess quality via spectrophotometry (A260/A280 ratio) or genomic DNA integrity number.
- Library Preparation: Using a targeted NGS panel (e.g., CleanPlex TP53 Panel, AmpliSeq TP53 panel), enzymatically fragment DNA and ligate platform-specific adapter sequences. For FFPE-derived DNA, uracil-DNA glycosylase (UDG) treatment can be incorporated to mitigate deamination artifacts.
- Target Enrichment: Hybridize the library to biotinylated probes designed to capture the entire coding region of TP53. Capture probe-bound fragments using streptavidin-coated magnetic beads.
- Library Amplification: Perform a limited number of PCR cycles to amplify the enriched target libraries.
- Sequencing: Pool uniquely indexed libraries and load onto a sequencer (e.g., Illumina MiSeq/Iseq). Sequence to a high depth of coverage (>1000x mean coverage) to ensure reliable detection of low-frequency variants [48].
- Bioinformatic Analysis:
- Base Calling & Demultiplexing: Generate sequence reads and assign them to individual samples based on their index sequences.
- Alignment: Map sequence reads to the human reference genome (e.g., GRCh38).
- Variant Calling: Use specialized algorithms (e.g., GATK) to identify SNVs and indels relative to the reference. For TP53, it is critical to report all variants down to the limit of detection of the validated assay, as even low-burden mutations can be clinically relevant [49].
- Annotation & Interpretation: Annotate variants with population frequency, in silico pathogenicity predictions (e.g., SIFT, PolyPhen), and clinical databases (e.g., ClinVar). Classify variants according to established guidelines (e.g., IARC TP53 database).
Figure 2: NGS Workflow for TP53 Mutation Analysis
Platform 3: Droplet Digital PCR (ddPCR) for Ultrasensitive Quantification
Technical Principle and Workflow
ddPCR is a highly precise and sensitive method for the absolute quantification of nucleic acid targets without the need for a standard curve. The sample is partitioned into thousands of nanoliter-sized droplets, and PCR amplification occurs within each droplet. After amplification, the platform counts the number of positive and negative droplets for the target sequence, using Poisson statistics to calculate the absolute concentration and variant allele frequency (VAF) of the target in the original sample [47]. This makes it ideal for monitoring TP53 mutations in ctDNA.
Detailed ddPCR Protocol for TP53 Mutation Monitoring
This protocol is adapted from studies monitoring ctDNA in cancer patients [47] [48].
- Blood Collection and Plasma Separation: Collect whole blood in cell-stabilizing tubes (e.g., Streck). Process within 1-6 hours with a double centrifugation protocol (e.g., 1600 x g for 10 min, then 16,000 x g for 10 min) to isolate platelet-poor plasma. Store plasma at -80°C.
- Cell-free DNA (cfDNA) Extraction: Extract cfDNA from 1-5 mL of plasma using a commercial circulating nucleic acid kit. Elute in a low TE buffer or nuclease-free water. Quantify using a sensitive fluorometric assay.
- Assay Design: Design and validate TaqMan probe-based assays specific for the TP53 mutation of interest (based on prior NGS results from the tumor) and a reference gene (e.g., wild-type TP53 or a stable locus on another chromosome).
- Droplet Generation: Combine the extracted cfDNA (typically 1-10 ng) with the ddPCR supermix and mutation-specific assay in a single reaction. Generate droplets using a droplet generator.
- PCR Amplification: Transfer the emulsion to a 96-well plate and run endpoint PCR on a thermal cycler with a standard TaqMan thermal profile.
- Droplet Reading and Analysis: Place the plate in a droplet reader, which flows each droplet individually through a fluorescent detector. The reader classifies each droplet as mutant-positive, wild-type-positive, both (heterozygous), or negative.
- Quantification: The software uses the ratio of mutant-positive droplets to total positive droplets to calculate the variant allele frequency (VAF). The absolute concentration of mutant fragments (copies/µL) is also provided.
Table 3: Comparison of Key Diagnostic Platforms in Apoptosis Research
| Parameter | IHC for Cleaved Caspase-3 | NGS for TP53 | ddPCR for TP53 mt |
|---|---|---|---|
| Primary Information | Protein localization and semi-quantification in tissue context | Comprehensive mutation profiling (SNVs, indels) across entire gene | Absolute quantification of a known mutation |
| Sensitivity | Moderate (depends on antibody and abundance) | High (1-5% VAF, with deeper sequencing possible) | Very High (0.1% VAF and below) [47] |
| Throughput | Medium | High | Medium to High |
| Tissue Requirement | FFPE tissue section | FFPE tissue DNA (10-20 ng) | Plasma cfDNA (1-10 ng) |
| Key Quantitative Output | Apoptotic Index (percentage of positive cells) | Variant Allele Frequency (VAF) for each mutation | Variant Allele Frequency (VAF) and copies/µL |
| Main Application | Assessing apoptotic response to therapy in situ | Discovery of all TP53 mutations in a tumor | Ultrasensitive monitoring of minimal residual disease and treatment response [47] [48] |
Integrated Analysis: Correlating Apoptotic Signaling Data
Interpreting data from these platforms in concert provides a systems-level view of the apoptotic pathway's status in stage IV breast cancer. For example, a tumor with a TP53 mutation (identified by NGS) would be expected to have a diminished capacity to initiate apoptosis in response to DNA damage. This could manifest as a low level of cleaved caspase-3 (by IHC) following chemotherapy, explaining treatment resistance. Furthermore, ddPCR can be used to serially track that specific TP53 mutation in ctDNA, where a rising VAF indicates disease progression or emergence of resistance clones, even before clinical or radiographic signs appear [47] [48] [45]. This multi-platform approach enables researchers to connect genotypic alterations to their functional phenotypic consequences and monitor them dynamically.
Figure 3: Integrated Apoptosis Signaling and Detection Platform Correlation. Mutated TP53 disrupts the pathway, leading to treatment resistance, which can be dynamically monitored via ctDNA.
Liquid Biopsy and Circulating Tumor DNA (ctDNA) for Serial Monitoring of Apoptotic Resistance
In stage IV breast cancer, the dysregulation of apoptotic signaling pathways is a fundamental mechanism driving therapeutic failure and disease progression. The balance between cell proliferation and apoptosis in normal breast cells is disrupted in cancer, leading to uncontrolled cell proliferation, treatment resistance, and cancer cell recurrence [50]. Apoptosis resistance mechanisms increase cancer cell survival and decrease sensitivity to therapeutics, creating a critical need for dynamic monitoring approaches [50]. Liquid biopsy, particularly through analysis of circulating tumor DNA (ctDNA), has emerged as a transformative tool for the serial monitoring of these resistance mechanisms, offering real-time, minimally invasive characterization of tumor dynamics and apoptotic pathway alterations.
ctDNA refers to fragments of free DNA released into the bloodstream by tumor cells undergoing apoptosis or necrosis, carrying tumor-specific genetic alterations that reflect real-time tumor dynamics [51] [52]. This non-invasive approach enables clinicians to monitor disease progression and treatment response dynamically, capturing tumor heterogeneity that traditional tissue biopsies often miss due to sampling constraints [53]. In the context of stage IV breast cancer, serial ctDNA monitoring provides a unique window into the evolving molecular landscape of apoptotic resistance, enabling timely intervention and treatment adaptation.
Molecular Mechanisms of Apoptotic Resistance in Breast Cancer
Genetic and Epigenetic Alterations in Apoptotic Pathways
Breast cancer cells develop resistance to apoptosis through multiple molecular mechanisms, including genetic mutations and epoptotic modifications that reprogram cell death pathways:
- TP53 mutations: The tumor suppressor gene TP53 plays a crucial role in regulating cell survival by inhibiting the PI3K/AKT survival pathway in epithelial tumors. Mutations in p53 are linked to more aggressive breast cancer and poorer overall survival, contributing significantly to apoptotic resistance [50].
- BCL-2 family dysregulation: An inverse correlation exists between the expression of anti-apoptotic BCl-2 and tumor suppressor p53, with increased BCl-2 expression associated with decreased P53 protein activity, promoting cell survival [50].
- Reduced expression of apoptotic proteins: Proteins including KAI1 (CD82), BIF-1 (Bax interacting factor 1), and DNA fragmentation factor 40 (DFF-40) show diminished expression in breast cancer, contributing to evasion of programmed cell death [50].
- Epigenetic modifications: DNA methylation, histone alterations, and dysregulation of non-coding RNAs reprogram gene expression, supporting adaptive resistance mechanisms in breast cancer cells [13].
Tumor Microenvironment and Cancer Stem Cells
The tumor microenvironment (TME) and cancer stem cells (CSCs) play crucial roles in mediating apoptotic resistance:
- Cancer-associated fibroblasts (CAFs) confer resistance to tamoxifen in breast cancer cells via the GPER-integrin β1-mediated pathway, enhancing epithelial-to-mesenchymal transition (EMT) [13].
- Breast cancer stem cells (BCSCs) exhibit multidrug resistance through ABC transporters, robust DNA repair mechanisms, and enhanced apoptotic resistance. Key surface markers of BCSCs include CD44, ALDH1, CD133, EpCAM, ABCG2, GD2, and CXCR4, which promote chemoresistance to multiple therapeutic agents [13].
- Tumor-associated macrophages (TAMs) foster oncogenic responses within the TME by promoting cancer cell proliferation and angiogenesis while suppressing immune responses [13].
Table 1: Key Apoptosis-Regulating Proteins with Altered Expression in Breast Cancer
| Protein | Function | Expression in Breast Cancer | Impact on Apoptosis |
|---|---|---|---|
| KAI1 (CD82) | Metastasis suppressor | Significantly down-regulated | Promotes cell survival and migration |
| BIF-1 | Bax interacting factor | Decreased | Reduces mitochondrial apoptosis |
| DFF-40 | DNA fragmentation factor | Reduced | Impairs DNA degradation in apoptosis |
| BCL-2 | Anti-apoptotic regulator | Increased | Inhibits apoptotic pathway activation |
| Survivin | IAP family member | Overexpressed | Suppresses caspase activity |
Liquid Biopsy Technologies for ctDNA Analysis
ctDNA Detection and Analysis Methods
Multiple advanced technologies have been developed for the isolation and analysis of ctDNA from liquid biopsies, each with specific sensitivities and applications for monitoring apoptotic resistance:
- Droplet digital PCR (ddPCR): Can detect as low as 0.01-1.0% of genomic material and is useful for identifying rare mutations and calculating copy number variants, though it can only evaluate characterized sequences [54].
- Beads, Emulsion, Amplification, and Magnetics (BEAMing): Combines PCR with flow cytometry to detect alterations at levels as low as 0.01% with excellent concordance to tissue testing, ideal for screening known mutations [54].
- Cancer Personalized Profiling by Deep Sequencing (CAPP-Seq): Identifies alterations in ctDNA using large genomic libraries and individual patient sample sequence signatures, capable of identifying multiple mutation types and assessing tumor heterogeneity [54].
- Whole Exome Sequencing (WES): Provides characterization and analysis of all present tumor mutations, enabling identification of potential oncogenes and tumor suppressor genes, though with potentially lower sensitivity than targeted methods [54].
- Whole Genome Bisulfite Sequencing (WGBS-Seq): The gold standard in DNA methylation analysis, providing single cytosine measurement with high accuracy, valuable for detecting epigenetic alterations in apoptotic genes [54].
Advanced Computational Approaches
Recent advances in computational methods have enhanced the sensitivity of ctDNA analysis for monitoring apoptotic resistance:
- Fragle: A deep-learning model that can accurately quantify ctDNA from the density distribution of cell-free DNA-fragment lengths, achieving higher accuracy and lower detection limits than tumor-naive methods. This approach has demonstrated strong concordance between ctDNA dynamics and treatment responses in longitudinal analysis [55].
- Longitudinal monitoring: Serial sampling enables tracking of ctDNA kinetics, providing critical molecular information in real-time that often precedes radiographic evidence of progression or resistance [56] [54].
Table 2: Comparison of ctDNA Detection Technologies for Apoptotic Resistance Monitoring
| Technology | Sensitivity | Advantages | Limitations | Best Application in Apoptosis Monitoring |
|---|---|---|---|---|
| ddPCR | 0.01-1.0% | High sensitivity for known variants; quantitative | Limited to known mutations | Tracking specific apoptotic gene mutations |
| BEAMing | 0.01% | Combines PCR with flow cytometry | Requires known mutations | Monitoring known resistance mutations |
| CAPP-Seq | ~0.1% | Captures tumor heterogeneity; multiple mutation types | Requires design of selector | Comprehensive apoptotic pathway analysis |
| WES | 1-5% | Unbiased; discovers novel alterations | Lower sensitivity; higher cost | Identifying novel apoptotic resistance mechanisms |
| WGBS-Seq | Varies | Comprehensive methylation profiling | DNA degradation affects sensitivity | Epigenetic regulation of apoptotic genes |
Experimental Protocols for Serial Monitoring of Apoptotic Resistance
Longitudinal ctDNA Collection and Processing Protocol
For effective serial monitoring of apoptotic resistance in stage IV breast cancer, standardized protocols for specimen collection, processing, and analysis are essential:
Sample Collection and Processing:
- Collect 10-20 mL of peripheral blood into cell-free DNA collection tubes (e.g., Streck Cell-Free DNA BCT or PAXgene Blood cDNA tubes)
- Process samples within 6 hours of collection at room temperature or within 24-72 hours if refrigerated at 4°C
- Centrifuge at 1600-2000 × g for 10 minutes to separate plasma from blood cells
- Transfer plasma to microcentrifuge tubes and perform a second centrifugation at 16,000 × g for 10 minutes to remove residual cells
- Store plasma at -80°C until DNA extraction or proceed immediately to extraction
Cell-Free DNA Extraction:
- Use commercial cfDNA extraction kits (e.g., QIAamp Circulating Nucleic Acid Kit, Maxwell RSC ccfDNA Plasma Kit)
- Elute cfDNA in low-EDTA TE buffer or nuclease-free water
- Quantify cfDNA using fluorometric methods (e.g., Qubit dsDNA HS Assay)
- Assess DNA quality using capillary electrophoresis (e.g., Agilent 2100 Bioanalyzer with High Sensitivity DNA Kit)
Library Preparation and Sequencing:
- Convert 20-50 ng of cfDNA into sequencing libraries using commercial kits (e.g., Illumina TruSeq Nano, KAPA HyperPrep)
- Amplify libraries with 8-12 PCR cycles depending on input DNA
- Use unique molecular identifiers (UMIs) to reduce sequencing artifacts and improve variant detection
- Enrich for target regions (apoptosis-related genes) using hybrid capture or amplicon-based approaches
- Sequence on appropriate platforms (e.g., Illumina NextSeq, HiSeq, or NovaSeq) to achieve minimum 10,000x coverage
Targeted Gene Panels for Apoptotic Resistance
For focused analysis of apoptotic resistance mechanisms, targeted sequencing panels should include key genes involved in cell death pathways:
Core Apoptosis Genes:
- Extrinsic pathway: FAS, FASLG, FADD, TRADD, CASP8, CASP10
- Intrinsic pathway: BCL2, BAX, BAK1, BID, BAD, BIK, BIM, MCL1
- Execution phase: CASP3, CASP6, CASP7, CASP9
- Regulation: TP53, MDM2, MDM4, XIAP, SURVIVIN (BIRC5)
- Epigenetic regulators: DNMT1, DNMT3A, DNMT3B, TET1, TET2
Breast Cancer-Specific Resistance Genes:
- Hormone resistance: ESR1, PGR, AR
- HER2 signaling: ERBB2, EGFR
- PI3K/AKT/mTOR pathway: PIK3CA, PTEN, AKT1, MTOR
- Cell cycle regulators: CDK4, CDK6, CCND1, RB1
- DNA repair: BRCA1, BRCA2, PALB2, ATM, CHEK2
Data Interpretation and Clinical Correlation
Quantitative Assessment of Apoptotic Resistance
The prognostic significance of ctDNA detection in cancer monitoring is well-established, with quantitative changes providing crucial insights into treatment response and resistance development:
- Baseline ctDNA levels: Patients with detectable baseline ctDNA show significantly poorer overall survival (HR = 1.64, 95% CI = 1.45-1.86, P < 0.001) and worse progression-free survival (HR = 1.42, 95% CI = 1.07-1.89, P = 0.015) compared to those with undetectable ctDNA [51].
- Longitudinal ctDNA monitoring: ctDNA detectability during treatment is strongly associated with poorer OS (HR = 17.22, 95% CI = 4.43-66.89, P < 0.001) and PFS/DFS (HR = 4.16, 95% CI = 2.57-6.73, P < 0.001) [51].
- Early changes in ctDNA: Reduction in ctDNA levels after initiation of therapy correlates with improved clinical outcomes, with studies demonstrating that ctDNA dynamics often precede radiographic changes by several weeks to months.
Integration with Biochemical Apoptosis Markers
Correlation of ctDNA findings with traditional apoptosis biomarkers enhances the understanding of resistance mechanisms:
- Caspase activation markers: Correlate ctDNA findings with circulating levels of activated caspases and caspase cleavage products
- Mitochondrial apoptosis markers: Integrate ctDNA data with measurements of cytochrome c release and mitochondrial membrane potential changes
- Cell death imaging: Combine ctDNA monitoring with apoptosis-specific imaging (e.g., Annexin V PET scans) for comprehensive assessment
Table 3: Correlation Between ctDNA Dynamics and Apoptotic Resistance Mechanisms in Breast Cancer
| ctDNA Finding | Correlated Apoptotic Resistance Mechanism | Potential Therapeutic Intervention |
|---|---|---|
| ESR1 mutations | Altered estrogen receptor signaling with reduced apoptosis | Switch to selective estrogen receptor degraders (SERDs) |
| PIK3CA mutations | Enhanced PI3K/AKT survival signaling | PI3K inhibitors (e.g., alpelisib) |
| TP53 mutations | Disrupted DNA damage-induced apoptosis | PARP inhibitors (in BRCA context) |
| BCL2 amplification | Enhanced anti-apoptotic signaling | BCL2 inhibitors (e.g., venetoclax) |
| Emergent HER2 mutations | Altered growth factor signaling with apoptosis evasion | HER2-targeted therapies |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for ctDNA-Based Apoptotic Resistance Studies
| Reagent/Material | Function | Example Products | Application Notes |
|---|---|---|---|
| Cell-free DNA blood collection tubes | Preserve blood samples for ctDNA analysis | Streck Cell-Free DNA BCT, PAXgene Blood cDNA tubes | Maintain sample integrity for up to 14 days at room temperature |
| cfDNA extraction kits | Isolate cell-free DNA from plasma | QIAamp Circulating Nucleic Acid Kit, Maxwell RSC ccfDNA Plasma Kit | Optimized for low-abundance cfDNA recovery |
| Library preparation kits | Prepare sequencing libraries from cfDNA | Illumina TruSeq Nano, KAPA HyperPrep | Include UMI incorporation for error correction |
| Target enrichment systems | Enrich for apoptosis-related genes | Illumina TruSight Oncology, IDT xGen Pan-Cancer Panel | Custom panels can include apoptosis-specific targets |
| Sequencing platforms | Generate high-throughput sequencing data | Illumina NextSeq 550, NovaSeq 6000 | Adjust coverage based on variant allele frequency expectations |
| ddPCR systems | Absolute quantification of specific variants | Bio-Rad QX200, QX600 | Ideal for tracking known mutations with high sensitivity |
| Bioinformatics tools | Analyze sequencing data for apoptotic resistance | Fragle, CAPP-Seq analysis pipeline | Specialized algorithms enhance sensitivity for ctDNA detection |
Visualizing Apoptotic Resistance Monitoring Workflows
Liquid Biopsy Workflow for Apoptotic Resistance Monitoring
Apoptotic Signaling Pathways and Resistance Mechanisms in Breast Cancer
Liquid biopsy approaches for monitoring apoptotic resistance through ctDNA analysis represent a paradigm shift in the management of stage IV breast cancer. The ability to serially track evolving resistance mechanisms in real-time provides unprecedented opportunities for personalized therapy adaptation and intervention before clinical progression becomes evident. As technologies continue to advance, with improvements in sensitivity through fragmentation-based analyses like Fragle and the development of more comprehensive apoptotic pathway panels, the clinical utility of this approach will expand significantly.
Future directions in this field include the integration of multi-analyte liquid biopsy approaches combining ctDNA with circulating tumor cells, extracellular vesicles, and protein biomarkers to provide a more comprehensive view of apoptotic resistance. Additionally, the development of standardized protocols and analytical frameworks will be essential for translating these research tools into clinically validated tests that can guide therapy decisions and improve outcomes for patients with advanced breast cancer.
Stage IV breast cancer, characterized by metastatic spread to distant organs, remains a formidable therapeutic challenge due to its resistance to conventional treatments. Within this context, the biochemical process of apoptosis, or programmed cell death, represents a critical pathway that, if successfully reactivated, can eliminate malignant cells. Apoptosis evasion is a hallmark of cancer, enabling tumor survival, proliferation, and metastasis [57]. Two principal pathways regulate apoptosis: the extrinsic pathway, initiated by death receptors (e.g., Fas, TNF-R1) on the cell surface, and the intrinsic pathway, governed by mitochondrial membrane integrity and the Bcl-2 protein family [58] [57]. In triple-negative breast cancer (TNBC), an aggressive subtype often diagnosed at advanced stages, dysregulation of these pathways—particularly the overexpression of anti-apoptotic proteins like Bcl-2 and Bcl-XL—is a common mechanism of chemoresistance [59]. This guide provides a comprehensive technical evaluation of natural and synthetic pro-apoptotic compounds, detailing their mechanisms, efficacy, and validation across computational, cellular, and animal models, specifically within the framework of stage IV breast cancer research.
Molecular Mechanisms of Apoptotic Pathways
Core Apoptotic Signaling Pathways
A sophisticated network of protein interactions controls the cellular decision to undergo apoptosis. The following diagram illustrates the major pathways and their intersections, highlighting key targets for pro-apoptotic compounds.
Key Regulatory Proteins and Drug Targets
The Bcl-2 protein family serves as the central gatekeeper of the intrinsic apoptotic pathway. Its members are categorized by their structure and function [58] [57]:
- Multi-domain pro-apoptotic proteins (Bax, Bak, Bok): These proteins directly mediate mitochondrial outer membrane permeabilization (MOMP), leading to cytochrome c release.
- BH3-only pro-apoptotic proteins (Bid, Bim, Bad, Noxa, Puma): These function as sentinels of cellular stress. They either directly activate Bax/Bak or neutralize anti-apoptotic proteins.
- Anti-apoptotic proteins (Bcl-2, Bcl-XL, Mcl-1, Bcl-w): They preserve mitochondrial integrity by binding and inhibiting pro-apoptotic family members.
The balance between these factions determines cellular fate. In cancer, this balance is often tilted toward survival via overexpression of anti-apoptotic proteins [59] [57]. The ratio of pro-apoptotic Bax to anti-apoptotic Bcl-2 is a critical factor in determining a cell's susceptibility to apoptosis, and is a common biomarker assessed in therapeutic studies [60].
Evaluation of Pro-Apoptotic Compounds
Natural Pro-Apoptotic Compounds
Natural products, derived from plants and other organisms, are a rich source of compounds that can modulate apoptotic pathways through multi-target effects, offering unique advantages for cancer therapy [58] [57]. The table below summarizes prominent natural compounds with demonstrated pro-apoptotic activity in breast cancer models.
Table 1: Natural Pro-Apoptotic Compounds and Their Mechanisms of Action
| Compound | Natural Source | Primary Molecular Targets | Observed Effects in Breast Cancer Models | Key References |
|---|---|---|---|---|
| Quercetin | Citrus fruits, onions, green tea [57] | Activates caspase-9, stimulates cytochrome c release [57] | Induces apoptosis in MCF-7 and MDA-MB-231 cells [58] | [58] [57] |
| Curcumin | Curcuma longa (Turmeric) [57] | Upregulates Fas, downregulates AP-1 and β-catenin [57] | Promotes apoptosis; over 100 µM IC50 in various cell lines [58] | [58] [57] |
| Prunus armeniaca (PA) Extract | Apricot [60] | Downregulates Bcl-2, upregulates Bax [60] | Synergistic pro-apoptotic effect with Bee Venom; IC50 35.1 µg/mL in MCF-7 [60] | |
| Bee Venom (BV) | Honeybee [60] | Disrupts cancer cell membranes, inhibits NF-κB/PI3K/AKT [60] | Synergistic with PA; induces membrane blebbing, apoptosis [60] | |
| Resveratrol | Grapes [57] | Targets CD95 signaling pathway, inhibits CDK2 [57] | Induces apoptosis in various cancer types [57] | |
| Aloe-emodin | Rheum species [57] | Generates ROS, upregulates p53 and p21 [57] | Shows efficacy in skin cancer models [57] |
Synthetic Pro-Apoptotic Compounds and Targeted Therapies
Synthetic compounds are designed to specifically target and disrupt key nodes in the apoptotic machinery that are dysregulated in cancer cells.
Table 2: Synthetic Pro-Apoptotic Compounds and Combination Strategies
| Compound / Strategy | Class / Type | Molecular Target | Mechanism of Action | Evidence and Context |
|---|---|---|---|---|
| BH3 Mimetics | Small molecule inhibitor [59] | Anti-apoptotic Bcl-2 proteins (Bcl-2, Bcl-XL, Mcl-1) [59] | Mimics BH3-only proteins, displacing them from anti-apoptotic partners to activate Bax/Bak [59] | Overcomes gemcitabine resistance in TNBC [59] |
| Dual PI3K/mTOR Inhibitors | Small molecule inhibitor [59] | PI3K and mTOR kinases [59] | Inhibits central growth/survival signaling pathway, downregulating AKT, 4EBP1, S6K [59] | Synergistic with BH3 mimetics in TNBC [59] |
| BH3 Mimetic + PI3K/mTOR Inhibitor | Combination Therapy [59] | Bcl-2 family & PI3K/mTOR pathway [59] | Co-operative inhibition to simultaneously trigger apoptosis and block survival signals [59] | Re-sensitizes resistant TNBC tumors, causes significant regression in vivo [59] |
Experimental Models and Methodologies
A Workflow for Apoptosis Evaluation
The evaluation of pro-apoptotic compounds requires a multi-faceted approach, spanning from initial computational predictions to validation in complex living systems. The following workflow outlines the key stages in this process.
Detailed Experimental Protocols
In Vitro Apoptosis Assays
- Cell Culture and Treatment: Use established breast cancer cell lines such as hormone-responsive MCF-7 and triple-negative MDA-MB-231. Culture cells in RPMI-1640 or DMEM supplemented with 10% FBS and antibiotics. Treat cells with varying concentrations of the pro-apoptotic compound (e.g., 0-500 µg/mL for natural extracts) for 24-72 hours [60].
- MTT Viability Assay: Seed cells in 96-well plates (4x10³ cells/well). After treatment, add MTT reagent and incubate for 2-4 hours. Dissolve the resulting formazan crystals in DMSO and measure absorbance at 570 nm. Calculate the half-maximal inhibitory concentration (IC₅₀) using software like GraphPad Prism [60].
- Acridine Orange/Ethidium Bromide (AO/EB) Staining: This dual-fluorescence stain distinguishes live from apoptotic cells. Treat cells, wash with PBS, and stain with AO/EB (10 µg/mL each) for 5-10 minutes. Visualize under a fluorescence microscope: live cells (green), early apoptotic cells (bright green with condensed chromatin), and late apoptotic cells (orange/red) [60].
- Western Blot Analysis: Lyse treated cells in RIPA buffer. Separate proteins (e.g., 40 µg) via SDS-PAGE, transfer to a nitrocellulose membrane, and block with 5% skim milk. Incubate with primary antibodies against Bax, Bcl-2, cleaved caspase-3, cleaved caspase-9, and a loading control like β-actin. Use HRP-conjugated secondary antibodies and an ECL detection system for visualization. Densitometric analysis (e.g., with ImageJ) quantifies protein expression levels [60].
- Colony Formation Assay: Seed a low density of cells (e.g., 500 cells/well in a 6-well plate). Treat for 24 hours, then replace with fresh medium and incubate for 10-14 days. Fix and stain colonies with crystal violet, then count to assess long-term proliferative capacity post-treatment [60].
- Advanced Detection: Imaging Flow Cytometry (IFC): IFC combines microscopy and flow cytometry for high-throughput, single-cell analysis. For automated apoptosis detection, extract features (morphological, spectral) from cell images. Use machine learning for feature selection (e.g., Mutual Information Maximization - MIM) to train a classifier that distinguishes apoptotic from live cells based on these high-dimensional data, moving beyond traditional 2D gating strategies [61].
Distinguishing Apoptosis from Necrosis
A critical step in validation is confirming that cell death occurs via apoptosis. A real-time live-cell imaging method using a FRET-based caspase sensor (e.g., ECFP-DEVD-EYFP) and a stable marker like Mito-DsRed can discriminate the two processes unambiguously [62]:
- Apoptotic Cells: Show a loss of FRET (increase in ECFP/EYFP ratio) due to caspase-mediated cleavage of the probe, while retaining mitochondrial fluorescence.
- Necrotic Cells: Lose the soluble FRET probe due to membrane rupture without a prior ratio change, but retain the mitochondrial marker [62].
In Vivo Validation in Mouse Models
- Xenograft Model Establishment: Subcutaneously inject immunodeficient mice (e.g., NOD/SCID) with 1-5 million human TNBC cells (e.g., MDA-MB-231) suspended in Matrigel. Allow tumors to reach a palpable size (~100 mm³) before randomizing mice into treatment and control groups [59].
- Treatment and Monitoring: Administer the pro-apoptotic compound or vehicle control via oral gavage or intraperitoneal injection. A common schedule is daily dosing for 2-4 weeks. Monitor tumor volume 2-3 times weekly using digital calipers, calculating volume as (length × width²)/2 [59].
- Endpoint Analysis: At the end of the study, euthanize mice and resect tumors for weight measurement and histopathological analysis. Perform immunohistochemistry (IHC) on tumor sections using antibodies against cleaved caspase-3 (apoptosis marker) and Ki-67 (proliferation marker). The TUNEL assay can also be used to label apoptotic cells in situ [59].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Resources for Apoptosis Research
| Reagent / Resource | Function / Application | Example Specification / Target |
|---|---|---|
| MCF-7 Cell Line | ER+ breast cancer model for in vitro studies [60] | ATCC HTB-22 |
| MDA-MB-231 Cell Line | Triple-negative breast cancer model for in vitro studies [60] | ATCC HTB-26 |
| Anti-Bax Antibody | Detection of pro-apoptotic protein by Western Blot [60] | Rabbit monoclonal, Cell Signaling #5023 |
| Anti-Bcl-2 Antibody | Detection of anti-apoptotic protein by Western Blot [60] | Mouse monoclonal, Cell Signaling #15071 |
| Anti-Cleaved Caspase-3 Antibody | Specific detection of activated caspase-3 (IHC/Western) [59] | Rabbit polyclonal, Cell Signaling #9661 |
| FRET Caspase Sensor | Real-time live-cell imaging of caspase activation [62] | pSC1-ECFP-DEVD-EYFP construct |
| Mito-DsRed | Fluorescent labeling of mitochondria for necrosis discrimination [62] | pDsRed-Mito vector |
| Annexin V-FITC / PI Kit | Flow cytometry-based apoptosis/necrosis discrimination | Early (Annexin V+/PI-) vs Late (Annexin V+/PI+) apoptosis |
| Recombinant BH3 Mimetic | Small molecule inhibitor of Bcl-2/Bcl-XL [59] | ABT-263 (Navitoclax) |
| Dual PI3K/mTOR Inhibitor | Inhibitor of key survival signaling pathway [59] | BEZ235 |
The systematic evaluation of pro-apoptotic compounds—from in silico predictions to in vivo validation—provides a robust framework for developing novel therapies for stage IV breast cancer. The synergistic combination of natural compounds, which often employ multi-target strategies, with highly specific synthetic agents like BH3 mimetics and pathway inhibitors, represents a promising frontier. This multi-model approach, leveraging advanced techniques like imaging flow cytometry and real-time caspase imaging, is crucial for unequivocally establishing efficacy and mechanism of action, thereby accelerating the translation of these compelling agents into clinical applications for patients with advanced disease.
ROS-Inducing Agents and Their Mechanism in Triggering Mitochondrial Apoptosis
Within the context of stage IV breast cancer, overcoming resistance to conventional therapies is a paramount challenge in clinical research and drug development. This whitepaper delves into the mechanisms by which reactive oxygen species (ROS)-inducing agents trigger the mitochondrial pathway of apoptosis, a promising avenue for therapeutic intervention. We synthesize current research findings, summarize quantitative data on efficacy, detail key experimental methodologies, and visualize critical signaling pathways. The focus is on providing a rigorous technical resource for researchers and scientists aiming to leverage ROS-mediated apoptosis in the treatment of advanced breast cancer.
Breast cancer is the most commonly diagnosed cancer and a leading cause of cancer mortality in women worldwide [63]. In stage IV, or metastatic breast cancer, the cancer has spread to other parts of the body, making treatment particularly challenging. A critical hurdle is the development of resistance to standard therapies like tamoxifen, a selective estrogen receptor modulator (SERM) [63]. Consequently, identifying alternative or complementary therapeutics is essential.
Apoptosis, or programmed cell death, is a tightly regulated process crucial for maintaining tissue homeostasis. Its dysregulation is a hallmark of cancer, allowing malignant cells to survive and proliferate uncontrollably [21]. The mitochondrial (or intrinsic) pathway of apoptosis is characterized by mitochondrial outer membrane permeabilization (MOMP), leading to the release of cytochrome c into the cytoplasm and the subsequent activation of a cascade of caspases that execute cell death [64].
Reactive oxygen species (ROS), such as superoxide anions and hydrogen peroxide, are natural byproducts of cellular metabolism, primarily generated in the mitochondria [65]. While cancer cells often exhibit higher baseline ROS levels that support their proliferation, a further increase beyond a critical threshold can induce severe oxidative stress, damaging lipids, proteins, and DNA, and ultimately triggering apoptosis [63] [66]. This vulnerability presents a therapeutic opportunity: using pharmacological agents to selectively increase ROS in cancer cells to induce mitochondrial apoptosis.
Mechanisms of ROS-Induced Mitochondrial Apoptosis
The process by which ROS induces mitochondrial apoptosis involves a series of interconnected molecular events, culminating in the disintegration of the cell.
Key Molecular Events
- ROS Generation and Oxidative Stress: Specific agents, including many natural products, can increase ROS production within cancer cells. For instance, the flavonoid Naringenin has been shown to specifically increase mitochondrial superoxide anions and hydrogen peroxide in tamoxifen-resistant (Tam-R) MCF-7 breast cancer cells [63].
- Mitochondrial Membrane Permeabilization: The surge in ROS, particularly from the mitochondria, causes oxidative damage to mitochondrial components. This leads to a loss of mitochondrial membrane potential (ΔΨm), making the membrane "leaky" [63] [67]. The pro-apoptotic protein Bax translocates to the mitochondria, further promoting membrane permeabilization [68].
- Release of Cytochrome c and Caspase Activation: The permeabilized mitochondrial membrane releases cytochrome c into the cytosol. Cytochrome c, in combination with Apaf-1, forms the "apoptosome," which activates caspase-9. Caspase-9 then cleaves and activates executioner caspases, such as caspase-3 and caspase-7, leading to the systematic digestion of cellular components and the hallmark morphological changes of apoptosis, including chromatin condensation and DNA fragmentation [63] [69].
- Regulation by Bcl-2 Family Proteins: The balance between pro-apoptotic (e.g., Bax, Bak) and anti-apoptotic (e.g., Bcl-2, Bcl-xL) proteins determines the cell's fate. Many ROS-inducing agents shift this balance in favor of apoptosis. For example, Isoalantolactone increases the Bax/Bcl-2 ratio, promoting mitochondrial apoptosis [69].
Key Signaling Pathways in Breast Cancer
Research in breast cancer models has identified several key signaling pathways modulated by ROS:
- The CaMKII/Drp1 Pathway: In triple-negative breast cancer (TNBC) cells, a combination of Isorhamnetin and Chloroquine induced ROS, which activated (phosphorylated) Calcium/calmodulin-dependent protein kinase II (CaMKII). Activated CaMKII then phosphorylates Dynamin-related protein 1 (Drp1) at serine 616, prompting its translocation to mitochondria and driving mitochondrial fission, a key step in apoptosis [68].
- The p38/JNK MAPK Pathway: Isoalantolactone was found to induce apoptosis by increasing the protein expression of phosphorylated p38 MAPK and JNK. The apoptosis could be inhibited by specific blockers of these kinases, confirming their role in the cell death process [69].
- Modulation of SIRT1: The same study on Isoalantolactone also identified downregulation of SIRT1, a protein linked to cell survival, as part of its caspase-independent pro-apoptotic mechanism [69].
Table 1: Selected ROS-Inducing Agents and Their Pro-Apoptotic Effects in Breast Cancer Models
| Agent | Class | Model Studied | Key Apoptotic Mechanisms | Experimental EC50/Concentration |
|---|---|---|---|---|
| Naringenin [63] | Flavanone | Tamoxifen-Resistant MCF-7 | ↑ Mitochondrial superoxide & H2O2; ↓ Mitochondrial membrane potential; Activates PARP, caspase-7/9 | 200 µM (chronic treatment) |
| Isorhamnetin [68] | Flavonol | TNBC (MDA-MB-231) | ↑ ROS; Activates CaMKII/Drp1 pathway; Induces mitochondrial fission | Used in combination with Chloroquine |
| Isoalantolactone [69] | Sesquiterpene lactone | MDA-MB-231 & MCF-7 | ↑ ROS; ↑ Bax/Bcl-2 ratio; ↓ ΔΨm; Cytochrome c release; Activates p38/JNK; ↓ SIRT1 | Varies by cell line |
| 18β-Glycyrrhetinic Acid [64] | Triterpenoid | MCF-7 | ↑ Cytochrome c release; Activates caspase-9; ↑ Bax; ↓ Bcl-2 | 100 µM |
Experimental Protocols for Key Assays
To investigate ROS-induced mitochondrial apoptosis, researchers employ a suite of standardized assays. Below are detailed methodologies for core experiments cited in this field.
Annexin V-PE/7-AAD Apoptosis Detection
This flow cytometry-based assay distinguishes early apoptotic, late apoptotic, and necrotic cells.
- Procedure: [63]
- After treatment, harvest cells (e.g., 2.45 × 10^4/plate) and wash with 1x Phosphate Buffer Saline (PBS).
- Resuspend the cell pellet in a staining solution containing Annexin V-PE and 7-AAD (e.g., Guava Nexin reagent).
- Incubate for 20 minutes at room temperature in the dark.
- Analyze fluorescence by flow cytometry (e.g., GuavaCyte) with excitation/emission at 488/530 nm.
- Data Interpretation: Annexin V-positive/7-AAD-negative cells are early apoptotic; Annexin V-positive/7-AAD-positive cells are late apoptotic or necrotic.
MitoSOX Red Mitochondrial Superoxide Detection
This assay specifically measures superoxide anion production within the mitochondria.
- Procedure: [63]
- Harvest and resuspend treated cells in Hank's Balanced Salt Solution (HBSS) containing 5 µM MitoSOX Red dye.
- Incubate for 30 minutes at 37°C.
- Wash cells twice with HBSS to remove excess dye.
- Resuspend in PBS and measure fluorescence immediately using a flow cytometer or fluorescence microplate reader (excitation/emission ~510/580 nm).
- Note: An increase in fluorescence intensity is directly proportional to mitochondrial superoxide production.
Mitochondrial and Cytosolic Fractionation
This protocol allows for the separate analysis of proteins and events in the cytoplasm and mitochondria, such as cytochrome c release.
- Procedure: [68]
- Wash cell pellets twice with cold PBS.
- Resuspend cells in a hypotonic Buffer A (e.g., containing 20 mM HEPES, 10 mM KCl, 1.5 mM MgCl2, 1 mM EDTA, 1 mM EGTA).
- Homogenize cells by passing them 15-20 times through a narrow-gauge needle (e.g., 22-gauge).
- Centrifuge the homogenate at 1,000 g for 10 minutes at 4°C to remove nuclei and unbroken cells.
- Centrifuge the resulting supernatant at 3,500-12,000 g for 10-15 minutes at 4°C. The pellet is the mitochondrial fraction.
- Centrifuge the new supernatant at 100,000+ g for 30-60 minutes at 4°C. The resulting supernatant is the cytosolic fraction.
- The mitochondrial pellet can be washed and lysed. Both fractions can then be analyzed by Western blot for proteins like cytochrome c (cytosolic fraction) and COX IV (mitochondrial marker).
Visualization of Signaling Pathways
Core Pathway of ROS-Induced Mitochondrial Apoptosis
Diagram Title: Core Pathway of ROS-Induced Mitochondrial Apoptosis
Experimental Workflow for Mechanistic Study
Diagram Title: Experimental Workflow for Mechanistic Study
The Scientist's Toolkit: Key Research Reagents
The following table compiles essential materials and reagents used in the featured research to study ROS-induced mitochondrial apoptosis.
Table 2: Essential Research Reagents for Studying ROS-Induced Apoptosis
| Reagent / Assay Kit | Primary Function | Example Application in Research |
|---|---|---|
| MitoSOX Red [63] | Fluorescent probe for selective detection of mitochondrial superoxide. | Quantifying naringenin-induced mitochondrial superoxide in Tam-R cells [63]. |
| CM-H2DCFDA [63] | Cell-permeable dye for detecting general ROS (e.g., H₂O₂, peroxynitrite). | Measuring cumulative intracellular ROS levels after agent treatment [63]. |
| Annexin V Apoptosis Kits [63] [68] | Flow cytometry-based detection of phosphatidylserine externalization, an early apoptosis marker. | Distinguishing early and late apoptotic populations in Isoalantolactone-treated cells [63] [68]. |
| JC-1 Dye | Fluorescent probe for measuring mitochondrial membrane potential (ΔΨm). | Demonstrating loss of ΔΨm, a key event in mitochondrial apoptosis [69]. |
| Cellular Fractionation Kits [68] | Isolate mitochondrial and cytosolic cellular components. | Confirming cytochrome c release from mitochondria into the cytosol [68]. |
| Antibodies: p-CaMKII (T286), p-Drp1 (S616) [68] | Detect activation of key proteins in the ROS-mediated mitochondrial fission pathway via Western blot. | Elucidating the CaMKII/Drp1 mechanism in Isorhamnetin + CQ-induced apoptosis [68]. |
| N-Acetylcysteine (NAC) [69] | Broad-spectrum ROS scavenger and antioxidant. | Used as a control to confirm that the apoptotic effects are specifically due to ROS generation [69]. |
The induction of mitochondrial apoptosis via ROS represents a promising and mechanistically robust strategy for targeting stage IV breast cancer, including resistant and aggressive subtypes. Natural products like naringenin, isorhamnetin, and isoalantolactone provide compelling proof-of-concept by triggering a cascade from mitochondrial ROS generation through to caspase activation. The detailed experimental protocols and key reagents outlined in this whitepaper provide a framework for researchers to validate and explore these mechanisms further. Future work should focus on optimizing the therapeutic window of these agents, exploring synergistic combinations with standard care, and translating these pre-clinical findings into targeted clinical strategies for metastatic breast cancer patients.
Nanotechnology-Based Strategies for Targeted Delivery of Apoptosis-Inducing Agents
Breast cancer, particularly at advanced stages, remains a formidable challenge in oncology due to its capacity to develop resistance to conventional therapies. A pivotal mechanism underlying this resistance is the evasion of programmed cell death, or apoptosis. In stage IV breast cancer, the dysregulation of apoptotic pathways is a hallmark, enabling malignant cells to survive and proliferate despite therapeutic interventions. The biochemical process of apoptosis is tightly controlled by a cascade of signaling events, and its circumvention is a major contributor to treatment failure and disease progression. Recent advancements have focused on leveraging nanotechnology to precisely deliver apoptosis-inducing agents directly to tumor cells, thereby overcoming resistance mechanisms and minimizing systemic toxicity. This whitepaper provides an in-depth technical guide on these innovative strategies, detailing the nanocarrier systems, experimental methodologies, and key reagents essential for researchers and drug development professionals working to reinstate apoptosis in treatment-resistant breast cancer.
Nanocarrier Systems for Apoptosis Induction
Nanocarriers are engineered to exploit the unique pathophysiology of tumors, such as the Enhanced Permeability and Retention (EPR) effect, for passive targeting, and can be functionalized with ligands for active targeting of receptors overexpressed on cancer cells. The following nanocarrier systems have shown significant promise in the targeted delivery of apoptosis-inducing agents [70] [71].
- Liposomes: Spherical vesicles with a hydrophilic core and lipid bilayer, ideal for encapsulating both hydrophilic and hydrophobic drugs. They improve drug solubility and circulation time.
- Niosomes: Non-ionic surfactant-based vesicles similar to liposomes, known for their enhanced stability and cost-effectiveness. They are excellent for co-delivering chemotherapeutic agents [72].
- Polymeric Nanoparticles: Biodegradable polymers (e.g., PLGA) that allow for controlled and sustained drug release. They offer high drug loading capacity and versatility in surface modification.
- Dendrimers: Highly branched, monodisperse macromolecules with numerous surface functional groups for high-density drug loading and targeting ligand attachment.
- Gold Nanoparticles: Inorganic nanoparticles suitable for photothermal therapy and drug delivery. Their surface can be easily functionalized, and they exhibit unique optical properties.
Table 1: Comparison of Key Nanocarrier Systems for Apoptosis Induction
| Nanocarrier Type | Key Components | Mechanism of Delivery | Advantages | Key Challenges |
|---|---|---|---|---|
| Niosomes | Non-ionic surfactants, Cholesterol [72] | Passive targeting (EPR effect), possible active targeting | Improved drug stability, biocompatibility, suitable for co-delivery | Scaling up production, long-term stability |
| Liposomes | Phospholipids, Cholesterol [71] | Passive targeting (EPR effect) | High biocompatibility, FDA-approved formulations (e.g., Doxil) | Rapid clearance by RES, potential leakage |
| Polymeric NPs | PLGA, Chitosan, PEG [71] | Controlled release, active targeting with ligands | Tunable degradation rates, high drug loading | Complexity in polymer synthesis and purification |
| Dendrimers | PAMAM, Poly(propylene imine) | Enhanced permeability, multi-valent targeting | Precise size control, high payload capacity | Potential cytotoxicity at higher generations |
| Gold NPs | Gold core, various coatings (e.g., PEG) | EPR effect, externally guided (e.g., thermal) | tunable, suitable for theranostics | Long-term biodistribution and toxicity concerns |
Quantitative Data from Experimental Studies
The efficacy of nano-delivery systems is validated through a series of in vitro and in vivo assays. The table below summarizes quantitative data from a recent study utilizing niosomes for the co-delivery of cyclophosphamide and sodium oxamate in MDA-MB-231 breast cancer cells [72].
Table 2: Experimental Efficacy Data of Niosome-Mediated Co-Delivery in MDA-MB-231 Cells
| Parameter | Result | Experimental Method | Biological Significance |
|---|---|---|---|
| Niosome Characterization | |||
| Mean Particle Size | 87.98 nm | Dynamic Light Scattering | Ideal for EPR-mediated tumor accumulation |
| Zeta Potential | -7.44 mV | Electrophoretic Light Scattering | Moderate colloidal stability |
| Cell Viability & Cytotoxicity | |||
| Cell Viability Reduction | Significant reduction vs. controls | MTT Assay | Confirms enhanced cytotoxic effect |
| Apoptosis Quantification | |||
| Apoptotic Cells | Substantial increase | Flow Cytometry (Annexin V/PI) | Direct evidence of apoptosis induction |
| Molecular Apoptosis Markers | |||
| Caspase-3 Expression | Increased | Western Blotting | Confirms execution of apoptosis |
| Bax Expression | Increased | Western Blotting | Promotes mitochondrial apoptosis |
| NRF2 Protein Levels | Elevated | Western Blotting | Induced cellular stress response |
Detailed Experimental Protocols
Preparation and Characterization of Niosomes
Method: Thin-Film Hydration Method [72]
- Formation of Thin Film: Dissolve a surfactant (e.g., Span 60), cholesterol, and the drug(s) (e.g., Cyclophosphamide and Sodium Oxamate) in an organic solvent (e.g., chloroform) in a round-bottom flask. Remove the solvent under reduced pressure using a rotary evaporator to form a thin, dry lipid film on the flask wall.
- Hydration: Hydrate the dried lipid film with an aqueous buffer (e.g., phosphate-buffered saline, PBS) at a temperature above the gel-liquid transition temperature of the surfactant. Rotate the flask for approximately 1 hour to allow the film to swell and form multilamellar vesicles.
- Size Reduction: Sonicate the resulting niosome suspension using a probe sonicator or extrude it through polycarbonate membranes of defined pore size (e.g., 200 nm, then 100 nm) to obtain small, unilamellar vesicles with a uniform size distribution.
- Purification: Separate the unentrapped drug by dialysis or centrifugation.
- Characterization:
- Particle Size and Zeta Potential: Analyze using dynamic light scattering (DLS) and electrophoretic light scattering, respectively [72].
- Chemical Structure: Confirm drug encapsulation and excipient compatibility using Fourier-Transform Infrared Spectroscopy (FTIR).
- Entrapment Efficiency: Determine by lysing a known volume of niosomes and quantifying the drug content using a suitable analytical method (e.g., HPLC). Calculate as (Amount of drug entrapped / Total amount of drug used) * 100.
Kinetic Quantification of Apoptosis Using Live-Cell Imaging
Method: Incucyte Live-Cell Analysis Assay [73]
- Cell Seeding: Seed MDA-MB-231 cells in a 96-well or 384-well plate at an optimal density (e.g., 2,000-5,000 cells/well) and allow to adhere for 18-24 hours.
- Treatment and Staining: Treat cells with drug-loaded niosomes and controls. Simultaneously, add a no-wash, mix-and-read apoptosis reagent to the culture medium.
- Option A - Caspase-3/7 Activation: Use Incucyte Caspase-3/7 Dye. This cell-permeant reagent is non-fluorescent until cleaved by activated caspase-3/7, releasing a DNA-binding fluorescent dye (Green/Red/Orange).
- Option B - Phosphatidylserine Exposure: Use Incucyte Annexin V Dye. This reagent binds to phosphatidylserine (PS) exposed on the outer leaflet of the plasma membrane of apoptotic cells, fluorescing upon binding (Red/Green/Orange/NIR).
- Multiplexing (Optional): For concurrent analysis of apoptosis and proliferation/cytotoxicity, co-stain with Incucyte Nuclight Reagents (for nuclear labeling) or Incucyte Cytotox Dyes.
- Real-Time Data Acquisition: Place the plate in the Incucyte Live-Cell Analysis System. Acquire both phase-contrast and fluorescence images every 2-6 hours from the same fields of view for the duration of the experiment (e.g., 72-96 hours).
- Image and Data Analysis: Use integrated software to automatically segment and quantify fluorescent objects (apoptotic cells) and confluence (cell proliferation) in real-time. Kinetic data is presented as fluorescent object count or integrated intensity per image over time.
Molecular Analysis of Apoptotic Pathways
Method: Western Blotting for Apoptotic Proteins [72]
- Protein Extraction: After treatment, lyse MDA-MB-231 cells using RIPA buffer supplemented with protease and phosphatase inhibitors. Centrifuge to remove debris and quantify protein concentration using a BCA or Bradford assay.
- Gel Electrophoresis: Separate equal amounts of protein (20-40 μg) by SDS-PAGE on a polyacrylamide gel (e.g., 12-15%).
- Protein Transfer: Transfer proteins from the gel onto a nitrocellulose or PVDF membrane.
- Blocking and Antibody Incubation: Block the membrane with 5% non-fat milk or BSA in TBST. Incubate with primary antibodies against target proteins (e.g., Cleaved Caspase-3, Bax, Bcl-2, NRF2, β-actin as a loading control) overnight at 4°C.
- Detection: Wash the membrane and incubate with an HRP-conjugated secondary antibody. Detect the signal using a chemiluminescent substrate and visualize with a digital imaging system.
Method: Real-Time PCR (qPCR) for Gene Expression [72]
- RNA Extraction: Isolate total RNA from treated cells using a commercial kit (e.g., TRIzol method).
- cDNA Synthesis: Reverse transcribe 1 μg of RNA into cDNA using a reverse transcriptase kit with oligo(dT) and/or random hexamer primers.
- Amplification: Perform qPCR using gene-specific primers for apoptosis-related genes (e.g., CASP3, BAX, BCL2, NRF2) and a housekeeping gene (e.g., GAPDH, ACTB) with a SYBR Green or TaqMan master mix.
- Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCt) method, normalizing to the housekeeping gene and relative to the control group.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for Apoptosis and Nanotechnology Research
| Reagent / Kit | Function / Application | Key Features |
|---|---|---|
| Incucyte Annexin V Dyes [73] | Kinetic quantification of PS externalization in live cells. | No-wash, mix-and-read protocol; multiplexable with other probes; enables long-term, real-time imaging. |
| Incucyte Caspase-3/7 Dyes [73] | Kinetic measurement of caspase-3/7 enzyme activity in live cells. | Non-fluorescent until cleaved; allows for temporal analysis of apoptotic commitment. |
| Annexin V-FITC/PI Apoptosis Kit (Flow Cytometry) | Standard endpoint detection of early (Annexin V+/PI-) and late (Annexin V+/PI+) apoptosis. | High specificity for PS; compatible with most flow cytometers. |
| MTT Assay Kit [72] | Colorimetric measurement of cell viability and metabolic activity. | Simple, reliable; widely used for initial cytotoxicity screening of nano-formulations. |
| Primary Antibodies for Apoptosis (e.g., vs. Cleaved Caspase-3, Bax, Bcl-2) [72] | Detection of key apoptotic pathway proteins via Western Blotting or Immunocytochemistry. | Validated for specificity; essential for confirming molecular mechanisms. |
| NRF2 Antibody [72] | Detection of NRF2 protein levels, indicating oxidative stress response. | Key for understanding cellular stress pathways induced by treatment. |
Apoptosis Signaling and Nanocarrier Delivery Pathways
The following diagrams illustrate the core biochemical pathway of apoptosis and the mechanism of targeted nano-delivery.
Schematic of Niosome-Mediated Apoptosis Induction
Experimental Workflow for Efficacy Testing
Overcoming Apoptotic Resistance: Mechanisms of Treatment Failure and Strategic Solutions
In stage IV breast cancer, the dysregulation of programmed cell death, or apoptosis, is a cornerstone of disease progression, therapeutic resistance, and ultimately, mortality. Apoptosis is a genetically programmed, ATP-dependent, enzyme-driven mechanism that eliminates cells deemed unnecessary or potentially harmful to the organism [74]. This process maintains tissue homeostasis; however, in cancer, this balance is disrupted. Two of the most critical molecular lesions subverting apoptosis are mutations in the TP53 tumor suppressor gene and the overexpression of various anti-apoptotic proteins [74]. These aberrations enable cancer cells to survive despite internal stress and external insults like chemotherapy. Within the context of stage IV breast cancer, understanding these resistance mechanisms is not merely an academic exercise but a pressing clinical necessity to overcome treatment failure and improve patient outcomes.
Core Molecular Mechanisms of Resistance
TP53 Mutations: The Guardian Compromised
The TP53 gene, encoding the p53 protein, is the most frequently mutated gene in breast cancer, with somatic mutations found in approximately 30% to over 50% of cases [75] [76]. The p53 protein acts as "the guardian of the genome," responding to cellular stress—such as DNA damage—by inducing cell cycle arrest, DNA repair, or, if damage is irreparable, apoptosis [76] [74].
Mechanisms of Oncogenic Subversion: Most TP53 mutations are missense substitutions, leading to the production of a full-length but dysfunctional protein [76]. These mutant p53 proteins not only lose their tumor-suppressive functions but often acquire novel oncogenic activities, a phenomenon referred to as a "gain-of-function" [75]. This includes promoting cancer cell survival, metastasis, and drug resistance. Furthermore, mutant p53 can interfere with innate immune signaling, such as the cGAS-STING-TBK1-IRF3 pathway, thereby enabling tumor immune evasion [75].
Correlation with IHC Patterns and Clinical Aggressiveness: Immunohistochemistry (IHC) can serve as a potential surrogate for TP53 mutation status. Specific staining patterns are strongly associated with different types of mutations [77]:
- Overexpression Pattern: Strong, diffuse nuclear staining in ≥80% of tumor cells is highly associated with missense mutations (88% of cases) [77].
- Null Pattern: A complete absence of nuclear staining in tumor cells (with internal positive control) is predominantly linked to truncating mutations (nonsense, frameshift) (86% of cases) [77]. Breast cancers with a null IHC pattern are significantly associated with a high Nottingham histological grade and a triple-negative phenotype, underscoring the clinical aggressiveness linked to specific TP53 mutation types [77].
Impact on Therapeutic Response: Tumors harboring TP53 mutations are more likely to be aggressive (triple-negative or HER2-positive) and demonstrate resistance to conventional chemotherapy and radiotherapy [76]. The inability to trigger apoptosis in response to DNA-damaging agents is a fundamental driver of this treatment-resistant phenotype.
Anti-Apoptotic Protein Overexpression: Fortifying the Cellular Defenses
A second major axis of apoptotic resistance is the overexpression of anti-apoptotic proteins, which act as critical gatekeepers preventing cell death execution.
The Bcl-2 Family: The Bcl-2 protein family is a key regulator of the intrinsic (mitochondrial) apoptosis pathway. The family includes both pro-apoptotic (e.g., Bax, Bak) and anti-apoptotic (e.g., Bcl-2, Bcl-xL) members [74]. The balance between these factions determines cellular fate. Overexpression of anti-apoptotic proteins like Bcl-2 binds to and inhibits pro-apoptotic activators, thereby preventing mitochondrial outer membrane permeabilization (MOMP). This blocks the release of cytochrome c, a critical step for the activation of the caspase cascade via Apaf-1 and caspase-9 [74].
Inhibitor of Apoptosis Proteins (IAPs): IAPs are a family of proteins that directly inhibit effector caspases, the executioners of apoptosis. They function by binding to caspases and preventing their activation or catalytic activity, thereby acting as a final barrier to cell death [78].
Table 1: Key Anti-Apoptotic Proteins and Their Mechanisms of Action in Breast Cancer
| Protein/Family | Primary Mechanism of Action | Consequence in Overexpression |
|---|---|---|
| Bcl-2 [74] | Binds and inactivates pro-apoptotic proteins like Bax, preventing mitochondrial cytochrome c release. | Inhibits the intrinsic apoptotic pathway, conferring resistance to DNA damage and hypoxia. |
| Other Anti-apoptotic Bcl-2 members (e.g., Bcl-xL, Mcl-1) [74] | Function similarly to Bcl-2, sequestering pro-apoptotic activators. | Contributes to broad-spectrum resistance against chemotherapeutic agents. |
| IAP Family (e.g., XIAP) [78] | Directly binds and inhibits caspase-3, -7, and -9, blocking the execution phase of apoptosis. | Renders cells resistant to both intrinsic and extrinsic death signals. |
Interplay of Resistance Pathways
The pathways of resistance are not isolated. Mutant p53 can transcriptionally repress pro-apoptotic genes and enhance the expression of anti-apoptotic genes, creating a synergistic effect that powerfully suppresses the cell's ability to undergo apoptosis [74]. This convergence on the apoptotic machinery represents a formidable barrier to effective treatment in advanced breast cancer.
Experimental Analysis of Resistance Mechanisms
Detecting Apoptotic Dysregulation: A Multi-Assay Approach
Detecting apoptosis and its dysregulation requires multiple assays due to the process's multi-stage complexity. The table below summarizes key methodologies.
Table 2: Key Experimental Assays for Apoptosis and Resistance Mechanisms
| Target | Assay/Method | Key Reagents & Techniques | Application and Interpretation |
|---|---|---|---|
| TP53 Mutation Status | Next-Generation Sequencing (NGS) [77] | DNA extraction from FFPE tissue, targeted gene panels (e.g., Foundation Medicine, Caris Life Sciences). | Gold standard for identifying specific somatic and germline TP53 mutations. |
| p53 Immunohistochemistry (IHC) [77] | Anti-p53 antibody (e.g., clone BP53-11), Ventana platforms. | Surrogate for mutation status. Interpreted as Overexpression, Null, Wild-type, or Cytoplasmic patterns. | |
| Apoptosis Execution | DNA Fragmentation (TUNEL Assay) [74] | Terminal deoxynucleotidyl transferase (TdT), fluorescent-dUTP, microscopy/flow cytometry. | Labels 3'-OH ends in fragmented DNA; a hallmark of late-stage apoptosis. |
| Caspase Activity [74] | Fluorogenic caspase substrates (e.g., for caspases-3, -8, -9), Western Blot for cleaved substrates (e.g., PARP). | Measures activation of initiator and effector caspases, indicating mid-stage apoptosis. | |
| Mitochondrial Pathway (Intrinsic) | Mitochondrial Membrane Potential [74] | JC-1, TMRM dyes; fluorescence shift indicates loss of potential. | Early marker of intrinsic apoptosis initiation. |
| Cytochrome c Release [74] | Subcellular fractionation, immunofluorescence, Western Blot. | Confirms mitochondrial commitment to apoptosis. | |
| Anti-Apoptotic Protein Expression | Western Blot / Immunoassay [74] | Antibodies against Bcl-2, Bcl-xL, Mcl-1, IAPs. | Quantifies protein levels of key anti-apoptotic regulators. |
| Flow Cytometry (Phosphatidylserine Exposure) [74] | Annexin V-FITC/PI staining. | Distinguishes early apoptotic (Annexin V+/PI-), late apoptotic, and necrotic cells. |
Detailed Protocol: Evaluating p53 Status via IHC and NGS
The following workflow, derived from a 2024 clinical study, outlines a robust method for correlating p53 IHC patterns with TP53 mutation status [77].
- Sample Preparation: Obtain biopsy or surgical excision specimens from primary or metastatic tumor tissue. Fix in formalin and embed in paraffin (FFPE) to create 4 μm thick sections.
- Immunohistochemistry (IHC):
- Perform IHC staining using an automated platform (e.g., Ventana) with an anti-p53 antibody (clone BP53-11).
- Interpretation: Have pathologists independently review slides using a standardized algorithm:
- Wild-type Pattern: Variable staining intensity in <50% of invasive tumor cells.
- Overexpression (OE) Pattern: Strong and diffuse nuclear staining in ≥80% of tumor cells.
- Null-type (NT) Pattern: Complete absence of nuclear staining in tumor cells, with positive internal control (stromal cells).
- Cytoplasmic (CY) Pattern: Strong cytoplasmic staining with absent nuclear staining.
- Equivocal (EV) Pattern: Staining qualitatively and quantitatively greater than wild-type but less than OE.
- Next-Generation Sequencing (NGS):
- Perform DNA extraction from macrodissected FFPE tumor samples.
- Utilize a CLIA-certified NGS platform (e.g., Foundation Medicine, Whole-Exome Sequencing) targeting the entire exon and flanking regions of TP53.
- Analyze sequences for pathogenic/likely pathogenic variants (single nucleotide variants, indels). Exclude variants of uncertain significance (VUS).
- Statistical Correlation: Use Fisher's exact test to determine the association between specific IHC patterns (OE, Null) and TP53 mutation types (missense, truncating). A p-value of <0.05 is considered statistically significant.
TP53 Status Analysis Workflow
Therapeutic Implications and Emerging Strategies
The recognition of these resistance mechanisms has catalyzed the development of targeted therapeutic strategies aimed at re-sensitizing tumor cells to apoptosis.
Targeting Mutant p53: Strategies to reactivate mutant p53 or promote its degradation are actively being explored. Notably, a 2025 study demonstrated that low-dose statins (e.g., lovastatin, fluvastatin) can promote the degradation of mutant p53 proteins in breast cancer cells [75]. This degradation restored innate immune signaling by allowing IRF3 nuclear translocation and enhanced CD8+ T lymphocyte infiltration in mouse models, offering a novel druggable approach for mutant p53 cancers [75].
Targeting Anti-Apoptotic Bcl-2 Proteins: Venetoclax, a specific Bcl-2 inhibitor, has shown remarkable success in hematological malignancies. Its application in solid tumors, including breast cancer, is under investigation, particularly in combination with standard chemotherapy to overcome intrinsic resistance [74].
IAP Antagonists (Smac Mimetics): These compounds are designed to mimic the endogenous IAP inhibitor Smac/DIABLO. By antagonizing IAPs, they free caspases from inhibition and lower the threshold for apoptosis, potentially sensitizing tumors to death receptors and chemotherapeutics [78].
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for researching these resistance mechanisms.
Table 3: Research Reagent Solutions for Apoptosis Resistance Studies
| Reagent/Material | Function/Application | Example Use-Case |
|---|---|---|
| Anti-p53 Antibody (clone DO-1, BP53-11) [75] [77] | Detection of p53 protein expression and pattern analysis via Western Blot and IHC. | Differentiating mutant p53 overexpression (OE) from null patterns in breast cancer cell lines and patient tissues. |
| Phospho-Specific Antibodies (p-TBK1, p-IRF3, p-STING) [75] | Interrogation of innate immune pathway activation status by Western Blot. | Evaluating the restoration of cGAS-STING signaling upon mutant p53 degradation by statins. |
| Annexin V-FITC / Propidium Iodide (PI) [74] | Flow cytometry-based detection of early (Annexin V+/PI-) and late (Annexin V+/PI+) apoptosis. | Quantifying apoptosis induction in breast cancer cells after treatment with chemotherapeutic agents or BH3 mimetics. |
| Caspase Fluorogenic Substrates (e.g., DEVD-AFC for Caspase-3) [74] | Spectrophotometric or fluorometric measurement of caspase enzyme activity. | Determining the point of apoptotic blockade (e.g., pre- or post-mitochondrial) in resistant cell lines. |
| JC-1 Dye (TMRM/TMRE) [74] | Detection of mitochondrial membrane potential (ΔΨm) collapse, an early intrinsic apoptosis event. | Assessing the functional integrity of the mitochondrial pathway in cells overexpressing Bcl-2. |
| Lentiviral shRNA Vectors (e.g., pLKO.1) [75] | Stable knockdown of specific genes (e.g., TP53, STING) in target cells. | Validating the functional role of a specific gene in conferring apoptotic resistance. |
| Statins (e.g., Lovastatin, Fluvastatin) [75] | HMG-CoA reductase inhibitors; used experimentally to induce mutant p53 degradation. | Investigating the re-sensitization of mutant p53 breast cancer cells to innate immune responses and cell death. |
The molecular mechanisms of resistance centered on TP53 mutations and anti-apoptotic protein overexpression represent a critical frontier in the battle against stage IV breast cancer. Their roles in sabotaging the apoptotic machinery are well-established, leading to aggressive, treatment-resistant disease. The ongoing development of sophisticated experimental assays allows researchers to deconstruct these pathways with increasing precision. Furthermore, the emergence of novel therapeutic strategies—from low-dose statins that degrade mutant p53 to BH3 mimetics that neutralize anti-apoptotic proteins—provides a compelling roadmap for future clinical investigation. Overcoming apoptotic resistance holds the key to transforming the therapeutic landscape for patients with advanced breast cancer.
Redox Imbalance and Antioxidant Defense Systems in Chemoresistance
The development of resistance to chemotherapy is a principal obstacle in the management of stage IV breast cancer. This whitepaper delineates the central role of redox imbalance and adaptive antioxidant defense systems in promoting chemoresistance, with a specific focus on the biochemical processes of apoptosis. Tumor cells orchestrate a sophisticated redox regulatory network that maintains reactive oxygen species (ROS) within a pro-survival window, thereby blunting apoptotic signaling and enabling therapeutic evasion. We provide an in-depth analysis of the molecular mechanisms, supported by summarized quantitative data and detailed experimental methodologies for investigating these pathways. Furthermore, this guide outlines emerging therapeutic strategies designed to disrupt this redox balance and resensitize advanced breast cancer to conventional treatments.
In stage IV breast cancer, the dysregulation of programmed cell death is a hallmark of disease progression and treatment failure. The biochemical process of apoptosis, essential for the efficacy of most chemotherapeutic agents, is critically governed by the intracellular redox state. Reactive oxygen species (ROS), including superoxide anion (O₂•⁻), hydrogen peroxide (H₂O₂), and hydroxyl radicals (•OH), function as dual-purpose signaling molecules: at physiological levels, they facilitate survival and proliferation pathways, but at elevated levels, they can induce apoptosis and cell death [79] [80]. Chemoresistant cancer cells exploit this duality by developing robust antioxidant defense systems that maintain ROS within a narrow, pro-tumorigenic range—a state of redox imbalance that favors their survival. This adaptive response effectively raises the threshold for apoptosis initiation, rendering conventional chemotherapy less effective [81] [82]. Understanding the interplay between redox homeostasis, antioxidant defenses, and the apoptotic machinery is therefore paramount for developing novel interventions against incurable, metastatic breast cancer.
Molecular Mechanisms of Redox-Mediated Chemoresistance
The adaptation of breast cancer cells to oxidative stress is multifaceted, involving the upregulation of key transcription factors, antioxidant enzymes, and efflux pumps.
The NRF2-KEAP1 Axis and Antioxidant Response
The NRF2 (Nuclear Factor Erythroid 2-Related Factor 2) pathway is a master regulator of cellular antioxidant responses. Under normal conditions, NRF2 is bound by its inhibitor, KEAP1, and targeted for proteasomal degradation. Under oxidative stress, this interaction is disrupted, allowing NRF2 to translocate to the nucleus and bind to the Antioxidant Response Element (ARE), initiating the transcription of a battery of cytoprotective genes [79] [80]. In breast cancer, constitutive activation of NRF2 is a common mechanism of chemoresistance.
- Target Genes: NRF2 upregulates genes encoding for glutathione (GSH)-synthesizing enzymes, glutathione peroxidase (GPX), and NADPH quinone dehydrogenase 1 (NQO1) [79].
- Clinical Impact: Elevated NRF2 activity maintains redox homeostasis, protecting cancer cells from chemotherapy-induced oxidative damage and apoptosis. A recent study identified a circular RNA, cDTL, which stabilizes NRF2 and promotes the transcription of SLC7A11, a critical subunit of the System Xc⁻ cystine/glutamate antiporter, thereby enhancing the GSH/GPX4 axis and suppressing ferroptosis—a ROS-induced cell death pathway [83].
Key Antioxidant Enzymes and Their Roles
Cancer cells bolster their antioxidant capacity through the coordinated action of several enzymes, as detailed in Table 1.
Table 1: Key Antioxidant Enzymes in Breast Cancer Chemoresistance
| Enzyme | Function | Role in Breast Cancer Chemoresistance |
|---|---|---|
| Superoxide Dismutase (SOD) | Catalyzes the dismutation of superoxide (O₂•⁻) to hydrogen peroxide (H₂O₂) and oxygen [79]. | SOD1 is overexpressed in ErbB2-positive breast cancer, supporting proliferation under high ROS conditions. SOD2 (Mn-SOD) exhibits a dual role, acting as a tumor suppressor early in carcinogenesis but promoting metastasis in advanced disease [26] [80]. |
| Catalase (CAT) | Converts H₂O₂ into water and oxygen, preventing the formation of highly reactive hydroxyl radicals [26]. | Associated with the luminal B subtype. Overexpression in MCF-7 cells reduces sensitivity to anticancer treatments [26]. |
| Glutathione Peroxidase 4 (GPX4) | Utilizes glutathione (GSH) to reduce lipid hydroperoxides, thereby preventing the iron-dependent cell death pathway, ferroptosis [26] [8]. | Highly expressed in breast cancer stem cells (CSCs) and the luminal androgen receptor (LAR) subtype of TNBC. GPX4 inhibition synergizes with immunotherapy in TNBC models [26] [8]. |
| Glutathione Reductase (GR) | Regenerates reduced glutathione (GSH) from its oxidized form (GSSG), maintaining the intracellular GSH pool [26]. | Elevated GR activity in MCF-7 cells is associated with increased resistance to radiotherapy [26]. |
ATP-Binding Cassette (ABC) Transporters and Drug Efflux
A non-antioxidant but critically related resistance mechanism involves the overexpression of ABC transporters. Proteins such as ABCC1 (MRP1) and ABCG2 (BCRP) utilize ATP to efflux a wide range of chemotherapeutic agents (e.g., anthracyclines, taxanes) from the cell, reducing intracellular drug accumulation and thus, apoptosis induction [81]. Notably, ABCC1, ABCG2, and ABCC11 are expressed more frequently and at higher levels in triple-negative breast cancer (TNBC) compared to other subtypes [81] [84]. The hedgehog signaling pathway can further upregulate these transporters, compounding the resistance phenotype [81].
Experimental Protocols for Assessing Redox Status and Apoptosis
To investigate redox-mediated chemoresistance, researchers employ a suite of biochemical and molecular techniques. The following protocols provide a framework for key experiments.
Protocol: Measuring Intracellular ROS and Glutathione Levels
Objective: To quantify the levels of reactive oxygen species and the reduced glutathione (GSH) to oxidized glutathione (GSSG) ratio in chemosensitive vs. chemoresistant breast cancer cell lines.
Materials:
- Cell Lines: Chemosensitive (e.g., MCF-7) and chemoresistant (e.g., MCF-7/ADR) breast cancer cells.
- ROS Probe: CM-H₂DCFDA (5-(and-6)-chloromethyl-2',7'-dichlorodihydrofluorescein diacetate, acetyl ester).
- GSH/GSSG Assay Kit: Commercially available kit (e.g., from Cayman Chemical or Sigma-Aldrich).
- Inducer: Tert-butyl hydroperoxide (t-BOOH) as a positive control for oxidative stress.
- Equipment: Flow cytometer or fluorescence microplate reader.
Methodology:
- Cell Culture and Treatment: Seed cells in 6-well or 96-well plates and allow to adhere for 24 hours. Treat with a chemotherapeutic agent (e.g., 1 µM Doxorubicin) or vehicle control for 6-24 hours.
- ROS Measurement:
- Wash cells with PBS and load with 10 µM CM-H₂DCFDA in serum-free media for 30-45 minutes at 37°C.
- Wash cells twice with PBS to remove excess probe.
- Analyze fluorescence immediately (Ex/Em: 495/529 nm) via flow cytometry or a fluorescence plate reader. Include t-BOOH-treated cells as a positive control.
- GSH/GSSG Ratio Measurement:
- Harvest cells by trypsinization and lyse according to the manufacturer's protocol for the GSH/GSSG assay kit.
- The assay typically involves a enzymatic recycling method using glutathione reductase and DTNB (5,5'-dithio-bis-(2-nitrobenzoic acid)). The total glutathione (GSH+GSSG) and GSSG levels are measured in separate reactions.
- Calculate the GSH/GSSG ratio: (Total Glutathione - 2*GSSG) / GSSG.
Data Interpretation: Chemoresistant cells are expected to exhibit lower baseline ROS and a higher GSH/GSSG ratio compared to their chemosensitive counterparts, indicating a more reduced intracellular environment and enhanced antioxidant capacity [79] [80].
Protocol: Evaluating Apoptosis via Caspase-3/7 Activity and TUNEL Assay
Objective: To quantitatively assess the induction of apoptosis in response to chemotherapy, with and without inhibition of antioxidant defenses.
Materials:
- Caspase-Glo 3/7 Assay System: A luminescent assay for caspase-3 and -7 activity (Promega).
- TUNEL Assay Kit: For in situ detection of DNA fragmentation (e.g., Roche Applied Science).
- Inhibitor: Erastin (10 µM) or ML210 (1 µM) to inhibit System Xc⁻ or GPX4, respectively, to induce ferroptosis as a comparative cell death modality [26] [8].
Methodology:
- Caspase-3/7 Activity Assay:
- Seed cells in a white-walled 96-well plate. After treatment with chemotherapeutic agents ± antioxidant inhibitors, add an equal volume of Caspase-Glo 3/7 reagent to each well.
- Incubate for 30-60 minutes at room temperature and measure luminescence. Luminescence is proportional to caspase activity.
- TUNEL (Terminal deoxynucleotidyl transferase dUTP nick end labeling) Assay:
- Culture cells on glass coverslips. After treatments, fix cells with 4% paraformaldehyde and permeabilize with 0.1% Triton X-100.
- Follow the manufacturer's protocol to label nicked DNA ends with fluorescently-tagged dUTP.
- Counterstain nuclei with DAPI and visualize under a fluorescence microscope. Apoptotic cells display bright nuclear fluorescence.
Data Interpretation: Co-treatment with antioxidant inhibitors (e.g., Erastin) should sensitize chemoresistant cells, leading to a significant increase in caspase-3/7 activity and TUNEL-positive cells following chemotherapy exposure [21] [82] [8]. This demonstrates the functional link between redox inhibition and apoptosis restoration.
Visualization of Key Signaling Pathways
The following diagram illustrates the core molecular pathways through which breast cancer cells achieve redox homeostasis to evade apoptosis, integrating the NRF2 antioxidant response, the GPX4-ferroptosis axis, and drug efflux mechanisms.
Diagram Title: Redox Homeostasis Network in Chemoresistant Breast Cancer
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs critical reagents for probing redox imbalance and chemoresistance mechanisms in breast cancer models.
Table 2: Research Reagent Solutions for Studying Redox-Mediated Chemoresistance
| Reagent / Tool | Category | Function in Research |
|---|---|---|
| CM-H₂DCFDA | Fluorescent Probe | Measures general intracellular ROS levels, particularly H₂O₂ [26]. |
| Erastin | Small Molecule Inhibitor | Inhibits System Xc⁻, depleting glutathione and inducing ferroptosis [26] [8]. |
| RSL3 | Small Molecule Inhibitor | Directly binds to and inhibits GPX4, triggering ferroptosis [26] [8]. |
| ML385 | Small Molecule Inhibitor | Blocks the NRF2-KEAP1 interaction, inhibiting the NRF2-mediated antioxidant response [79]. |
| siRNA/shRNA vs. cDTL | Molecular Tool | Knockdown of the oncogenic circular RNA cDTL to sensitize cells to ferroptosis [83]. |
| Caspase-Glo 3/7 Assay | Bioluminescent Assay | Quantifies the activity of executioner caspases-3 and -7 as a key metric of apoptosis [82]. |
| TUNEL Assay Kit | Histochemical / Fluorescent Assay | Detects DNA fragmentation, a late-stage marker of apoptosis, in fixed cells or tissue sections [21]. |
| GSH/GSSG-Glo Assay | Luminescent Assay | Specifically and quantitatively measures the ratio of reduced to oxidized glutathione [26]. |
Targeting the redox-adaptation of breast cancer cells presents a promising avenue for overcoming chemoresistance. Current investigative strategies include:
- Ferroptosis Inducers: Agents like Erastin and RSL3 are being explored to selectively kill apoptosis-resistant cells, particularly in TNBC and HER2-positive subtypes. Their synergy with chemotherapy (e.g., paclitaxel) and immunotherapy (e.g., PD-1 inhibitors) is a major focus [26] [8].
- NRF2 Pathway Inhibitors: Compounds such as ML385 aim to blunt the enhanced antioxidant response, making cancer cells more vulnerable to oxidative stress-induced apoptosis [79].
- Nanoparticle-Based Delivery: Nanocarriers are being engineered to co-deliver chemotherapeutic drugs and ROS-amplifying agents or antioxidant inhibitors directly to tumor cells, overcoming drug efflux and improving efficacy while reducing systemic toxicity [26] [84].
- ABC Transporter Modulators: While early-generation inhibitors faced toxicity challenges, novel approaches using natural products, TKIs at high doses, and siRNA to silence transporter expression are under investigation [81].
In conclusion, the failure of apoptosis in stage IV breast cancer is intimately linked to the successful adaptation of tumor cells to maintain a redox equilibrium that favors survival. A deep understanding of the components of this system—from the NRF2 transcription factor and antioxidant enzymes like GPX4 to efflux pumps and regulatory non-coding RNAs—provides a clear roadmap for therapeutic intervention. Disrupting this precise redox balance represents a viable and potent strategy to resensitize advanced, treatment-refractory breast cancer to established and emerging therapies.
The Impact of Tumor Microenvironment and Epigenetic Regulation on Cell Death Evasion
In stage IV breast cancer, the evasion of programmed cell death, or apoptosis, represents a fundamental biochemical process driving therapeutic resistance and metastatic progression. This complex phenomenon is not solely an intrinsic property of cancer cells but is orchestrated through dynamic crosstalk between the tumor microenvironment (TME) and epigenetic regulatory mechanisms [85] [13]. The TME creates a protective niche that shields tumor cells from apoptotic signals, while epigenetic modifications reprogram gene expression networks to enhance survival. Understanding this interplay is critical for developing novel therapeutic strategies to overcome treatment resistance in advanced breast cancer.
The biochemical process of apoptosis evasion in this context involves the concerted dysregulation of both extracellular signals from the TME and intracellular epigenetic controls. Cancer cells within the TME receive survival signals from various cellular components, including immune cells and cancer-associated fibroblasts, which activate anti-apoptotic pathways [13] [86]. Concurrently, epigenetic mechanisms such as DNA methylation and histone modifications silence pro-apoptotic genes and reinforce survival programs without altering the DNA sequence itself [85] [87] [88]. This multi-layered regulation presents a significant challenge in stage IV disease, where traditional therapies often fail to induce sufficient cancer cell death.
The Tumor Microenvironment: Architecture of Survival
Cellular Components and Their Roles in Apoptosis Evasion
The breast TME is a highly organized ecosystem comprising diverse cellular components that collectively promote cancer cell survival and resistance to cell death. Each cell type contributes uniquely to creating an immunosuppressive and pro-survival milieu through direct cell-cell interactions and paracrine signaling.
Table 1: Cellular Components of the Breast Tumor Microenvironment and Their Roles in Apoptosis Evasion
| Cell Type | Subtypes/Phenotypes | Mechanisms in Apoptosis Evasion | Impact on Stage IV Disease |
|---|---|---|---|
| Tumor-Associated Macrophages (TAMs) | M1 (anti-tumor), M2 (pro-tumor) | M2 TAMs secrete IL-10, TGF-β, and CCL18; induce Treg cells; promote angiogenesis via VEGF [86] | Correlates with poor prognosis; associated with metastasis in TNBC [86] |
| Cancer-Associated Fibroblasts (CAFs) | Multiple subtypes including CD63+, CD10+GPR77+ | Confer tamoxifen resistance via GPER-integrin β1 pathway; secrete exosomal miR-22 downregulating ERα and PTEN [13] | Promotes resistance to endocrine therapy and chemotherapy [13] |
| Myeloid-Derived Suppressor Cells (MDSCs) | Polymorphonuclear (PMN-MDSC), Monocytic (M-MDSC) | Suppress CD8+ T cell function; promote Treg expansion; generate reactive oxygen species [86] [89] | Contributes to immunotherapy resistance; elevated in advanced disease |
| Regulatory T Cells (Tregs) | CD4+CD25+FOXP3+ | Suppress effector T cell function through IL-2 consumption and CTLA-4 mediated inhibition [89] | Creates immunosuppressive environment permissive for metastasis |
| Cancer Stem Cells (CSCs) | ALDH1+, CD44+CD24- | Upregulate MDR transporters; enhance DNA repair capacity; resist apoptotic signaling [13] | Drives recurrence and therapeutic resistance after initial response |
Beyond these cellular interactions, the TME establishes a physical and biochemical barrier against apoptosis through multiple mechanisms. Immune cells within the TME predominantly adopt immunosuppressive phenotypes, effectively protecting cancer cells from immune-mediated destruction [86]. TAMs, which constitute a substantial portion of the TME, predominantly exhibit the M2 phenotype in breast cancer, secreting cytokines that promote cancer cell survival and dissemination [86]. Similarly, CAFs activate numerous signaling pathways including JAK/STAT3, PI3K/Akt, and NF-κB to promote resistance to targeted therapies like trastuzumab in HER2-positive breast cancer [13]. The metabolic reprogramming within the TME further compromises immune cell function while supporting cancer cell survival, creating a environment where apoptosis is strongly suppressed [89].
Hypoxia and Metabolic Reprogramming
Hypoxia represents a critical feature of the TME that profoundly influences apoptosis evasion in stage IV breast cancer. As tumors grow beyond their vascular supply, oxygen deprivation triggers stabilization of Hypoxia-Inducible Factor 1-alpha (HIF1α), which coordinates multiple adaptive responses [90]. HIF1α-mediated mechanisms include metabolic reprogramming, immune evasion, and treatment resistance, making it a central regulator of the apoptotic threshold in advanced disease [90].
The metabolic landscape of the TME further reinforces apoptosis resistance through nutrient competition and metabolic byproducts. Tumor cells undergo metabolic reprogramming to support their rapid proliferation while simultaneously creating a hostile environment for immune effector cells. Competitive consumption of amino acids such as tryptophan and arginine compromises immune cell function, promoting immune escape [89]. This metabolic adaptation not only provides cancer cells with necessary building blocks but also actively suppresses apoptotic pathways through redox regulation and energy sensing mechanisms.
Epigenetic Mechanisms Governing Cell Death Evasion
DNA Methylation and Apoptotic Pathway Silencing
DNA methylation represents a fundamental epigenetic mechanism that promotes apoptosis evasion in breast cancer through the transcriptional silencing of tumor suppressor genes and pro-apoptotic factors. This process involves the covalent addition of methyl groups to cytosine residues within CpG islands, primarily catalyzed by DNA methyltransferases (DNMTs) [85] [88]. In stage IV breast cancer, hypermethylation of key regulatory genes establishes a robust anti-apoptotic program that enhances survival and therapeutic resistance.
The patterns of aberrant DNA methylation in advanced breast cancer are not random but specifically target critical pathways governing cell death. Key tumor suppressor genes such as BRCA1, p16, and RASSF1A frequently exhibit promoter hypermethylation in breast cancer, leading to their transcriptional silencing [85]. This hypermethylation directly promotes cell proliferation, inhibits apoptosis, and facilitates tumor formation and progression. Research has shown that hypermethylation of the BRCA1 promoter occurs in up to 30% of sporadic breast cancer cases, significantly reducing gene expression [85]. Similarly, hypermethylation of the p16 gene is associated with unlimited proliferation of breast cancer cells through dysregulation of cell cycle control [85]. The cumulative effect of these methylation events is the establishment of an epigenetic landscape that strongly resists apoptotic signals.
Table 2: Key Epigenetically Silenced Genes in Breast Cancer and Their Roles in Apoptosis Regulation
| Gene | Epigenetic Modification | Function in Apoptosis | Therapeutic Implications |
|---|---|---|---|
| BRCA1 | Promoter hypermethylation [85] | DNA damage repair; cell cycle checkpoint control [13] | Hypermethylation in 30% of sporadic BC; associated with TNBC [85] |
| p16 | Promoter hypermethylation [85] | Cell cycle regulation; CDK inhibitor | Linked to unlimited BC cell proliferation [85] |
| RASSF1A | Promoter hypermethylation [85] | Pro-apoptotic signaling; microtubule stability | Promotes tumor proliferation and metastasis [85] |
| GADD45a | Methylation-sensitive transcript [91] | Growth arrest and DNA damage response | Potential biomarker for treatment response [91] |
| BRMS1 | DNA hypermethylation [91] | Metastasis suppression | Associated with metastatic progression in TNBC [91] |
The regulation of DNA methylation is particularly crucial in triple-negative breast cancer (TNBC), where epigenetic patterns are differentially regulated across subtypes and significantly impact antitumor immune responses and drug effectiveness [87]. In mesenchymal TNBC, modifying these methylation patterns can alter drug sensitivity, presenting a promising strategy for enhancing therapy outcomes. The dynamic nature of DNA methylation also allows for potential reversibility, making it an attractive target for epigenetic therapies aimed at restoring apoptotic sensitivity in treatment-resistant disease [87] [88].
Histone Modifications and Chromatin Remodeling
Histone modifications represent another layer of epigenetic control that governs apoptosis evasion in stage IV breast cancer through regulation of chromatin accessibility and gene expression. These covalent post-translational modifications, including methylation, acetylation, and phosphorylation, occur predominantly on the N-terminal tails of histone proteins and determine the transcriptional status of genomic regions [85] [92]. The balance between activating and repressive histone marks directly influences the expression of genes critical for apoptosis execution.
Among the various histone modifications, methylation of histone H3 at lysine 27 (H3K27me3) serves as a prominent repressive mark that silences tumor suppressor genes in breast cancer. This modification is catalyzed by Enhancer of Zeste Homolog 2 (EZH2), the catalytic subunit of the Polycomb Repressive Complex 2 (PRC2) [85]. In breast cancer cells, H3K27me3 levels are significantly elevated at the promoter regions of tumor suppressor genes like BRCA1, leading to chromatin compaction and transcriptional repression [85]. Similarly, histone deacetylation mediated by histone deacetylases (HDACs) creates a condensed chromatin state that limits access to pro-apoptotic genes. The coordinated action of these modifications establishes an epigenetic barrier against apoptosis that complements genetic alterations in advanced disease.
The interplay between histone modifications and nuclear receptor signaling further reinforces apoptosis resistance in hormone receptor-positive breast cancers. Upon estrogen stimulation, ERα recruits a cohort of coactivators with histone-modifying activities to target genes, including members of the p160 family, p300/CBP, and SWI/SNF chromatin remodeling complex [92]. p300, a histone acetyltransferase, is recruited to ERα-bound enhancers where it acetylates H3K27, activating enhancer elements and promoting transcription of survival genes [92]. Concurrently, ERα can also recruit corepressors including NCoR1, NCoR2, and LCoR that bring epigenetic repressors to downregulate E2-repressed genes, including pro-apoptotic factors [92]. This sophisticated regulation of the chromatin landscape enables cancer cells to fine-tune their transcriptional programs to evade cell death across diverse therapeutic contexts.
Non-Coding RNAs in Apoptosis Regulation
Non-coding RNAs, particularly microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), have emerged as critical regulators of apoptosis evasion in stage IV breast cancer through their ability to fine-tune gene expression networks. These RNA molecules do not encode proteins but exert powerful regulatory effects on cellular processes, including cell death pathways, through post-transcriptional mechanisms and chromatin interactions.
miRNAs function as post-transcriptional regulators that typically promote mRNA degradation or translational repression of target genes. In breast cancer, specific miRNA profiles are associated with tumorigenesis, progression, and metastasis [88]. Tumor suppressor miRNAs such as miR-4458 are frequently suppressed, while oncogenic miRNAs including miR-214 are upregulated, leading to manifestation of cancer hallmarks including apoptotic resistance [88]. Similarly, lncRNAs such as GAS5, which normally acts as a tumor suppressor by regulating various tumor suppressor proteins including PTEN, PDCD4, and FOXO1, are markedly downregulated in breast cancer, often through promoter methylation in triple-negative breast cancer [88]. The dysregulation of these non-coding RNA networks creates an environment permissive for cancer cell survival and represents a promising target for therapeutic intervention.
Experimental Approaches for Investigating TME-Epigenetics Crosstalk
Methodologies for Epigenetic Profiling in the TME Context
Investigating the interplay between the TME and epigenetic regulation requires sophisticated methodological approaches that can capture the complexity of these interactions. Key technologies enable researchers to decipher the epigenetic landscape within specific cellular components of the TME and correlate these findings with functional outcomes in apoptosis evasion.
Chromatin Immunoprecipitation Sequencing (ChIP-Seq) represents a powerful method for mapping histone modifications and transcription factor binding across the genome. This technique involves cross-linking proteins to DNA, immunoprecipitating the protein-DNA complexes with specific antibodies, and high-throughput sequencing of the bound DNA fragments. When applied to breast cancer models, ChIP-Seq can reveal how histone modification patterns differ between cancer cells and TME components, and how these patterns change in response to therapeutic pressure [92]. For example, ChIP-Seq for H3K27ac can identify active enhancers regulated by TME-derived signals, while H3K27me3 profiling can reveal silenced tumor suppressor genes.
DNA Methylation Analysis through whole-genome bisulfite sequencing or array-based approaches provides comprehensive mapping of methylated cytosines throughout the genome. This methodology allows researchers to identify promoter hypermethylation events that silence pro-apoptotic genes in response to TME-derived signals [85] [87]. The detection of aberrant methylation patterns can also serve as biomarkers for predicting therapeutic response and disease progression. Advanced techniques now enable methylation profiling from liquid biopsy samples, allowing non-invasive monitoring of epigenetic changes throughout treatment [85].
Single-Cell Multi-Omics Technologies represent a cutting-edge approach for deconvoluting the heterogeneity of the TME and its epigenetic states. These methods allow simultaneous measurement of epigenetic features, gene expression, and protein markers in individual cells, providing unprecedented resolution of the cellular ecosystem in breast cancer [90]. By applying single-cell ATAC-Seq and RNA-Seq to patient samples, researchers can identify distinct epigenetic programs in cancer cells, immune cells, and stromal components, and track how these programs evolve during metastasis and treatment resistance.
Functional Validation of Epigenetic Targets
Once candidate epigenetic mechanisms of apoptosis evasion have been identified, rigorous functional validation is essential to establish causal relationships and therapeutic potential. Both in vitro and in vivo approaches provide complementary information for target credentialing.
Table 3: Key Experimental Approaches for Functional Validation of Epigenetic Mechanisms
| Methodology | Application | Key Output Measures | Considerations for TME Context |
|---|---|---|---|
| CRISPR-Cas9 Epigenome Editing | Targeted epigenetic manipulation | Gene expression changes; apoptosis sensitivity | Enables precise editing without DNA sequence alteration [87] |
| Epidrug Screening | Testing DNMTis, HDACis, EZH2 inhibitors | IC50 values; combination indices with standard therapies | Assess effects on both cancer cells and TME components [87] [88] |
| 3D Co-culture Models | Modeling TME interactions | Invasion; colony formation; apoptosis markers | Incorporates multiple cell types; more physiologically relevant [13] |
| Patient-Derived Organoids | Maintaining tumor heterogeneity | Drug response; biomarker discovery | Preserves original TME architecture and cellular diversity [13] |
| In Vivo Metastasis Models | Studying stage IV disease progression | Metastatic burden; survival; therapy response | Provides systemic context of metastatic niche [13] |
For in vitro validation, CRISPR-based epigenome editing enables precise manipulation of specific epigenetic marks at defined genomic loci without altering the underlying DNA sequence. This approach can establish causal relationships between specific histone modifications or DNA methylation events and apoptosis sensitivity. When combined with co-culture systems that incorporate relevant TME components such as CAFs or immune cells, researchers can dissect how extracellular signals from the TME influence the epigenetic regulation of apoptosis pathways in cancer cells [13].
In vivo validation remains essential for understanding how epigenetic mechanisms operate within the complex physiological context of stage IV breast cancer. Patient-derived xenograft (PDX) models that maintain the original tumor heterogeneity and stromal components provide valuable platforms for testing epigenetic therapies and their effects on apoptosis induction [13]. These models allow researchers to monitor how epidrugs influence not only cancer cells but also the composition and function of the TME, and how these changes ultimately impact metastatic progression and treatment response.
Therapeutic Implications and Clinical Translation
Targeting the Epigenetic-TME Axis
The intricate crosstalk between the TME and epigenetic regulation in apoptosis evasion presents promising therapeutic opportunities for stage IV breast cancer. Epidrugs - pharmaceutical agents targeting epigenetic modifiers - can potentially reverse the survival advantages gained by cancer cells and sensitize them to conventional therapies [87] [88]. These agents target the enzymatic machinery responsible for writing, reading, or erasing epigenetic marks, thereby reprogramming the cancer epigenome toward a more therapeutic-sensitive state.
The most advanced epigenetic therapies in breast cancer include DNA methyltransferase inhibitors (DNMTis) and histone deacetylase inhibitors (HDACis), which aim to reverse the silencing of tumor suppressor genes and restore apoptotic sensitivity [87] [88]. DNMTis, such as azacitidine and decitabine, incorporate into DNA during replication and inhibit CpG dinucleotide methylation, leading to reactivation of hypermethylated genes [88]. HDACis, including vorinostat and panobinostat, block Zn²⁺-dependent HDAC enzymes, promoting histone acetylation and chromatin relaxation [88]. Additionally, inhibitors targeting EZH2, the catalytic subunit of PRC2 responsible for H3K27 methylation, have shown promise in preclinical models of breast cancer, particularly in combination with other agents [92].
The therapeutic potential of epidrugs extends beyond direct effects on cancer cells to modulation of the TME. Preclinical studies have demonstrated that epigenetic therapies can enhance antitumor immune responses by increasing tumor immunogenicity and reversing immunosuppressive pathways in the TME [87]. DNMTis and HDACis can upregulate the expression of cancer testis antigens and MHC class I molecules on tumor cells, making them more visible to immune recognition [89]. Simultaneously, these agents can alter the differentiation and function of immune cells within the TME, potentially shifting the balance from immunosuppressive to immunostimulatory states.
Combination Strategies and Clinical Outlook
The future of targeting the TME-epigenetics axis in stage IV breast cancer lies in rational combination therapies that simultaneously address multiple facets of apoptosis evasion. Based on current research, several promising strategies have emerged:
Epidrugs with Immune Checkpoint Inhibitors represent a particularly promising approach for overcoming immunotherapy resistance in breast cancer. Preclinical evidence suggests that epigenetic therapies can sensitize immunologically "cold" tumors to checkpoint blockade by enhancing T cell infiltration and function [87] [89]. Clinical trials are currently evaluating combinations of DNMTis or HDACis with PD-1/PD-L1 inhibitors in advanced breast cancer, with preliminary results showing enhanced efficacy compared to single-agent immunotherapy [89].
Epidrugs with Targeted Therapies offer another rational combination strategy, particularly for hormone receptor-positive breast cancers that have developed endocrine resistance. The combination of HDACis with endocrine therapies has already demonstrated clinical benefit in advanced ER+ breast cancer, leading to FDA approval of combinations such as exemestane with entinostat in some regions [92]. Ongoing research is exploring next-generation epigenetic drugs with improved therapeutic indices and selectivity for specific epigenetic regulators.
Multi-Epidrug Combinations that simultaneously target different epigenetic mechanisms may provide enhanced efficacy through synergistic effects on gene expression programs. For example, simultaneous inhibition of DNMT and HDAC activities may more effectively reactivate silenced tumor suppressor genes than either approach alone [87] [88]. However, such combinations require careful optimization to minimize overlapping toxicities while maximizing therapeutic benefit.
The clinical translation of these strategies faces several challenges, including the development of predictive biomarkers to identify patients most likely to benefit from epigenetic therapies. Potential biomarkers include specific DNA methylation signatures, histone modification patterns, or expression levels of epigenetic regulators in tumor samples [87] [92]. Additionally, non-invasive monitoring approaches using liquid biopsies to track circulating tumor DNA methylation patterns may enable dynamic assessment of treatment response and resistance development [85] [91].
The Scientist's Toolkit: Essential Research Reagents
Investigating the interplay between the TME and epigenetic regulation in apoptosis evasion requires a specialized set of research tools and reagents. The following table summarizes key resources that enable experimental dissection of these complex mechanisms.
Table 4: Essential Research Reagents for Investigating TME-Epigenetics Crosstalk in Breast Cancer
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| DNMT Inhibitors | 5-Azacytidine, Decitabine | DNA demethylation studies; combination therapy screening | Inhibit DNA methyltransferases; reactivate silenced genes [87] [88] |
| HDAC Inhibitors | Vorinostat, Panobinostat, Entinostat | Chromatin remodeling studies; histone acetylation analysis | Block histone deacetylases; promote gene expression [87] [88] |
| EZH2 Inhibitors | GSK126, Tazemetostat | H3K27me3 modulation studies; stem cell pathway analysis | Inhibit histone methyltransferase activity of PRC2 [92] |
| Cytokine/Chemokine Reagents | Recombinant TGF-β, IL-6, IL-10; neutralizing antibodies | TME signaling studies; immune cell recruitment assays | Modulate TME composition and signaling pathways [13] [86] |
| Epigenetic Antibodies | Anti-H3K27ac, Anti-H3K27me3, Anti-5mC | ChIP assays; immunohistochemistry; Western blotting | Detect specific epigenetic marks; assess chromatin states [85] [92] |
Additional specialized reagents include epigenetic editing systems such as CRISPR-dCas9 fused to catalytic domains of epigenetic modifiers, which enable locus-specific manipulation of epigenetic marks [87]. Metabolic inhibitors targeting key pathways such as glutamine metabolism or mitochondrial function can dissect the interplay between metabolism and epigenetics in the TME [89]. Furthermore, patient-derived organoid culture systems that maintain both cancer cells and native TME components provide physiologically relevant models for studying these interactions and screening potential therapeutic agents [13].
Visualizing Key Signaling Pathways
The following diagrams illustrate critical signaling pathways connecting TME signals, epigenetic regulation, and apoptosis evasion in stage IV breast cancer, generated using Graphviz DOT language.
TME-Epigenetic Signaling Network: This diagram illustrates how signals from the tumor microenvironment (yellow nodes), including hypoxia, cytokine signaling, CAF-derived signals, and metabolic stress, activate specific epigenetic regulators (red nodes) that ultimately lead to apoptosis evasion (green nodes) through multiple molecular pathways.
Epidrug Mechanisms and Combinations: This visualization depicts the major classes of epidrugs (blue nodes) that target specific epigenetic regulators (red nodes), their rational combinations with other therapeutic modalities (green nodes), and the resulting biological outcomes (yellow nodes) that collectively contribute to improved control of advanced breast cancer.
The evasion of apoptosis in stage IV breast cancer represents a complex biochemical process orchestrated through the dynamic interplay between the tumor microenvironment and epigenetic regulatory mechanisms. The TME creates a protective niche that shields cancer cells from apoptotic signals through cellular interactions, soluble factors, and metabolic adaptations. Concurrently, epigenetic modifications, including DNA methylation, histone modifications, and non-coding RNA expression, reprogram gene expression networks to enhance survival and therapeutic resistance. Understanding this multidimensional regulation provides critical insights for developing novel therapeutic strategies that simultaneously target the TME and epigenetic landscape to restore apoptotic sensitivity in treatment-resistant disease.
Future research directions should focus on deciphering the spatial and temporal dynamics of TME-epigenetics crosstalk throughout disease progression and therapeutic intervention. Advanced technologies such as single-cell multi-omics, spatial transcriptomics, and epigenetic profiling of circulating tumor cells will enable more comprehensive mapping of these interactions in clinical samples. Additionally, the development of more selective epidrugs with improved therapeutic indices and the identification of robust biomarkers for patient stratification will be essential for successful clinical translation. By integrating these approaches, researchers can develop more effective strategies to overcome apoptosis evasion and improve outcomes for patients with stage IV breast cancer.
In the context of stage IV breast cancer, the dysregulation of apoptotic pathways represents a fundamental biochemical process contributing to therapeutic resistance and disease progression. Breast cancer, comprising 18% of all cancers in women, demonstrates that tumour growth results not only from uncontrolled proliferation but equally from reduced apoptosis [21]. Despite decreased mortality rates owing to improved adjuvant therapies, advanced disease often develops resistance through defects in the cellular machinery that execute programmed cell death [21] [93]. The balance between pro-apoptotic and anti-apoptotic signals becomes disrupted in malignancy, with stage IV breast cancers frequently exhibiting overexpression of anti-apoptotic proteins, mutational inactivation of key death pathways, and metabolic adaptations that favor survival [93]. Understanding and therapeutically targeting these resistance mechanisms through rational combination strategies is paramount for improving outcomes in treatment-refractory disease.
Core Molecular Mechanisms of Apoptotic Resistance
Key Pathways and Resistance Nodes in Breast Cancer
The apoptotic machinery operates primarily through two initiation pathways: the extrinsic (death receptor) pathway and the intrinsic (mitochondrial) pathway. In breast cancer, both pathways are frequently impaired, creating significant barriers to effective treatment [93].
The extrinsic pathway initiates when death ligands like TNF-related apoptosis-inducing ligand (TRAIL) bind to death receptors DR4 and DR5, forming the death-inducing signaling complex (DISC) and activating caspase-8 [94]. The intrinsic pathway triggers through intracellular stress signals that cause mitochondrial outer membrane permeabilization, cytochrome c release, and caspase-9 activation [93]. Both pathways converge on executioner caspases (3, 6, and 7) that mediate the terminal phase of cell death [93].
Resistance mechanisms in stage IV breast cancer often involve:
- Downregulation of death receptors: Reduced surface expression of DR4 and DR5 limits initiation of extrinsic apoptosis [94].
- Overexpression of inhibitor proteins: Cellular FLICE-inhibitory protein (c-FLIP) competes with caspase-8 for binding to DISC, while Bcl-2 family anti-apoptotic proteins (Bcl-2, Bcl-xL, Mcl-1) block mitochondrial permeabilization [21] [94] [95].
- Impaired caspase function: Mutations or epigenetic silencing of caspase genes diminishes execution capability [93].
- Elevated IAP proteins: Inhibitor of apoptosis proteins (IAPs) directly bind and inhibit caspases 3, 7, and 9 [94].
Table 1: Key Apoptotic Regulatory Proteins and Their Roles in Breast Cancer Resistance
| Protein | Function | Expression in Resistant Breast Cancer | Therapeutic Implications |
|---|---|---|---|
| Bcl-2 | Anti-apoptotic; inhibits mitochondrial pore formation | Often elevated; correlated with hormone receptor positivity | Surprisingly associated with improved survival in some breast cancers; potential therapeutic target [21] |
| c-FLIP | Inhibits caspase-8 activation at DISC | Frequently overexpressed | Primary resistance mechanism to TRAIL-based therapies; key combinatorial target [94] [95] |
| Mcl-1 | Anti-apoptotic Bcl-2 family member | Commonly amplified in resistant disease | Regulates mitochondrial priming; CDK9 inhibition accelerates its degradation [95] |
| p53 | Tumor suppressor; promotes cell cycle arrest and apoptosis | Mutated in ~30% of breast cancers; dysfunctional in many others | Loss permits survival despite genomic damage; limits chemotherapy efficacy [21] [93] |
| IAP Family | Direct caspase inhibition | Elevated in treatment-resistant subsets | Smac/DIABLO mimetics can counteract this resistance mechanism [94] |
Biochemical Dynamics of Resistance Development
The transition to treatment-resistant stage IV breast cancer involves dynamic adaptations in apoptotic signaling networks. Studies examining breast tumors before and after neoadjuvant chemotherapy reveal that residual, chemoresistant cells consistently demonstrate upregulation of anti-apoptotic proteins like Bcl-2 and fundamental alterations in the balance between proliferation and apoptosis [21]. High-throughput analyses of resistant cell populations show consistent downregulation of pro-apoptotic BH3-only proteins, enhanced survival signaling through PI3K/Akt and NF-κB pathways, and metabolic rewiring that buffers against oxidative and proteotoxic stress [21] [94]. These adaptations create a permissive environment for the accumulation of additional mutations and epigenetic alterations that further reinforce the apoptosis-resistant phenotype.
Strategic Combination Therapies to Overcome Resistance
TRAIL-Based Combination Strategies
TNF-related apoptosis-inducing ligand (TRAIL) represents a promising therapeutic agent due to its ability to selectively induce apoptosis in transformed cells while sparing normal tissues [94]. However, most breast cancers exhibit primary resistance to TRAIL monotherapy, necessitating rational combination approaches.
TRAIL with CDK9 Inhibitors: Co-treatment with CDK9 inhibitors (e.g., dinaciclib, NVP-2) represents one of the most potent strategies for overcoming TRAIL resistance [95]. Mechanistically, CDK9 inhibition rapidly downregulates the short-lived anti-apoptotic proteins c-FLIP and Mcl-1, simultaneously lowering the threshold for both extrinsic and intrinsic apoptosis activation. This combination has demonstrated efficacy across diverse cancer types, including breast cancer models, with remarkable potency in eliminating clonogenic growth while sparing normal primary hepatocytes [95].
TRAIL with Proteasome Inhibitors: Combinations with proteasome inhibitors (e.g., bortezomib) enhance TRAIL sensitivity through multiple mechanisms, including endoplasmic reticulum (ER) stress induction, DR5 upregulation via CHOP activation, and reduced c-FLIP stability [94]. ER stress triggers ROS generation, which activates p38/ERK MAPK pathways and JNK signaling, collectively shifting the balance toward apoptosis execution.
TRAIL with IAP Antagonists: Smac mimetics and other IAP antagonists promote caspase activation by neutralizing XIAP, c-IAP1, and c-IAP2, thereby sensitizing resistant breast cancer cells to TRAIL-mediated killing [94] [95]. This approach particularly benefits tumors with elevated IAP expression profiles.
Table 2: Efficacy Metrics of Promising Combination Therapies in Preclinical Models
| Combination Strategy | Model System | Cell Death Induction | Proposed Mechanism | Clonogenic Survival Impact |
|---|---|---|---|---|
| TRAIL + CDK9 inhibitor | Patient-derived PDAC cells, NSCLC, breast cancer lines | 60-95% apoptosis at 24h | c-FLIP and Mcl-1 downregulation, enhanced mitochondrial priming | Near-complete abolition (<5% survival) [95] |
| TRAIL + Proteasome inhibitor | Various carcinoma models | 40-80% synergy | ER stress, DR5 upregulation, ROS-mediated signaling | Significant reduction (10-20% survival) [94] |
| TRAIL + IAP antagonist | Hematologic and solid tumor models | 50-70% enhancement | Caspase disinhibition, NF-κB modulation | Moderate reduction (15-30% survival) [94] [95] |
| HIV protease inhibitors + Chemotherapy | KBV20C resistant oral squamous carcinoma | 45-65% late apoptosis | P-gp independent sensitization, G2 phase arrest | Not reported [96] |
Non-TRAIL Combination Approaches
Beyond TRAIL-based strategies, several other rational combinations show promise for re-sensitizing resistant breast cancer cells:
Bcl-2 Family Targeting: Navitoclax (ABT-263) and related BH3 mimetics directly inhibit anti-apoptotic Bcl-2 family members, promoting mitochondrial outer membrane permeabilization and intrinsic apoptosis initiation [93]. When combined with conventional chemotherapy or targeted agents, these compounds can overcome resistance rooted in impaired mitochondrial priming.
Repurposed Antiretroviral Agents: HIV protease inhibitors including nelfinavir and lopinavir demonstrate potent chemosensitization properties in drug-resistant cancer models [96]. Notably, nelfinavir exerts this effect independently of P-glycoprotein inhibition, suggesting distinct mechanisms such as ER stress induction and Akt pathway modulation that may be particularly valuable for multidrug-resistant breast cancers.
Experimental Methodology for Combination Therapy Evaluation
Core Assessment Techniques
Rigorous evaluation of combination therapies requires multimodal assessment of apoptotic response and resistance reversal:
Dynamic BH3 Profiling: This functional technique measures mitochondrial priming by exposing permeabilized cells to BH3 domain peptides and quantifying cytochrome c release [95]. The increase in priming following drug exposure serves as a predictive biomarker for apoptosis sensitivity, with TRAIL-CDK9i combinations demonstrating particularly robust enhancements in mitochondrial priming across diverse cancer types.
Annexin V/Propidium Iodide Staining: Flow cytometric analysis of phosphatidylserine externalization (annexin V positivity) with membrane integrity assessment (PI exclusion) provides quantitative apoptosis measurements at the population level [97]. This method distinguishes early apoptotic (annexin V+/PI-), late apoptotic (annexin V+/PI+), and necrotic (annexin V-/PI+) populations, enabling kinetic analyses of cell death progression.
Caspase Activity Assays: Fluorometric or colorimetric substrates specific for initiator (caspase-8, -9) and executioner (caspase-3/7) caspases provide enzymatic activity measurements [97]. Western blot analysis of caspase cleavage and PARP proteolysis offers complementary confirmation of apoptotic pathway activation.
TUNEL Assay: Terminal deoxynucleotidyl transferase dUTP nick end labeling detects DNA fragmentation, a hallmark of late-stage apoptosis [21] [97]. While highly sensitive, this technique requires careful controls to distinguish apoptotic DNA cleavage from necrotic degradation.
Morphological Assessment: High-content imaging analysis of characteristic apoptotic morphology—including membrane blebbing, cell shrinkage, and nuclear condensation—provides orthogonal validation of cell death mechanisms [93] [97]. This approach can be combined with specific molecular markers for mechanistic insights.
Advanced Mechanistic Studies
For in-depth investigation of resistance reversal mechanisms:
Death Inducing Signaling Complex (DISC) Analysis: Immunoprecipitation of activated death receptors followed by Western blotting for FADD, caspase-8, and c-FLIP reveals compositional changes in the primary signaling complex following combination treatment [94] [95].
Mitochondrial Function Assays: Multiparameter assessment of mitochondrial membrane potential (ΔΨm), ROS production, and cytochrome c localization elucidates contributions of the intrinsic pathway to combination therapy efficacy [93] [97].
3D Culture and Organoid Models: Patient-derived organoids and spheroid cultures maintain physiological tissue architecture and tumor microenvironment interactions, providing more clinically relevant therapeutic response data [95]. Notably, pancreatic cancer organoids resistant to gemcitabine demonstrated exceptional sensitivity to TRAIL-CDK9i combinations, highlighting the potential of this approach for treatment-resistant disease.
Research Reagent Solutions
Table 3: Essential Research Tools for Apoptosis Combination Therapy Studies
| Reagent/Category | Specific Examples | Primary Application | Key Considerations |
|---|---|---|---|
| Recombinant Death Ligands | rhTRAIL, Agonistic anti-DR4/DR5 antibodies | Extrinsic pathway activation | Specific activity varies between preparations; receptor specificity should be verified [94] [95] |
| Small Molecule Inhibitors | Dinaciclib (CDK9i), NVP-2 (CDK9i), Navitoclax (Bcl-2 family inhibitor) | Target-specific sensitization | Off-target effects necessitate careful controls; pharmacokinetics impact dosing schedules [95] |
| Apoptosis Detection Reagents | Annexin V conjugates, Caspase substrates/antibodies, TUNEL assay kits | Quantitative cell death measurement | Timing critical for accurate staging; multiplex approaches recommended for mechanism [97] |
| Viability/Proliferation Assays | ATP-based viability, Clonogenic survival, Real-time cell analysis | Therapeutic efficacy assessment | Distinguish cytostatic vs. cytotoxic effects; clonogenic assays most relevant for long-term impact [95] |
| Mitochondrial Function Probes | TMRE/JC-1 (ΔΨm), MitoSOX (ROS), Cytochrome c antibodies | Intrinsic pathway evaluation | Functional assays require careful standardization and controls [97] |
| 3D Culture Systems | Basement membrane extract matrices, Patient-derived organoids | Physiological relevance modeling | Technical complexity balanced by improved clinical predictivity [95] |
Signaling Pathway Diagrams
The strategic optimization of combination therapies to re-sensitize resistant breast cancer cells represents a paradigm shift in oncology, moving beyond conventional dose escalation toward mechanistically informed targeting of apoptotic pathways. The TRAIL-CDK9 inhibitor combination exemplifies this approach, demonstrating exceptional potency across diverse cancer models including treatment-resistant malignancies [95]. Future developments will likely focus on biomarker-driven patient selection, sequential therapy scheduling to prevent adaptive resistance, and triple-combination strategies that simultaneously target multiple resistance nodes. For stage IV breast cancer patients facing limited options, these rationally designed apoptotic re-sensitization strategies offer renewed therapeutic potential grounded in the fundamental biochemistry of cell death regulation.
Leveraging Apoptosis-Related Biomarkers (e.g., AIF1, Caspase-3) for Prognostic Stratification
The deregulation of apoptotic, or programmed cell death, pathways is a established hallmark of cancer, enabling uncontrolled cell proliferation and tumor survival [98] [99]. In the context of stage IV breast cancer, where therapeutic options are often limited and prognosis poor, a deep understanding of the biochemical processes of apoptosis provides a critical framework for identifying novel prognostic and therapeutic strategies. Apoptosis proceeds via two principal pathways that converge on a common execution phase. The extrinsic pathway is initiated by the binding of extracellular death ligands (e.g., FasL, TRAIL) to cell surface death receptors, leading to the assembly of the Death-Inducing Signaling Complex (DISC) and activation of initiator caspase-8 [98] [99]. The intrinsic pathway, activated by cellular stress signals such as DNA damage, is regulated by the Bcl-2 family of proteins and results in mitochondrial outer membrane permeabilization (MOMP). This pivotal event causes the release of apoptogenic factors, including cytochrome c and Apoptosis-Inducing Factor 1 (AIF1), from the mitochondrial intermembrane space into the cytosol [100] [98]. Released cytochrome c facilitates the formation of the apoptosome, activating caspase-9, which then cleaves and activates the executioner caspase, caspase-3 [99]. AIF1, in contrast, translocates to the nucleus and induces large-scale DNA fragmentation in a caspase-independent manner [100]. The core components of these pathways, particularly executioner factors like caspase-3 and AIF1, have emerged as promising biomarkers for stratifying patient prognosis and predicting response to therapy.
Prognostic Value of Key Apoptosis Biomarkers in Breast Cancer
Clinical evidence robustly demonstrates that the expression levels of specific apoptosis-related biomarkers are strongly correlated with survival outcomes in breast cancer patients. The relationship, however, is complex and can be counter-intuitive, as illustrated by caspase-3.
Table 1: Prognostic Value of Caspase-3 in Breast Cancer
| Study Cohort / Subtype | Expression Level | Correlation with Survival | Hazard Ratio (HR) and Statistical Data |
|---|---|---|---|
| Early-Stage Invasive Breast Cancer (n=1902) [101] [102] | High | Adverse Breast Cancer-Specific Survival | HR: 1.347; 95% CI: 1.086-1.670; P = 0.007 (Multivariate) |
| Meta-Analysis (n=3091, 21 studies) [103] | High | Poor Overall Survival | HR: 1.73; 95% CI: 1.12–2.67; P = 0.014 (Pooled Analysis) |
| Triple-Negative Breast Cancer (TNBC) [100] | High | Improved Overall Survival | Significant OS advantage, particularly in chemotherapy-treated patients. |
| Asian Patient Subgroup (Meta-Analysis) [103] | High | Poor Overall Survival | HR: 3.16; 95% CI: 1.20–8.15; P = 0.020 |
The expression of caspase-3, a primary executioner caspase, is independently associated with adverse breast cancer-specific survival in large cohort studies [101] [102]. A comprehensive meta-analysis of over 3,000 cases confirmed that high caspase-3 expression is a significant risk factor for poor overall survival, with this effect being particularly pronounced in Asian populations and in specific breast cancer subtypes like progestogen receptor (PR) and HER-2 positive cancers [103]. Paradoxically, in the aggressive triple-negative breast cancer (TNBC) subtype, elevated levels of the cleaved, active form of caspase-3 are associated with an overall survival advantage, especially in patients who receive chemotherapy [100]. This suggests that the functional integrity of the caspase-dependent apoptotic pathway in TNBC may be a critical determinant for responding to cytotoxic treatment.
Alongside caspase-3, the caspase-independent effector AIF1 has also demonstrated significant prognostic potential. In TNBC, high levels of AIF1 protein, which is typically localized in the cytoplasm in a mitochondrial pattern, grant a significant overall survival advantage [100]. This survival benefit is markedly stronger in patients who undergo chemotherapy, indicating that AIF1-mediated cell death may be a key mechanism through which chemotherapy exerts its cytotoxic effect. The KM Plotter for breast proteins database corroborates these findings, showing a massive survival benefit for patients with high AIF1 protein expression across multiple survival estimates [100].
Table 2: Prognostic Value of AIF1 and Combinatorial Biomarkers in Breast Cancer
| Biomarker / Combination | Cancer Context | Prognostic Value | Key Findings |
|---|---|---|---|
| AIF1 (Protein) | Triple-Negative Breast Cancer (TNBC) [100] | Improved Overall Survival | Logrank p=0.0033; HR=0.40. Stronger effect in chemotherapy-treated patients (p=0.0072). |
| AIF1 (mRNA - AIFM1) | Triple-Negative Breast Cancer (TNBC) [100] | Improved Overall Survival | Logrank p=0.018; HR=0.48 (0.26–0.9). |
| High Caspase-3 / High Calpain-1 | Total Breast Cancer Cohort [101] | Worse Breast Cancer-Specific Survival | P = 0.005 (Kaplan-Meier analysis) |
| High Caspase-3 / High Calpain-1 | Basal-like Breast Cancer Subgroup [101] | Worse Breast Cancer-Specific Survival | P = 0.034 (Kaplan-Meier analysis) |
Furthermore, the prognostic power of these biomarkers can be enhanced by evaluating them in combination. For instance, the co-expression of high caspase-3 and high calpain-1 (a calcium-dependent protease implicated in cancer) predicts worse breast cancer-specific survival in the overall patient population and, more specifically, within the basal-like subgroup [101]. This highlights the importance of understanding the complex interactions within the apoptotic machinery and related proteolytic systems.
Experimental Protocols for Biomarker Analysis
To reliably generate the prognostic data discussed above, standardized and validated experimental protocols are essential. Immunohistochemistry (IHC) on formalin-fixed, paraffin-embedded (FFPE) tissue sections is the cornerstone technique for visualizing and quantifying protein expression of apoptosis biomarkers in the tumor tissue context.
Immunohistochemistry (IHC) for Protein Detection
Materials and Reagents:
- FFPE Tissue Microarrays (TMAs) or Whole Sections: Containing representative tumor samples.
- Primary Antibodies: Mouse anti-human caspase-3 (for procaspase-3), rabbit anti-human cleaved caspase-3/p20 (active form), rabbit anti-human AIF1 [100] [104].
- Biotin-Conjugated Secondary Antibodies: Species-specific (e.g., anti-mouse, anti-rabbit).
- Avidin-Biotin-Peroxidase Complex (ABC Kit): For signal amplification.
- Enzyme Substrate: e.g., 3,3'-Diaminobenzidine (DAB), which produces a brown precipitate upon reaction with horseradish peroxidase (HRP).
- Hematoxylin: For counterstaining cell nuclei.
Detailed Protocol:
- Sectioning and Deparaffinization: Cut FFPE blocks into 4-5 µm thick sections. Deparaffinize in xylene and rehydrate through a graded series of ethanol to water.
- Antigen Retrieval: Perform heat-induced epitope retrieval by incubating slides in a citrate-based or EDTA-based buffer (pH 6.0 or 9.0) using a pressure cooker or microwave to unmask hidden epitopes.
- Blocking: Incubate sections with a protein block (e.g., normal serum) to reduce non-specific binding.
- Primary Antibody Incubation: Apply the optimized dilution of the primary antibody (e.g., cleaved caspase-3 at 1:100 [104]) and incubate overnight at 4°C in a humidified chamber.
- Secondary Antibody and ABC Incubation: Apply the appropriate biotinylated secondary antibody, followed by the pre-formed ABC complex as per the manufacturer's instructions.
- Detection: Develop the slides with DAB substrate solution for a predetermined time, then stop the reaction in water.
- Counterstaining and Mounting: Counterstain with hematoxylin to visualize nuclei, then dehydrate, clear, and mount the slides with a permanent mounting medium.
Scoring and Quantification
Assessment is typically performed by two independent pathologists blinded to the clinical outcome [104]. Staining is evaluated in cancerous epithelium across multiple randomly selected fields.
- Caspase-3 and AIF1 Scoring: Cytoplasmic immunoreactivity is scored. Patients can be stratified as "positive" or "negative" using a predefined threshold (e.g., >5% of tumor cells showing distinct staining) [104]. For more granular analysis, a semiquantitative H-score or immunoreactive score (IRS) that incorporates both staining intensity (0-3) and the percentage of positive cells (0-100%) can be calculated.
- Quality Control: Specificity controls must include tissue incubation with pre-immune serum or isotype-matched immunoglobulins as negative controls. Validation of antibody specificity via Western blotting on a subset of frozen samples is highly recommended [104].
Signaling Pathways and Molecular Interactions
The following diagram illustrates the core apoptotic pathways and the points at which the key biomarkers AIF1 and caspase-3 function.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their applications for studying apoptosis biomarkers in a research setting.
Table 3: Research Reagent Solutions for Apoptosis Biomarker Analysis
| Reagent / Resource | Specific Example | Function and Application in Research |
|---|---|---|
| Primary Antibodies for IHC | Anti-Cleaved Caspase-3 (p20) | Detects the active, cleaved form of caspase-3, providing a direct readout of apoptotic executioner activity in FFPE tissues [104]. |
| Anti-AIF1 | Detects apoptosis-inducing factor 1, used to assess the status of the caspase-independent apoptotic pathway via cytoplasmic/mitochondrial localization [100]. | |
| IHC Detection Kits | Avidin-Biotin-Peroxidase Complex (ABC) | Signal amplification system used in conjunction with biotinylated secondary antibodies to enhance detection sensitivity of target proteins [104]. |
| Clinical Databases | KM Plotter | Online tool (https://kmplot.com/) used for in silico validation of biomarker prognostic potential by analyzing mRNA expression and survival data from large patient cohorts (e.g., TNBC) [100]. |
| Cell Line Models | MCF-7 Caspase-3 Restored | Caspase-3 deficient MCF-7 breast cancer cells with restored caspase-3 expression; used in vitro to study the specific role of caspase-3 in chemosensitivity and apoptotic signaling [102]. |
The stratification of breast cancer patients, particularly those with advanced disease, using apoptosis-related biomarkers like caspase-3 and AIF1 represents a promising avenue for personalizing prognosis and refining therapeutic strategy. The evidence confirms that these biomarkers provide crucial, and often independent, prognostic information. The paradoxical role of caspase-3—where its high expression is generally linked to poor survival but predicts better outcomes in chemotherapy-treated TNBC—underscores the complexity of apoptosis in cancer and highlights the necessity of context-dependent interpretation. Future research should focus on validating these biomarkers in large, multi-center prospective trials and standardizing IHC scoring protocols to facilitate their transition into routine clinical practice. Furthermore, exploring the interplay between caspase-dependent and independent pathways, and their relationship with the tumor immune microenvironment, could unlock novel combination therapies designed to re-sensitize treatment-resistant, stage IV breast cancers to cell death.
Validation and Comparative Analysis of Apoptosis-Targeting Therapies in Advanced Disease
Comparative Efficacy of Single-Agent vs. Combination Apoptosis Inducers in Preclinical Models
The emergence of resistance to apoptotic cell death constitutes a fundamental hallmark of cancer pathogenesis, presenting a significant barrier to successful therapeutic outcomes in stage IV breast cancer. This whitepaper synthesizes current preclinical evidence evaluating the efficacy of apoptosis-inducing agents, contrasting single-agent approaches with rational combination strategies. Through systematic analysis of quantitative data from diverse experimental models, we demonstrate that combinatorial regimens consistently outperform monotherapies across multiple breast cancer subtypes, particularly in treatment-resistant settings. The findings provide a mechanistic framework for understanding synergistic interactions among apoptosis-targeting agents and establish methodological guidelines for preclinical assessment of novel therapeutic combinations. These insights offer researchers and drug development professionals a validated roadmap for advancing more effective, apoptosis-focused treatment paradigms against advanced breast cancer.
Apoptosis evasion represents a critical oncogenic mechanism that enables breast cancer progression and therapeutic resistance [105] [106]. The molecular machinery of apoptosis operates through two primary signaling cascades: the extrinsic (death receptor-mediated) pathway and the intrinsic (mitochondrial-mediated) pathway [105]. In stage IV breast cancer, both pathways are frequently compromised through overexpression of anti-apoptotic proteins (e.g., BCL-2, MCL-1) and downregulation or mutation of pro-apoptotic factors [105] [106]. This molecular rewiring not only drives disease progression but also limits the effectiveness of conventional chemotherapeutics, which predominantly rely on apoptosis induction for their cytotoxic effects [105].
Therapeutically targeting apoptotic pathways has emerged as a promising strategy for overcoming treatment resistance in advanced breast cancer. However, the development of effective apoptosis-targeting agents faces substantial challenges, including pathway redundancy, compensatory mechanisms, and robust survival signaling within tumor cells [105]. This complexity necessitates a thorough comparative assessment of therapeutic approaches to identify optimal strategies for engaging the apoptotic machinery in treatment-refractory disease.
Apoptosis Signaling Pathways: Molecular Framework
Core Apoptotic Machinery
The extrinsic apoptosis pathway initiates when extracellular death ligands (e.g., TRAIL, FAS ligand) bind to cognate death receptors (DR4, DR5, FASR), triggering caspase-8/10 activation and subsequent execution via caspases-3/7 [105]. This pathway offers therapeutic appeal, particularly through TRAIL signaling, which can induce apoptosis regardless of p53 status—a significant advantage in p53-mutated breast cancers [105].
The intrinsic pathway activates in response to intracellular stress signals, leading to BAX/BAK-mediated mitochondrial outer membrane permeabilization (MOMP), cytochrome c release, and apoptosome formation [105]. This pathway is critically regulated by the balance between pro-apoptotic (BIM, BID, BAX, BAK) and anti-apoptotic (BCL-2, MCL-1, BCL-XL) BCL-2 family proteins [105] [107].
Beyond these core pathways, emerging evidence indicates significant cross-talk with other regulatory networks, including mTOR signaling [107], HSP90-mediated protein stability [108], and GSK-3β activity [109], which collectively influence apoptotic susceptibility in breast cancer cells.
Figure 1: Apoptosis Signaling Pathways in Breast Cancer. The diagram illustrates the core extrinsic (death receptor) and intrinsic (mitochondrial) apoptosis pathways, highlighting key regulatory nodes and points of cross-talk with resistance mechanisms. Anti-apoptotic proteins (red) represent critical therapeutic targets, while cross-talk pathways (green) offer opportunities for combination approaches.
Quantitative Comparison of Single-Agent vs. Combination Approaches
Efficacy Metrics Across Preclinical Models
Table 1: Comparative Efficacy of Apoptosis-Targeting Agents in Preclinical Breast Cancer Models
| Therapeutic Agent/Combination | Molecular Target | Experimental Model | Efficacy Metric | Single-Agent Response | Combination Response | Synergy Assessment |
|---|---|---|---|---|---|---|
| LCTA-3344 + AKT Inhibitor IV [108] | Apoptosis inducer + AKT | MCF-7/HT hormone-resistant BC | Combination Index (CI) | IC~50~: 2.6 ± 0.3 µM (MCF-7)1.4 ± 0.1 µM (MCF-7/HT) | CI: 0.8 (MCF-7)CI: 0.4 (MCF-7/HT) | Synergistic (CI<1) |
| 9-ING-41 + Venetoclax [109] | GSK-3β + BCL-2 | Double-hit lymphoma (DHL) | Cell viability & apoptosis | Moderate single-agent activity | Marked synergistic cytotoxicity | Superior to either agent alone |
| MTI-31 (mTOR-KI) [107] | mTORC1/mTORC2 | HER2+/PIK3CAmut breast cancer | Tumor growth inhibition | Dose-dependent TGI | N/A (single agent) | MED: 5 mg/kg (>50% TGI) |
| ONC201 [105] | TRAIL pathway modulator | Multiple solid tumors | Clinical trial phase | Various Phase I/II trials | Combination trials ongoing | N/A |
Analysis of Combination Synergy Patterns
The quantitative data reveal consistent superiority of rational combination regimens over single-agent approaches across diverse preclinical models. The most compelling evidence emerges from studies where combination index (CI) values were quantitatively determined, with CI<1 indicating true synergistic interactions rather than merely additive effects [108]. Notably, the combination of novel apoptosis inducer LCTA-3344 with AKT Inhibitor IV demonstrated enhanced synergy specifically in the hormone-resistant MCF-7/HT subline (CI=0.4) compared to the parental MCF-7 cells (CI=0.8), suggesting particular utility in treatment-resistant settings [108].
Similar synergistic relationships were observed in hematologic malignancy models, where the GSK-3β inhibitor 9-ING-41 combined with the BCL-2 inhibitor venetoclax produced "marked synergistic cytotoxicity" in double-hit lymphoma cells, exceeding the efficacy of either agent alone [109]. This combination enhanced cell cycle arrest and modulated key proteins in the GSK-3 pathway and downstream WNT/β-catenin signaling [109].
Experimental Protocols for Apoptosis Induction Studies
Standardized Apoptosis Induction Methodology
Protocol 1: Chemical Induction of Apoptosis in Breast Cancer Cell Lines [110]
Cell Preparation:
- Inoculate adherent cells into 10 cm² tissue culture dishes or suspension cells into T75 flasks at ~1 × 10⁶ cells/mL density.
- Maintain cells in appropriate medium (e.g., RPMI-1640 with 10% FBS for Jurkat cells) at 37°C in a 5% CO₂ humidified incubator.
Agent Administration:
- Prepare stock solutions of apoptosis-inducing agents in suitable solvents (DMSO for staurosporine, actinomycin D, camptothecin; H₂O for doxorubicin).
- Add cellular-damaging agents at optimized concentrations:
- Doxorubicin: 0.2 µg/mL
- Actinomycin D: 1 µM
- Camptothecin: 1-10 µM
- Staurosporine: 2-10 µM
- Venetoclax: 50-100 nM [109]
- Include negative controls with equivalent volumes of buffer or solvent alone.
Incubation and Monitoring:
- Harvest cells at multiple time points (8, 12, 16, 24, 48, and 72 hours) post-treatment to capture dynamic apoptotic responses.
- For combination studies, administer agents simultaneously or sequentially based on mechanistic rationale.
Apoptosis Detection:
- Collect cells by centrifugation at 300-350 × g for 5 minutes.
- Wash with PBS and resuspend to 1.5 × 10⁶ cells/mL for downstream analysis.
- Assess apoptosis via multiple complementary methods:
- Annexin V/propidium iodide staining by flow cytometry
- Caspase-3/7 activation assays
- Western blotting for PARP cleavage, caspase activation
- Mitochondrial membrane potential measurements (JC-1 assay)
Protocol 2: Preclinical Evaluation of Combination Therapies [108] [111]
High-Throughput Drug Screening Platform:
- Establish short-term patient-derived xenograft cultures (PDXC) plated as tumor-spheres.
- Treat with individual drugs and combinations at concentrations scaled to clinical C~max~ values.
- Utilize fixed-ratio combinations (e.g., C~max~ and 10% C~max~) to control for false positives.
Synergy Assessment:
- Generate concentration-response curves for individual agents and combinations.
- Calculate combination index (CI) using the Chou-Talalay method:
- CI < 1 indicates synergy
- CI = 1 indicates additive effect
- CI > 1 indicates antagonism
- Validate synergistic combinations in multiple orthogonal assays.
In Vivo Validation:
- Implement orthotopic xenograft models representing key molecular subtypes.
- Administer agents at minimum efficacious dose (MED) and maximum tolerated dose (MTD).
- Monitor tumor volume regression and survival benefit.
Figure 2: Experimental Workflow for Apoptosis Induction Studies. The diagram outlines a comprehensive methodology for evaluating single-agent and combination apoptosis inducers, incorporating both in vitro and in vivo validation steps. Critical pathway-specific assays (green) and key analytical approaches (yellow) are highlighted.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Apoptosis Studies
| Reagent/Category | Specific Examples | Research Application | Experimental Considerations |
|---|---|---|---|
| Small Molecule Apoptosis Inducers | LCTA-3344 [108], ONC201 [105], 9-ING-41 [109] | Mechanistic studies of intrinsic/extrinsic pathway activation | Optimize concentration using IC~50~ determination; validate target engagement |
| BCL-2 Family Inhibitors | Venetoclax [109], Navitoclax [111] | Targeting anti-apoptotic proteins in mitochondrial pathway | Monitor MCL-1 upregulation as resistance mechanism; combination approaches preferred |
| Pathway-Specific Inhibitors | AKT Inhibitor IV [108], MTI-31 (mTOR-KI) [107], Cobimetinib [111] | Modulating cross-talk signaling networks | Assess baseline pathway activation; employ combination indices to quantify synergy |
| Death Receptor Agonists | Anti-FAS/CD95 antibody [110], TRAIL receptor agonists [105] | Activating extrinsic apoptosis pathway | Confirm receptor expression; evaluate decoy receptor interference |
| Apoptosis Detection Reagents | Annexin V/Propidium Iodide, Caspase substrates, JC-1 dye [110] | Quantifying apoptotic response | Use multiple complementary methods; establish temporal kinetics |
| Cell Culture Models | MCF-7/HT (hormone-resistant) [108], Patient-derived xenograft cultures [111] | Preclinical efficacy assessment | Employ both sensitive and resistant variants; validate clinical relevance |
Discussion and Future Perspectives
The accumulated preclinical evidence strongly supports combination approaches over single-agent strategies for effective apoptosis induction in advanced breast cancer models. The observed synergistic interactions between novel apoptosis inducers and targeted agents directed against complementary pathways (e.g., AKT, mTOR, GSK-3β) suggest that overcoming resistance requires simultaneous modulation of multiple nodes within the apoptotic network [108] [107] [109].
Several key principles emerge from these studies that should guide future research directions. First, the molecular context of the tumor—including hormone receptor status, HER2 amplification, PIK3CA mutation status, and prior therapy exposure—profoundly influences response to apoptosis-targeting agents [107] [108]. Second, the sequencing and scheduling of combination therapies requires careful optimization, as demonstrated by the enhanced efficacy of certain drug pairs in specific resistant subpopulations [108]. Third, comprehensive biomarker development is essential for identifying patient populations most likely to benefit from these targeted approaches [105].
Future work should prioritize the development of next-generation apoptosis inducers with improved pharmacological properties, the identification of rational combination partners based on mechanistic understanding of resistance pathways, and the validation of predictive biomarkers that can guide clinical translation. The integration of apoptosis-targeting strategies with emerging therapeutic modalities—including immunotherapy, antibody-drug conjugates, and cellular therapies—represents a particularly promising frontier in the ongoing effort to overcome treatment resistance in stage IV breast cancer [112] [113].
The dysregulation of apoptosis is a hallmark of cancer, playing a critical role in tumor progression, metastasis, and therapeutic resistance. In the context of stage IV breast cancer, the validation of prognostic biomarkers within the apoptotic pathway is paramount for stratifying patients and personalizing treatment strategies. This whitepaper provides an in-depth technical examination of the prognostic potential of Apoptosis-Inducing Factor 1 (AIF1), Caspase-3, and B-Cell Lymphoma 2 (BCL-2). We synthesize current evidence from clinical cohorts, detailing experimental methodologies for biomarker assessment, and contextualize their function within the broader biochemical process of apoptosis. The objective is to present a comprehensive guide for researchers and drug development professionals on the validation and clinical application of these key apoptotic regulators in advanced breast cancer.
Stage IV breast cancer is characterized by the dissemination of tumor cells to distant sites, a process facilitated by the evasion of programmed cell death. Apoptosis is a genetically controlled cell death mechanism essential for maintaining tissue homeostasis and eliminating damaged cells. In carcinogenesis, imbalances between pro-apoptotic and anti-apoptotic signals allow cancer cells to survive beyond their normal lifespan, contributing to tumor growth and resistance to therapy [21] [114]. The core biochemical process of apoptosis can be initiated via two principal pathways: the intrinsic (mitochondrial) pathway, regulated by the BCL-2 family of proteins, and the extrinsic (death receptor) pathway. Both pathways converge to activate executioner caspases, such as Caspase-3, which orchestrate the systematic dismantling of the cell. AIF1 represents a caspase-independent route of apoptosis, translocating from the mitochondria to the nucleus upon lethal cellular stress to trigger DNA fragmentation [115] [116]. A profound understanding of these interconnected mechanisms is crucial for developing biomarkers that can accurately predict disease behavior and therapeutic efficacy in stage IV breast cancer.
Biomarker-Specific Analysis and Clinical Evidence
BCL-2: A Dual-Function Regulator
BCL-2 is a key anti-apoptotic protein that promotes cell survival by preventing mitochondrial outer membrane permeabilization (MOMP), thereby inhibiting the release of pro-apoptotic factors like cytochrome c and AIF1.
- Function and Mechanism: BCL-2 protein contains four BCL-2 homology (BH) domains (BH1-BH4). It exerts its anti-apoptotic effect by sequestering pro-apoptotic proteins such as Bax and Bak, preventing them from forming pores in the mitochondrial membrane [114]. The BH4 domain is particularly critical for its survival function.
- Clinical and Prognostic Evidence: The prognostic significance of BCL-2 in breast cancer is complex and context-dependent. Contrary to its anti-apoptotic function, its expression in breast tumor tissue is frequently associated with favorable prognostic features, including estrogen receptor (ER) positivity and low tumor grade. Consequently, BCL-2 positivity has been correlated with improved survival in several studies [21]. However, its overexpression is implicated in chemoresistance. Research demonstrates that the calcium-sensing receptor antagonist NPS-2143 induces apoptosis in breast cancer cells, an effect accompanied by a "remarkable reduction in the expression of Bcl-2 antiapoptotic protein" [115]. Furthermore, a 2023 study found a statistically significant negative association between the expression of tumor-suppressor microRNAs (let-7d and miR-195) and BCL-2 gene expression, suggesting a regulatory mechanism that, when disrupted, promotes breast carcinogenesis [117].
Caspase-3: The Key Executioner Protease
Caspase-3 is a critical effector caspase that, upon activation, cleaves a wide array of cellular substrates, leading to the characteristic morphological changes of apoptosis.
- Function and Mechanism: Caspase-3 exists as an inactive zymogen that is cleaved and activated by initiator caspases (e.g., caspase-9 in the intrinsic pathway, caspase-8 in the extrinsic pathway). Its activation is a point of convergence in the apoptotic cascade and is often considered a point of no return [116]. One of its key substrates is cytokeratin 18 (CK18); the caspase-cleaved form of CK18 (detected by the M30 Apoptosense assay) is a specific serological biomarker of epithelial apoptosis [116].
- Clinical and Prognostic Evidence: The expression and activation of Caspase-3 are pivotal for the efficacy of many anti-cancer therapies. A 2021 study on breast cancer cells demonstrated that the pro-apoptotic effect of the CaSR antagonist NPS-2143 was mediated through the significant activation of caspase 3/7 [115]. In clinical specimens, studies using immunohistochemistry (IHC) have shown correlations between caspase-3 expression and tumor characteristics. A 2023 study confirmed a "statistically significant positive association" between the relative gene expression of CASP3 and the tumor-suppressive microRNAs let-7d and miR-195 in breast cancer tissues [117]. This positions Caspase-3 not only as a key mediator of cell death but also as a potential biomarker for monitoring therapeutic response.
AIF1: The Caspase-Independent Executioner
Apoptosis-Inducing Factor 1 (AIF1) is a flavoprotein located in the mitochondrial intermembrane space that, when released, mediates a caspase-independent pathway of apoptosis.
- Function and Mechanism: In response to severe cellular damage, AIF is cleaved and translocates from the mitochondria to the nucleus. Once in the nucleus, it induces chromatin condensation and large-scale (~50 kbp) DNA fragmentation, a process distinct from the oligonucleosomal DNA laddering produced by caspase-activated DNases [115] [116]. This pathway can serve as a backup cell death mechanism when caspase activation is blocked.
- Clinical and Prognostic Evidence: While the search results provided do not contain specific clinical cohort data validating AIF1 in breast cancer, its fundamental role in the apoptotic machinery is well-established. One study noted that stimulation of the Calcium-sensing Receptor (CaSR) could protect breast cancer cells from caspase-independent apoptosis by "hindering nuclear accumulation of apoptosis inducing factor (AIF)" [115]. This highlights the pathophysiological relevance of AIF in breast cancer cell survival and underscores its potential as a biomarker, particularly in the context of resistance to caspase-dependent therapies. Validation in clinical cohorts remains an active and necessary area of investigation.
Table 1: Summary of Apoptotic Biomarkers in Breast Cancer
| Biomarker | Primary Function | Prognostic Association | Therapeutic Implications |
|---|---|---|---|
| BCL-2 | Anti-apoptotic; inhibits MOMP | Paradoxically associated with favorable prognosis (ER+, low grade) but promotes chemoresistance [21]. | Target of inhibitors (e.g., Venetoclax); reduction sensitizes cells to therapy [115] [114]. |
| Caspase-3 | Pro-apoptotic; executioner caspase | Positive association with tumor-suppressive miRNAs; activation correlates with therapy-induced apoptosis [115] [117]. | Key mediator of treatment efficacy; cleaved CK18 (M30) is a serological PD biomarker [116]. |
| AIF1 | Pro-apoptotic; caspase-independent DNA fragmentation | Implicated in bypassing caspase-dependent resistance; hindrance of nuclear accumulation promotes survival [115]. | Potential biomarker for alternative cell death pathways and resistance mechanisms. |
Experimental Protocols for Biomarker Validation
Robust validation of apoptotic biomarkers requires a multi-faceted methodological approach. Below are detailed protocols for key techniques cited in the literature.
Immunohistochemistry (IHC) on Tissue Microarrays (TMAs)
IHC is a cornerstone for quantifying protein expression in formalin-fixed, paraffin-embedded (FFPE) clinical samples, allowing for the correlation of biomarker levels with clinicopathological data.
- Protocol Workflow:
- TMA Construction: Core biopsies from donor FFPE tissue blocks (e.g., from primary breast tumors and matched normal tissue) are assembled into a recipient TMA block [118] [117].
- Sectioning and Deparaffinization: TMA blocks are sectioned (4-5 μm thickness), mounted on slides, and deparaffinized in xylene followed by a graded alcohol series.
- Antigen Retrieval: Slides are heated in a citrate-based or EDTA-based buffer (pH 6.0 or 9.0) using a pressure cooker or microwave to unmask epitopes.
- Immunostaining: Sections are incubated with primary antibodies specific for BCL-2, activated Caspase-3, or AIF1. This is followed by incubation with a labeled secondary antibody and detection using a chromogen like 3,3'-Diaminobenzidine (DAB).
- Counterstaining and Scoring: Slides are counterstained with hematoxylin, dehydrated, and mounted. Staining is scored by a pathologist based on intensity (0-3) and percentage of positive tumor cells, often resulting in a combined H-score or a simple positive/negative classification [117].
Quantitative Real-Time PCR (qRT-PCR) for Gene Expression
qRT-PCR is used to quantify the mRNA expression levels of apoptotic genes, providing a precise measure of transcriptional regulation.
- Protocol Workflow:
- RNA Extraction: Total RNA is isolated from homogenized tissue samples or cell lines using TRIzol reagent or commercial kits, following the manufacturer's instructions [46] [117].
- cDNA Synthesis: RNA is reverse transcribed to complementary DNA (cDNA) using a commercial cDNA synthesis kit with random hexamers and/or oligo-dT primers.
- qPCR Amplification: The cDNA is combined with gene-specific forward and reverse primers (for BCL2, CASP3, AIF1, and housekeeping genes like GAPDH or U6), and a SYBR Green master mix. The reaction is run on a real-time PCR instrument.
- Data Analysis: The cycle threshold (Ct) values for target genes are normalized to the housekeeping gene, and the relative expression is calculated using the 2^–ΔΔCt method [117].
Assessment of Caspase Activity
Functional assays for caspase activity are crucial for confirming the engagement of the apoptotic pathway.
- Protocol Workflow (Apo-ONE Homogeneous Caspase-3/7 Assay):
- Cell Plating and Treatment: Breast cancer cells (e.g., MDA-MB-231, MCF-7) are plated in a black-walled, clear-bottom 96-well plate and treated with the compound of interest (e.g., NPS-2143) for a specified duration [115].
- Assay Reagent Addition: An equal volume of Apo-ONE Caspase-3/7 reagent, containing a pro-fluorescent substrate, is added to each well.
- Incubation and Measurement: The plate is incubated protected from light for a period (e.g., 2-4 hours) to allow caspase cleavage of the substrate, which generates a fluorescent product. Fluorescence is measured with a plate reader at an excitation/emission of ~499/521 nm [115].
- Data Analysis: Fluorescence in treated samples is normalized to vehicle control and expressed as a fold-change in caspase 3/7 activity.
Table 2: Key Research Reagent Solutions for Apoptosis Biomarker Studies
| Reagent / Assay | Function / Application | Example from Literature |
|---|---|---|
| TUNEL Assay | Detects DNA fragmentation in situ by labeling 3'-OH ends of DNA breaks; labels late-stage apoptotic cells [21]. | Used for quantification of apoptosis in breast cancer tissue sections. |
| Apo-ONE Homogeneous Caspase-3/7 Assay | Fluorescent-based kit to quantitatively measure the enzymatic activity of effector caspases in cell cultures [115]. | Used to demonstrate NPS-2143-induced caspase activation in MDA-MB-231 cells [115]. |
| M30 Apoptosense ELISA | Serum-based ELISA that specifically detects caspase-cleaved CK18, a biomarker of epithelial apoptosis [116]. | Used in clinical trials to monitor apoptotic response to therapy. |
| M65 ELISA | Measures both full-length and cleaved CK18, serving as a biomarker for overall cell death (apoptosis and necrosis) [116]. | Often used in conjunction with M30 to dissect the mode of cell death. |
| qRT-PCR Primers | Gene-specific oligonucleotides for amplifying and quantifying mRNA transcripts of apoptotic genes. | Used to measure expression of BCL2, CASP3, let-7d, and miR-195 in breast tissues [46] [117]. |
Signaling Pathways and Logical Workflows
Apoptotic Signaling Pathways in Breast Cancer
The following diagram illustrates the interconnected biochemical pathways involving BCL-2, Caspase-3, and AIF1, contextualizing their roles in breast cancer cell fate.
Biomarker Validation Workflow
A logical workflow for the analytical and clinical validation of apoptotic biomarkers is essential for translational research.
The rigorous validation of AIF1, Caspase-3, and BCL-2 is of paramount importance for advancing the management of stage IV breast cancer. These biomarkers, operating at different nodes of the apoptotic machinery, provide a multi-dimensional view of tumor biology, from intrinsic survival signals (BCL-2) to the final execution of cell death (Caspase-3, AIF1). The integration of multiple techniques—from IHC and qRT-PCR on clinical specimens to functional activity assays in models—is essential to establish their prognostic and predictive power. As the field moves towards more personalized medicine, the combined assessment of these apoptotic regulators holds significant promise for identifying high-risk patients, predicting responses to conventional and targeted therapies, and ultimately, guiding the development of novel agents to overcome treatment resistance in advanced disease.
The biochemical process of apoptosis, or programmed cell death, is a critical mechanism targeted by systemic therapies in stage IV breast cancer. The efficacy of these treatments is profoundly influenced by the inherent molecular architecture of distinct breast cancer subtypes. Triple-negative breast cancer (TNBC), characterized by the absence of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) expression, constitutes approximately 15–20% of all breast cancers and demonstrates a proclivity for visceral metastasis and early recurrence [119] [120]. In contrast, HER2-positive breast cancer, defined by HER2 oncogene amplification, employs sophisticated signaling networks to suppress apoptosis and drive aggressive disease. This whitepaper provides a cross-subtype analysis of the apoptotic signaling pathways, elucidates the molecular foundations of treatment response and resistance, and details experimental methodologies for investigating cell death mechanisms, thereby offering a technical guide for therapeutic innovation in metastatic breast cancer.
Core Apoptotic Signaling Pathways
A comprehensive understanding of apoptosis begins with its two principal signaling cascades: the intrinsic and extrinsic pathways, which converge on a common execution phase.
The Intrinsic (Mitochondrial) Pathway
The intrinsic pathway is regulated by the B-cell lymphoma 2 (BCL-2) family of proteins, which govern mitochondrial outer membrane permeabilization (MOMP). MOMP leads to the release of cytochrome c into the cytosol [121]. Cytochrome c then binds to apoptotic protease-activating factor 1 (APAF1), forming the "apoptosome," a multi-protein complex that activates initiator caspase-9. Subsequently, caspase-9 cleaves and activates executioner caspases, such as caspase-3 and caspase-7 [122] [121]. The BCL-2 family comprises both pro-apoptotic (e.g., BAX, BAK, BIM, PUMA) and anti-apoptotic (e.g., BCL-2, BCL-xL, MCL-1) members. The delicate balance between these opposing factions determines cellular commitment to death.
The Extrinsic (Death Receptor) Pathway
The extrinsic pathway is initiated by the binding of specific extracellular death ligands—such as FAS ligand (FASL) or TNF-related apoptosis-inducing ligand (TRAIL)—to their corresponding death receptors (e.g., FAS, DR4, DR5) on the cell membrane [121]. This ligand-receptor interaction prompts the assembly of the death-inducing signaling complex (DISC), which recruits and activates initiator caspase-8. Active caspase-8 can then directly cleave and activate executioner caspases like caspase-3. Furthermore, caspase-8 can proteolytically activate the BH3-only protein BID, generating truncated BID (tBID), which translocates to the mitochondria and amplifies the apoptotic signal via the intrinsic pathway [122].
Convergent Execution Phase
Both the intrinsic and extrinsic pathways culminate in the activation of executioner caspases (e.g., caspase-3, -6, -7). These enzymes orchestrate the systematic dismantling of the cell by cleaving hundreds of cellular substrates, including structural proteins like cytokeratin 18 and nuclear proteins such as Poly (ADP-ribose) polymerase (PARP), leading to the characteristic morphological hallmarks of apoptosis [121].
The following diagram illustrates the core components and interconnectivity of these pathways:
Diagram Title: Core Apoptotic Signaling Pathways
Subtype-Specific Dysregulation of Apoptosis
HER2-Positive Breast Cancer: Orchestrated Survival
HER2 overexpression drives a multi-faceted suppression of apoptosis, primarily through the persistent activation of the PI3K-AKT signaling cascade, leading to profound therapeutic implications [122] [37].
Key Molecular Mechanisms:
- PI3K-AKT Signaling Hyperactivation: AKT phosphorylates multiple substrates to inhibit apoptosis. It phosphorylates the pro-apoptotic BH3-only protein BAD, leading to its sequestration by 14-3-3 proteins and inactivation [122]. AKT also phosphorylates caspase-9, directly reducing its catalytic activity, and promotes the nuclear export of FOXO transcription factors, suppressing the expression of their pro-apoptotic target genes like BIM [122].
- Suppression of p53 Activity: HER2 signaling enhances the MDM2-mediated ubiquitination and proteasomal degradation of the tumor suppressor p53. This diminishes the transcription of pivotal pro-apoptotic genes such as PUMA, NOXA, and BAX [122].
- Upregulation of Anti-Apoptotic Proteins: HER2-positive tumors frequently exhibit elevated levels of anti-apoptotic BCL-2 family members (BCL-2, BCL-xL, MCL-1) and the inhibitor of apoptosis (IAP) family protein survivin, which directly impedes caspase activation [122] [37].
- Mitochondrial Interference: Emerging evidence suggests that HER2 can localize to mitochondria, where it may directly inhibit the release of cytochrome c, adding another layer of apoptotic resistance [122].
Triple-Negative Breast Cancer (TNBC): Contextual Vulnerability and Resistance
TNBC lacks targeted receptors but possesses distinct apoptotic profiles, often characterized by high intrinsic cellular stress yet frequently developing resistance through alternative survival pathways.
Key Molecular Mechanisms:
- BCL-2 Family Dependence: While often considered highly aggressive, some TNBCs exhibit a degree of "primed" apoptosis, making them theoretically vulnerable. However, overexpression of anti-apoptotic proteins like BCL-2, BCL-xL, and MCL-1 is a common resistance mechanism to chemotherapy [123].
- p53 Inactivation: Somatic mutations in the TP53 gene are exceptionally common in TNBC, occurring in over 80% of cases [123]. This abrogates a critical DNA damage sensor and initiator of apoptosis, allowing tumor cells to survive despite genomic instability.
- Alternative Cell Death Regulators: Recent research highlights the prognostic significance of caspase-independent death effectors. For instance, elevated expression of Apoptosis-Inducing Factor 1 (AIF1) and the executioner caspase-3 in primary TNBC tumors is associated with a significant overall survival advantage, particularly in patients receiving chemotherapy [100].
- Enhanced DNA Damage Repair: A subset of TNBC, especially those with deficiencies in homologous recombination (HR) repair (e.g., BRCA1/2 mutations), initially exhibits hypersensitivity to DNA-damaging agents. However, restored HR proficiency via secondary mutations can lead to acquired resistance to platinum salts and PARP inhibitors [123] [124].
Table 1: Comparative Analysis of Apoptotic Pathway Dysregulation
| Apoptotic Component | HER2-Positive Breast Cancer | Triple-Negative Breast Cancer (TNBC) |
|---|---|---|
| Primary Initiator | Growth factor signaling (HER2/PI3K/AKT) | Genomic instability, cellular stress |
| BCL-2 Family | ↑ BCL-2, BCL-xL, MCL-1 [122] | Variable BCL-2; context-dependent priming [123] |
| p53 Status | Wild-type but degraded via MDM2 [122] | >80% mutation rate, leading to loss of function [123] |
| IAP Proteins | ↑ Survivin expression [122] [37] | Context-dependent expression |
| Key Resistance Mechanism | Redundant survival signals from PI3K/AKT [122] | Upregulated anti-apoptotic proteins, enhanced DNA repair [123] |
| Therapeutic Implication | Susceptible to HER2 + BCL-2 co-inhibition | Susceptible to DNA-damaging agents + apoptosis sensitizers |
The following pathway diagram synthesizes the distinct apoptotic regulation networks in HER2-positive and TNBC subtypes:
Diagram Title: Subtype-Specific Apoptotic Regulation
Quantitative Data Synthesis
The differential regulation of apoptosis translates into distinct clinical and pathological responses to therapy. The tables below synthesize key quantitative findings from the literature.
Table 2: Biomarker Expression and Correlation with Survival Outcomes
| Biomarker | Molecular Function | Subtype Association | Prognostic Correlation | Reference |
|---|---|---|---|---|
| Survivin | IAP, inhibits caspase activation | HER2-positive | Overexpression linked to poor outcomes | [122] |
| AIF1 | Caspase-independent apoptosis | TNBC | High protein/mRNA confers significant OS advantage (HR=0.48) | [100] |
| Caspase-3 (cleaved) | Executioner caspase | TNBC | Elevated expression grants significant OS advantage | [100] |
| BCL-2 | Anti-apoptotic (BCL-2 family) | HER2-positive; variable in TNBC | Overexpression associated with resistance; in TNBC, high levels can grant OS advantage | [122] [100] |
| TILs (Tumor-Infiltrating Lymphocytes) | Immune-mediated cell death | TNBC (IM subtype) | High levels associated with improved response and survival | [120] |
Table 3: Treatment Response Metrics by Subtype
| Therapeutic Context | Breast Cancer Subtype | Key Metric | Reported Value / Trend | Underlying Apoptotic Mechanism |
|---|---|---|---|---|
| Neoadjuvant Chemotherapy | TNBC (BL1 subtype) | Pathological Complete Response (pCR) | Higher rate | DDR activation and primed apoptosis [120] |
| Neoadjuvant Chemotherapy | TNBC (LAR subtype) | Pathological Complete Response (pCR) | Lower rate | Androgen receptor signaling, chemoresistance [120] |
| CWBI + BCS | TNBC & HER2-positive (no targeted therapy) | 5/10-year Local Recurrence Risk | ~2x higher vs. Luminal A | Innate radioresistance [125] |
| APBI | TNBC | 5-year IBTR Risk | Up to 33% | Residual disease survival post-chemo [125] |
| Platinum/PARPi | TNBC (BRCA-mutated) | Initial Response | High | HR deficiency, synthetic lethality [124] |
Detailed Experimental Protocols
To investigate the apoptotic pathways described, robust and reproducible experimental methodologies are essential. The following protocols are standardized for cross-subtype analysis.
Immunohistochemical (IHC) Profiling of Apoptotic Markers
This protocol is designed to quantify the expression and localization of key apoptotic proteins in formalin-fixed, paraffin-embedded (FFPE) breast tumor specimens.
Workflow Overview:
Diagram Title: IHC Staining Workflow
Detailed Procedure:
- Sectioning: Cut 4-5 µm thick sections from FFPE tissue blocks and mount them on charged slides.
- Deparaffinization and Rehydration: Immerse slides in xylene (2 changes, 10 minutes each), followed by a graded ethanol series (100%, 95%, 70%) and finally rinse in deionized water.
- Antigen Retrieval: Perform heat-induced epitope retrieval (HIER) using a citrate-based (pH 6.0) or EDTA-based (pH 9.0) buffer in a decloaking chamber or water bath at 95-100°C for 20-30 minutes. Cool slides to room temperature.
- Blocking and Antibody Incubation:
- Quench endogenous peroxidase activity with 3% hydrogen peroxide for 10 minutes.
- Block non-specific binding with 2.5% normal horse serum for 30 minutes at room temperature.
- Incubate with primary antibodies diluted in antibody diluent overnight at 4°C in a humidified chamber. Key antibodies include:
- Cleaved Caspase-3 (Asp175): To detect activated caspase-3.
- BCL-2: As a key anti-apoptotic marker.
- AIF1: For caspase-independent apoptosis.
- Ki-67: As a proliferation marker for context.
- Detection: Apply a labeled polymer-horseradish peroxidase (HRP) secondary antibody system (e.g., ImmPRESS system) for 30-60 minutes at room temperature. Visualize using 3,3'-Diaminobenzidine (DAB) as the chromogen for 5-10 minutes, developing a brown precipitate at the antigen site.
- Counterstaining and Mounting: Counterstain with hematoxylin to visualize nuclei, dehydrate through graded alcohols and xylene, and mount with a synthetic mounting medium.
- Scoring and Analysis: Evaluate stained slides by a pathologist blinded to the clinical data. Use a semi-quantitative scoring system like the H-score (which incorporates staining intensity and the percentage of positive tumor cells) or the Allred score. Digital image analysis can be employed for objectivity and reproducibility.
BH3 Profiling to Measure Apoptotic Priming
BH3 profiling is a functional assay that measures mitochondrial priming—the proximity of a cell to the apoptotic threshold—by quantifying its dependence on specific anti-apoptotic proteins [121].
Detailed Procedure:
- Cell Preparation: Use single-cell suspensions from fresh or viably frozen tumor tissue or cultured cell lines. Isolate tumor cells using magnetic bead-based or FACS sorting if working with heterogeneous samples.
- Permeabilization: Permeabilize cells with digitonin-containing buffer to allow BH3 peptides access to the mitochondria while retaining cytochrome c.
- BH3 Peptide Exposure: Incubate permeabilized cells with a panel of synthetic BH3 domain peptides (e.g., BIM, BAD, HRK, MS1) for 60-90 minutes at room temperature or 37°C. Each peptide has specific binding profiles; for example, BAD indicates dependence on BCL-2/BCL-xL, while MS-1 indicates MCL-1 dependence.
- Cytochrome c Release Quantification: Fix the cells and stain with an anti-cytochrome c antibody. Analyze the percentage of cells that have released cytochrome c by flow cytometry.
- Data Interpretation: A high percentage of cytochrome c release after exposure to a "priming" peptide like BIM indicates a high overall level of mitochondrial priming, suggesting susceptibility to apoptosis. Selective sensitivity to specific peptides (e.g., BAD) identifies which anti-apoptotic protein(s) the cell is dependent on for survival.
Immunoblotting (Western Blot) for Caspase Activation
This protocol detects the cleavage and activation of caspases and their substrates (e.g., PARP) as direct evidence of apoptosis execution.
Detailed Procedure:
- Protein Extraction: Lyse cell pellets or pulverized tumor tissue in RIPA buffer supplemented with protease and phosphatase inhibitors. Determine protein concentration using a BCA or Bradford assay.
- Gel Electrophoresis: Separate equal amounts of protein (20-40 µg) by SDS-PAGE on 4-20% gradient gels and transfer to PVDF or nitrocellulose membranes.
- Antibody Probing:
- Block membranes with 5% non-fat milk in TBST for 1 hour.
- Incubate with primary antibodies against target proteins (e.g., Caspase-3, Cleaved Caspase-3, PARP, Cleaved PARP) diluted in blocking buffer overnight at 4°C.
- Wash membranes and incubate with appropriate HRP-conjugated secondary antibodies for 1 hour at room temperature.
- Detection and Analysis: Detect signal using enhanced chemiluminescence (ECL) substrate and image with a digital imager. The appearance of cleaved caspase-3 and cleaved PARP fragments (e.g., 89 kDa) is a definitive biochemical marker of ongoing apoptosis.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Apoptosis Research in Breast Cancer
| Research Tool | Specific Example(s) | Primary Function in Experimentation | Key Application in Subtype Analysis |
|---|---|---|---|
| Anti-Cleaved Caspase-3 IHC Antibody | Rabbit monoclonal (Asp175) | Detects activated/executioner caspase-3 in FFPE tissue | Measure baseline apoptosis and therapy-induced cell death in TNBC vs. HER2+ xenografts [100] |
| BH3 Peptides | BIM, BAD, MS-1, HRK | Functional profiling of mitochondrial apoptotic dependency | Identify BCL-2 family dependencies (e.g., MCL-1 in HER2+; BCL-2 in some TNBC) for targeted inhibition [121] |
| PARP Cleavage WB Antibody | Anti-PARP (46D11) | Detects full-length (116 kDa) and cleaved (89 kDa) PARP as apoptosis marker | Confirm activation of execution phase caspases in vitro after drug treatment [121] |
| Recombinant Death Ligands | TRAIL, FASL | Activate the extrinsic apoptotic pathway via death receptors | Test sensitivity of HER2+ vs. TNBC cell lines to immune-mediated killing [122] |
| Small Molecule Inhibitors | ABT-199 (Venetoclax - BCL-2), A-1331852 (BCL-xL), S63845 (MCL-1) | Specifically inhibit anti-apoptotic BCL-2 family proteins | Investigate synthetic lethality when combined with HER2 or DNA-damaging agents in specific subtypes [123] [121] |
| SMAC Mimetics | LCL161, Birinapant | Antagonize IAP proteins like XIAP, relieving caspase inhibition | Overcome survivin-mediated resistance in HER2+ models or sensitize resistant TNBC cells [121] |
The translation of preclinical discoveries into clinically viable therapies represents a critical pathway in advancing oncology care. Within stage IV breast cancer, the deliberate targeting of the biochemical process of apoptosis has yielded some of the most significant breakthroughs in treatment, alongside notable failures that provide instructive lessons. This review examines the mechanistic successes of HER2-targeted therapies and nanoparticle-mediated drug delivery, which promote apoptotic cell death through distinct signaling pathways. It also analyzes translational failures stemming from poor preclinical model predictivity and overlooked resistance mechanisms. A comprehensive synthesis of clinical trial data, experimental methodologies, and emerging technologies is presented to guide future research and development efforts aimed at exploiting apoptotic pathways for therapeutic benefit in advanced breast cancer.
Breast cancer remains a leading cause of cancer-related mortality in women worldwide, with stage IV or metastatic disease presenting particular therapeutic challenges due to its heterogeneity and capacity for treatment resistance [106]. The process of apoptosis, or programmed cell death, serves as a critical regulatory mechanism for eliminating malignant cells, and its dysregulation constitutes a hallmark of cancer [21] [64]. The "bench-to-bedside" paradigm describes the translational pathway from basic scientific discovery to clinical application, a journey particularly exemplified in the development of apoptosis-targeting therapies for advanced breast cancer.
Figure 1: The Bench-to-Bedside Translation Pathway
In stage IV breast cancer, malignant cells evade apoptosis through multiple mechanisms, including upregulation of anti-apoptotic proteins (e.g., Bcl-2, Bcl-xL), loss of pro-apoptotic factors, impaired death receptor signaling, and defective caspase activation [21] [106]. The successful translation of apoptosis-targeting agents requires a deep understanding of these molecular adaptations and the development of strategies to overcome them. This review examines both triumphant and unsuccessful translational efforts, with a specific focus on the biochemical basis of apoptotic regulation in advanced breast cancer and its implications for therapeutic development.
Biochemical Foundations of Apoptosis in Breast Cancer
Core Apoptotic Signaling Pathways
Apoptosis occurs through two principal signaling cascades: the extrinsic (death receptor) pathway and the intrinsic (mitochondrial) pathway. In breast cancer, both pathways are frequently dysregulated, contributing to treatment resistance and disease progression.
Figure 2: Apoptotic Signaling Pathways in Breast Cancer
The intrinsic pathway is regulated by the Bcl-2 family of proteins, which includes both pro-apoptotic (e.g., Bax, Bak, Bad) and anti-apoptotic (e.g., Bcl-2, Bcl-xL) members. In response to cellular stress, DNA damage, or growth factor deprivation, pro-apoptotic proteins permeabilize the mitochondrial outer membrane, facilitating cytochrome c release and subsequent caspase activation [21] [64]. The extrinsic pathway is initiated by ligand binding to death receptors (e.g., FAS, TRAIL-R) at the cell surface, leading to caspase-8 activation. Both pathways converge on the activation of executioner caspases (caspase-3, -6, and -7), which orchestrate the systematic dismantling of the cell [106].
Apoptosis Detection Methodologies
Accurate assessment of apoptosis in both preclinical models and clinical specimens is essential for translational research. Key methodological approaches include:
Table 1: Core Methodologies for Apoptosis Detection in Breast Cancer Research
| Method | Principle | Applications | Key Advantages | Limitations |
|---|---|---|---|---|
| TUNEL Assay | Labels DNA strand breaks | Tissue sections, cell culture | High specificity for late apoptosis | Cannot differentiate from necrosis |
| Caspase Activity Assays | Measures protease cleavage | Cell lysates, live cells | Quantitative, pathway-specific | Does not confirm cell death |
| Annexin V/PI Staining | Detects phosphatidylserine exposure | Flow cytometry | Distinguishes early vs. late apoptosis | Requires single-cell suspension |
| Mitochondrial Membrane Potential (ΔΨm) | Fluorescent dye retention | Flow cytometry, microscopy | Early apoptotic events | Non-specific for apoptosis |
| Western Blotting | Detects cleavage products (PARP, caspases) | Cell/tissue lysates | Mechanistic insight, multiple targets | Semi-quantitative, no single-cell data |
The TUNEL (terminal deoxynucleotidyl transferase dUTP nick end labeling) assay has been widely used to detect DNA fragmentation, a hallmark of apoptotic cell death, in breast cancer tissue specimens [21]. This technique can be applied to formalin-fixed, paraffin-embedded clinical material, enabling retrospective analysis of apoptosis in tumor biopsies obtained before, during, and after treatment. However, it provides only a snapshot of a dynamic process and cannot distinguish between apoptosis and necrosis without simultaneous morphological assessment [21].
Success Stories in Translational Apoptosis Research
HER2-Targeted Therapies: A Paradigm Shift
The development of HER2-targeted agents represents one of the most successful examples of bench-to-bedside translation in oncology. HER2 amplification occurs in approximately 15-20% of invasive breast cancers and has been historically associated with aggressive disease behavior and poor prognosis [126].
Mechanistic Insights: Trastuzumab, a humanized monoclonal antibody targeting the extracellular domain of HER2, promotes apoptosis through multiple mechanisms: (1) inhibition of HER2-mediated intracellular signaling cascades, particularly the MAPK and PI3K pathways; (2) induction of antibody-dependent cellular cytotoxicity (ADCC); and (3) prevention of HER2 extracellular domain cleavage [126]. The critical role of apoptosis induction in the therapeutic efficacy of trastuzumab was established in preclinical models, where treatment led to cell cycle arrest and suppression of proliferation through modulation of Bcl-2 family proteins and caspase activation [126].
Clinical Translation: Pivotal clinical trials demonstrated that the addition of trastuzumab to first-line chemotherapy significantly improved time to progression (7.4 vs. 4.6 months) and overall survival (25.1 vs. 20.3 months) in patients with HER2-positive metastatic breast cancer [126]. Subsequent development of additional HER2-targeted agents, including pertuzumab, ado-trastuzumab emtansine (T-DM1), and trastuzumab deruxtecan (T-DXd), has further improved outcomes through enhanced apoptotic induction.
Table 2: Evolution of HER2-Targeted Therapies in Metastatic Breast Cancer
| Therapeutic Agent | Mechanism of Action | Key Clinical Trial | Progression-Free Survival | Overall Survival |
|---|---|---|---|---|
| Trastuzumab + Chemotherapy | HER2 monoclonal antibody | Slamon et al. (2001) | 7.4 months | 25.1 months |
| Trastuzumab + Pertuzumab + Docetaxel | Dual HER2 blockade | CLEOPATRA | 18.5 months | 56.5 months |
| T-DM1 | Antibody-drug conjugate | EMILIA | 9.6 months | 29.9 months |
| T-DXd | Antibody-drug conjugate | DESTINY-Breast03 | 28.8 months | Not Reached |
The success of HER2-targeted therapies underscores the importance of targeting specific molecular drivers of cancer cell survival and apoptosis resistance. The continuous refinement of these approaches, from monoclonal antibodies to antibody-drug conjugates, demonstrates how iterative translational research can substantially improve patient outcomes in stage IV breast cancer [126].
Nanomedicine Approaches for Apoptosis Induction
Nanoparticle-based drug delivery systems have emerged as a promising strategy to enhance the efficacy and reduce the toxicity of apoptosis-inducing agents in breast cancer treatment.
Mechanistic Basis: Nanocarriers, including lipid-based nanoparticles, polymeric nanoparticles, and inorganic nanoparticles, improve drug delivery through multiple mechanisms: (1) enhanced permeability and retention (EPR) effect for passive tumor targeting; (2) surface functionalization with targeting ligands for active targeting; and (3) controlled release profiles that maintain therapeutic drug concentrations [127] [128]. These systems can deliver chemotherapeutic agents, nucleic acids, and immunomodulators directly to tumor cells, maximizing apoptotic induction while minimizing off-target effects.
Clinical Applications: Several nanomedicines have received regulatory approval for cancer treatment, including liposomal doxorubicin (Doxil) and albumin-bound paclitaxel (Abraxane). These formulations demonstrate improved therapeutic indices compared to their conventional counterparts, with reduced cardiotoxicity (doxorubicin) and hypersensitivity reactions (paclitaxel) [127] [128]. Ongoing clinical trials are investigating novel nanoparticle-based approaches for stage IV breast cancer, including targeted delivery of pro-apoptotic small interfering RNAs (siRNAs) and combination therapies that simultaneously engage multiple apoptotic pathways.
The Scientist's Toolkit: Essential Reagents for Apoptosis and Nanomedicine Research
| Research Tool | Function | Application Examples |
|---|---|---|
| Recombinant Death Receptor Ligands | Activate extrinsic apoptosis pathway | FASL, TRAIL in therapeutic studies |
| Caspase Inhibitors | Mechanistic studies of apoptosis | Z-VAD-FMK for pathway validation |
| BH3 Mimetics | Inhibit anti-apoptotic Bcl-2 proteins | Venetoclax (ABT-199) in clinical trials |
| Fluorescent Caspase Substrates | Real-time apoptosis monitoring | DEVD-AMC for caspase-3/7 activity |
| Polymeric Nanoparticles | Drug delivery vehicles | PLGA-PEG for controlled drug release |
| Lipid Nanoparticles | Nucleic acid delivery | siRNA targeting anti-apoptotic genes |
| Targeting Ligands | Cell-specific delivery | HER2 antibodies, RGD peptides |
Translational Failures and Lessons Learned
Limitations of Preclinical Models
The failure of many promising apoptosis-targeting agents to demonstrate efficacy in clinical trials often reflects limitations in preclinical model systems. Key discrepancies include:
Tumor Microenvironment Complexity: Traditional cell line-based xenograft models inadequately recapitulate the tumor-stromal interactions, immune context, and metabolic conditions of human breast cancers. This is particularly relevant for apoptosis induction, as the tumor microenvironment can confer profound resistance to cell death signals [129] [128]. For example, the failure of EGFR and VEGF inhibitor combinations in breast cancer, despite promising preclinical data, has been attributed in part to inability to accurately model tumor heterogeneity and stromal effects in murine systems [129].
Molecular Heterogeneity: The classification of breast cancer into molecular subtypes (luminal A, luminal B, HER2-enriched, basal-like) has revealed substantial genetic and phenotypic diversity that is often poorly represented in standard preclinical models. Agents demonstrating efficacy in genetically homogeneous model systems may fail in clinically heterogeneous patient populations [129] [130]. This is particularly evident in triple-negative breast cancer, where numerous targeted agents have shown limited clinical benefit despite robust preclinical activity.
Overcoming Resistance to Apoptosis Induction
The development of resistance to apoptosis-inducing therapies represents a major challenge in stage IV breast cancer. Key resistance mechanisms include:
Upregulation of Anti-Apoptotic Proteins: Increased expression of Bcl-2, Bcl-xL, and Mcl-1 can confer resistance to diverse chemotherapeutic agents and targeted therapies [21] [64]. This is particularly relevant in estrogen receptor-positive breast cancer, where Bcl-2 expression is frequently elevated and associated with improved survival but may also contribute to endocrine therapy resistance [21].
Impaired Death Receptor Signaling: Downregulation of death receptors or upregulation of decoy receptors can limit the efficacy of death receptor-targeted therapies [106]. Additionally, epigenetic modifications that silence caspase expression or activity represent another mechanism of apoptosis resistance.
Figure 3: Mechanisms of Apoptosis Resistance in Breast Cancer
Case Study: Podophyllotoxin Derivatives
The development of podophyllotoxin (PPT)-based chemotherapeutic agents illustrates both the challenges and opportunities in translating natural products into clinically effective apoptosis-inducing agents. PPT, a potent tubulin inhibitor isolated from Podophyllum plants, demonstrates significant antitumor activity but is limited by poor water solubility, toxicity, and inadequate stability [131].
Translational Strategies: Semi-synthetic derivatives, including etoposide, teniposide, and etopophos, were developed to improve the therapeutic profile of PPT. These agents inhibit topoisomerase II, leading to DNA damage and apoptosis induction [131]. While clinically valuable, these derivatives are associated with significant adverse effects, including nausea, cardiomyopathy, and myelosuppression, limiting their utility in heavily pretreated stage IV breast cancer patients.
Nanomedicine Approaches: Recent advances have focused on PPT-based nanoplatforms, including liposomes, polymeric micelles, and polymer-drug conjugates, to enhance tumor-specific delivery and improve the efficacy-toxicity balance [131]. These systems utilize passive targeting (EPR effect), active targeting (ligand-receptor interactions), and stimulus-responsive targeting (pH, enzymes) to maximize drug delivery to tumor cells while minimizing exposure to normal tissues. Combination approaches integrating PPT-based chemotherapy with photodynamic therapy, photothermal therapy, and immunotherapy represent promising strategies to overcome apoptosis resistance in advanced breast cancer [131].
Emerging Technologies and Future Directions
Advanced Preclinical Models
The development of more physiologically relevant model systems is critical for improving the predictivity of preclinical apoptosis research. Key advances include:
Patient-Derived Xenografts (PDXs): These models, established by implanting patient tumor tissue directly into immunocompromised mice, better maintain the genetic and phenotypic heterogeneity of original tumors. PDXs have demonstrated utility in predicting clinical response to targeted therapies and identifying biomarkers of apoptosis sensitivity [129].
Organoid and Microfluidic Systems: Three-dimensional organoid cultures and "tumor-on-a-chip" platforms recapitulate key aspects of the tumor microenvironment, enabling high-throughput screening of apoptosis-inducing agents in more physiologically relevant contexts [128]. These systems permit real-time monitoring of apoptotic events and can be used to assess combination therapies targeting multiple resistance mechanisms simultaneously.
Biomimetic Nanomedicines
The integration of biological components with synthetic nanocarriers represents a promising approach to enhance drug delivery to metastatic breast cancer sites. Biomimetic strategies include:
Cell Membrane-Coated Nanoparticles: Coating synthetic nanocarriers with membranes derived from platelets, leukocytes, or cancer cells can confer enhanced circulation, immune evasion, and tumor-targeting capabilities [128]. For example, platelet membrane-coated nanoparticles have demonstrated improved delivery to metastatic sites through interactions with circulating tumor cells and the tumor vasculature.
Exosome-Based Delivery Systems: Exosomes, natural extracellular vesicles involved in intercellular communication, can be engineered to deliver pro-apoptotic cargo, including siRNAs, microRNAs, and chemotherapeutic agents, to specific cell populations [128]. These systems leverage natural trafficking pathways to overcome biological barriers that limit conventional nanocarriers.
Artificial Intelligence in Translational Research
Artificial intelligence (AI) and machine learning approaches are transforming multiple aspects of apoptosis research and drug development:
Predictive Modeling: AI algorithms can integrate multi-omic data to predict tumor vulnerability to specific apoptosis-inducing agents, facilitating patient selection for clinical trials and ultimately guiding personalized therapy [128].
Drug Discovery: Machine learning approaches can identify novel compounds with pro-apoptotic activity or predict optimal nanocarrier properties for specific therapeutic applications, accelerating the drug development pipeline [128].
Clinical Trial Optimization: AI-based analysis of digital pathology images can quantify apoptotic events in tumor biopsies with greater accuracy and reproducibility than manual assessment, enabling more precise evaluation of treatment response in clinical trials [128].
The targeted induction of apoptosis remains a cornerstone of therapeutic development for stage IV breast cancer. Successes such as HER2-targeted therapies demonstrate the profound impact of targeting specific molecular vulnerabilities, while failures provide critical insights into the complexity of apoptotic regulation and the limitations of current model systems. The continued integration of advanced technologies, including nanomedicine, biomimetic delivery systems, and artificial intelligence, holds promise for overcoming existing barriers to clinical translation. As our understanding of the biochemical basis of apoptosis in breast cancer continues to evolve, so too will our ability to develop more effective, personalized approaches for targeting this critical cell death pathway in advanced disease.
In stage IV breast cancer, the dysregulation of apoptosis is a cornerstone of disease progression and treatment resistance. Apoptosis, a genetically programmed cell death process, is essential for maintaining tissue homeostasis and eliminating damaged cells. In advanced breast cancer, malignant cells evade this process through multiple mechanisms, including the overexpression of anti-apoptotic proteins and defects in key signaling pathways. The biochemical landscape of stage IV disease is characterized by complex molecular adaptations that suppress apoptotic signals, enabling cancer cells to survive, proliferate, and develop resistance to conventional therapies. Recent advances in understanding these mechanisms have revealed promising therapeutic opportunities through targeted modulation of apoptosis pathways, particularly when integrated with immunotherapy and other targeted agents. This whitepaper examines the current scientific knowledge on apoptosis modulation in advanced breast cancer, with a focus on integrating these approaches for improved clinical outcomes.
Molecular Mechanisms of Apoptosis in Breast Cancer
Core Apoptotic Pathways and Their Regulation
The execution of apoptosis occurs through two primary pathways that converge on caspase activation:
Intrinsic (Mitochondrial) Pathway: Regulated by the Bcl-2 protein family, this pathway activates in response to intracellular stressors including DNA damage, oxidative stress, and oncogenic signaling. Key events include mitochondrial outer membrane permeabilization (MOMP), cytochrome c release, and formation of the apoptosome complex, which activates caspase-9 [132].
Extrinsic (Death Receptor) Pathway: Initiated by extracellular death ligands binding to cell surface death receptors, leading to formation of the death-inducing signaling complex (DISC) and activation of caspase-8 [132].
Both pathways converge on the activation of executioner caspases (caspase-3, -6, and -7), which mediate the proteolytic cleavage of cellular components and final stages of cell death [132].
Key Anti-Apoptotic Proteins as Therapeutic Targets
The Inhibitor of Apoptosis Proteins (IAPs) family represents crucial regulatory checkpoints that are frequently overexpressed in breast cancer. These proteins function as potent caspase inhibitors and contribute to treatment resistance:
- XIAP (X-linked IAP): Directly binds to and inhibits caspases-3, -7, and -9, constituting the most potent endogenous caspase inhibitor among IAPs [133].
- c-IAP1 and c-IAP2: Regulate apoptosis primarily through their E3 ubiquitin ligase activity and modulation of NF-κB signaling pathways rather than direct caspase inhibition [133].
- Survivin: Functions through complex formation with other IAPs and directly interacts with SMAC/DIABLO and caspases [133].
- BRUCE/Apollon: Acts as both a suppressor of apoptosis and an E3 ubiquitin ligase, inhibiting pro-apoptotic SMAC/DIABLO and HtrA2/Omi [133].
Table 1: Key Inhibitor of Apoptosis Proteins (IAPs) in Breast Cancer
| IAP Family Member | Primary Mechanism of Action | Functional Consequences in Cancer |
|---|---|---|
| XIAP | Direct inhibition of caspases-3, -7, and -9 | Prevents execution of apoptosis; confers chemotherapy resistance |
| c-IAP1/c-IAP2 | E3 ubiquitin ligase activity; modulates NF-κB signaling | Regulates survival pathways; suppresses formation of pro-apoptotic complexes |
| Survivin | Complex formation with other IAPs; binds SMAC and caspases | Stabilizes XIAP; inhibits caspase activation |
| BRUCE/Apollon | E3 ubiquitin ligase; inhibits SMAC/DIABLO and HtrA2/Omi | Targets pro-apoptotic proteins for degradation; maintains mitochondrial integrity |
The diagram below illustrates the core apoptotic pathways and key regulatory nodes targeted by therapeutic agents in breast cancer:
Current Apoptosis-Targeting Strategies in Clinical Development
SMAC Mimetics and IAP Antagonists
SMAC (Second Mitochondria-derived Activator of Caspases) mimetics represent a promising class of investigational compounds that target IAPs for degradation:
Mechanism of Action: These small molecules mimic the endogenous SMAC/DIABLO protein, which normally counteracts IAP-mediated caspase inhibition. SMAC mimetics bind to IAPs, particularly cIAP1 and cIAP2, promoting their auto-ubiquitination and proteasomal degradation [133] [134].
Therapeutic Effects: Degradation of cIAPs leads to several pro-apoptotic consequences: (1) sensitization to death receptor signaling; (2) reduction of NF-κB activation; (3) release of caspase inhibition; and (4) promotion of necroptosis in some cellular contexts [133].
Clinical Experience: Preclinical studies in breast cancer models demonstrate that SMAC mimetics can overcome resistance to conventional therapies. As single agents, they show limited efficacy, but in combination with other therapeutics, they significantly enhance apoptosis induction [134].
Kinase-Targeted Approaches in Apoptosis Modulation
Protein kinases play crucial regulatory roles in apoptosis pathways, making them attractive therapeutic targets:
PI3K/AKT/mTOR Pathway: This frequently dysregulated pathway in breast cancer promotes cell survival and suppresses apoptosis. Inhibitors targeting various nodes in this pathway can restore apoptotic sensitivity [132].
Tyrosine Kinases: EGFR and SRC family kinases demonstrate significantly elevated expression in breast cancer tissues and contribute to apoptosis resistance through multiple signaling pathways [132].
Combination Strategies: Research indicates that combining kinase inhibitors with apoptosis modulators can produce synergistic effects. For instance, the combination of an apoptosis inducer with an AKT inhibitor demonstrated enhanced activity in hormone-resistant breast cancer cells [108].
Table 2: Quantitative Assessment of Apoptosis-Targeting Agents in Breast Cancer
| Therapeutic Class | Specific Agents/Compounds | Experimental Model | Efficacy Metrics | Combination Synergy |
|---|---|---|---|---|
| SMAC Mimetics | LCL161, Birinapant | Breast cancer cell lines; xenograft models | IC~50~: 1-5 µM; Tumor growth inhibition: 60-80% | CI: 0.4-0.8 with AKT inhibitors [108] |
| AKT Inhibitors | AKT Inhibitor IV, Ipatasertib | MCF7, MCF7/HT cells | IC~50~: 2-5 µM; Apoptosis induction: 40-60% | CI: 0.4 with LCTA-3344 [108] |
| PARP Inhibitors | Olaparib, Talazoparib | BRCA-mutant breast cancer; clinical trials | 3-year IDFS: 85.9% vs 77.1% with placebo [113] | Synthetic lethality in HR-deficient tumors |
| Natural Compounds | Icariin (ICA) | TNBC cell lines | Autophagy inhibition; ROS-mediated apoptosis | Dual action on autophagy and apoptosis [135] |
Integration with Immunotherapy Platforms
Immune Checkpoint Inhibitors and Apoptosis Modulation
The tumor microenvironment in stage IV breast cancer creates significant immunosuppressive barriers that can be overcome through strategic combinations:
Dendritic Cell Vaccines: Personalized dendritic cell vaccines have demonstrated response rates exceeding 90% in some studies, with mechanism involving enhanced antigen presentation and T-cell priming [136].
PD-1/PD-L1 Inhibitors: These agents can synergize with apoptosis inducers by promoting immunogenic cell death and enhancing T-cell-mediated killing of tumor cells [136] [137].
TIL and CAR T-cell Therapies: Adoptive cell transfer approaches benefit from apoptosis induction, which increases tumor antigen availability and reduces immunosuppressive factors [136].
Immunogenic Cell Death and Apoptosis
Certain apoptosis-inducing agents can stimulate immunogenic cell death (ICD), characterized by the surface exposure of calreticulin and release of ATP and HMGB1. These damage-associated molecular patterns (DAMPs) promote dendritic cell maturation and antigen presentation, enhancing antitumor immunity [136] [132].
Experimental Models and Methodological Approaches
In Vitro Assessment of Apoptosis Modulation
Research into apoptosis modulation requires robust experimental models and methodologies:
Cell Line Models: Hormone-sensitive (MCF7) and resistant (MCF7/HT) breast cancer cell lines enable study of resistance mechanisms. Triple-negative breast cancer (TNBC) models (MDA-MB-231, BT-549) are particularly relevant for immunotherapy combinations [108].
Apoptosis Detection Methods: Techniques include morphological assessment, TUNEL assay for DNA fragmentation, caspase activity assays, and flow cytometry with Annexin V/propidium iodide staining [21].
Synergy Assessment: The Combination Index (CI) method quantitatively evaluates drug interactions, with CI < 0.9 indicating synergy, CI = 0.9-1.1 indicating additive effects, and CI > 1.1 indicating antagonism [108].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Apoptosis Studies
| Research Tool Category | Specific Examples | Experimental Application | Key Readouts |
|---|---|---|---|
| Apoptosis Inducers | 1-substituted isatin-5-sulfonamides (LCTA-3344) [108] | Mechanism studies in hormone-resistant models | IC~50~ values; caspase activation |
| SMAC Mimetics | LCL161, Birinapant [133] [134] | IAP inhibition studies; combination therapies | cIAP1 degradation; TNFα sensitivity |
| Kinase Inhibitors | AKT Inhibitor IV, HSP90 inhibitors [108] [132] | Pathway analysis; combination screening | Phospho-protein profiling; synergy metrics |
| Natural Compounds | Icariin (ICA) [135] | Autophagy-apoptosis crosstalk studies | ROS measurement; DRP1-mediated fission |
| Detection Reagents TUNEL assay kits; caspase activity assays; Annexin V conjugates [21] | Apoptosis quantification in treated cells | Apoptotic indices; caspase cleavage | |
| Cell Line Models | MCF7, MCF7/HT, MDA-MB-231 [108] [135] | Therapy response assessment; resistance modeling | Resistance indices; gene expression profiles |
The experimental workflow for evaluating apoptosis-modulating therapies typically follows this pathway:
Biomarkers and Patient Stratification Strategies
Predictive Biomarkers for Apoptosis-Targeted Therapies
Identifying appropriate biomarkers is crucial for successful clinical development of apoptosis-modulating agents:
IAP Expression Profiles: Immunohistochemical assessment of XIAP, cIAP1/2, and survivin can identify tumors dependent on these anti-apoptotic proteins [133] [21].
Programmed Cell Death Signatures: Multi-gene expression signatures encompassing 19 different programmed cell death patterns can stratify patients by prognosis and therapeutic response [138].
HRD and BRCA Status: Homologous recombination deficiency (HRD) and BRCA1/2 mutations predict sensitivity to PARP inhibitors and potentially to combinations with apoptosis modulators [113].
Molecular Subtyping for Targeted Application
Breast cancer molecular subtypes demonstrate distinct apoptosis regulation mechanisms:
Triple-Negative Breast Cancer (TNBC): Characterized by high genomic instability and frequent dysregulation of apoptosis pathways, making it particularly susceptible to IAP inhibition and immune checkpoint combinations [137].
Hormone Receptor-Positive (HR+) Breast Cancer: Often exhibits overexpression of Bcl-2 and other anti-apoptotic proteins, contributing to endocrine therapy resistance [108] [21].
HER2-Positive Breast Cancer: HER2 signaling activates multiple survival pathways, including PI3K/AKT, which can be targeted with combination approaches [132].
Clinical Translation and Future Perspectives
Clinical Trial Evidence and Emerging Data
Recent clinical trials provide encouraging evidence for apoptosis-focused combinations:
PARP Inhibitors in BRCA-Mutant Breast Cancer: The phase III OlympiA trial demonstrated significant improvement in invasive disease-free survival (85.9% vs. 77.1% with placebo) and overall survival with adjuvant olaparib in gBRCAmut, HER2-negative breast cancer [113].
Immunotherapy Combinations: Early-phase trials combining PD-1/PD-L1 inhibitors with apoptosis modulators show enhanced response rates, particularly in TNBC, with ongoing studies optimizing dosing schedules [136] [137].
Novel Agent Development: Next-generation PARP1-selective inhibitors (e.g., AZD5305) aim to reduce hematologic toxicity while maintaining efficacy, and combinations with antibody-drug conjugates show promising activity beyond BRCA-mutated cancers [113].
Challenges and Future Research Directions
Several challenges remain in optimally integrating apoptosis modulation with other treatment modalities:
Resistance Mechanisms: Tumor cells can develop resistance through multiple mechanisms, including upregulation of alternative survival pathways, reduced drug accumulation, and mutations in apoptotic components [133] [113].
Therapeutic Index Optimization: Balancing efficacy with toxicity remains challenging, particularly when combining multiple targeted agents [132].
Biomarker Refinement: Developing more precise biomarkers to identify patients most likely to benefit from specific combinations requires further research [138] [137].
Future research should focus on rational combination designs based on comprehensive molecular profiling, development of resistance-overcoming strategies, and innovative clinical trial designs that incorporate adaptive methodologies and translational endpoints.
Conclusion
The intricate biochemical process of apoptosis remains a cornerstone for understanding progression and treatment failure in stage IV breast cancer. A deep understanding of the core pathways, coupled with advanced methodological tools for detection and a clear strategy to overcome resistance, is paramount. The future of treating advanced breast cancer lies in validated, personalized approaches that integrate novel apoptosis-targeting agents, rational combination strategies, and robust biomarker-guided therapies to effectively counter tumor heterogeneity and evasion mechanisms, ultimately improving patient outcomes.
References
- 1. Apoptosis and the Response to Anti-Cancer Drugs - Anticancer Drug Action Laboratory - Mayo Clinic Research [https://www.mayo.edu/research/labs/anticancer-drug-action/research-projects/apoptosis-response-anticancer-drugs]
- 2. Mitochondrial metabolism and cancer therapeutic innovation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319113/]
- 3. Biomarkers of apoptosis : release of cytochrome , activation of... c [https://pubmed.ncbi.nlm.nih.gov/11503418/]
- 4. - Wikipedia Cytochrome c [https://en.wikipedia.org/wiki/Cytochrome_c]
- 5. Cell Death Effect of Scrophularia Variegata on Apoptosis ... Breast [https://pmc.ncbi.nlm.nih.gov/articles/PMC4616888/]
- 6. Effectiveness of Graphene Oxide (GO) in Activating the Mitochondrial Pathway of Oxidative Stress-Induced Apoptosis in Breast Cancer Cells [https://www.mdpi.com/2073-4409/14/21/1717]
- 7. Estrogen regulation of apoptosis : how can one hormone stimulate and... [https://breast-cancer-research.biomedcentral.com/articles/10.1186/bcr2255]
- 8. Advances in novel cell death mechanisms in breast cancer: intersecting perspectives on ferroptosis, cuproptosis, disulfidptosis, and pyroptosis | Molecular Cancer | Full Text [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02445-0]
- 9. of Procaspase- Mechanisms in the 8 ... Activation Extrinsic [https://link.springer.com/article/10.1134/S0026893319050091]
- 10. of Cell Mechanisms : Death | Intrinsic & Apoptosis Pathways Extrinsic [https://blog.cellsignal.com/mechanisms-of-cell-death-apoptosis]
- 11. - Caspase in inflammatory diseases: a potential therapeutic target 8 [https://cmbl.biomedcentral.com/articles/10.1186/s11658-024-00646-x]
- 12. Caspase-8 cleaves its substrates from the plasma membrane upon CD95-induced apoptosis | Cell Death & Differentiation [https://www.nature.com/articles/cdd2012156]
- 13. Decoding breast cancer treatment resistance through genetic, epigenetic, and immune-regulatory mechanisms: from molecular insights to translational perspectives [https://www.oaepublish.com/articles/cdr.2025.69]
- 14. The molecular mechanism of apoptosis upon caspase-8 activation: Quantitative experimental validation of a mathematical model - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0167488912001991]
- 15. Vitex Rotundifolia Fractions Induced Apoptosis in Human Breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7173364/]
- 16. Antiproliferative and apoptotic effects of black turtle bean extracts on... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-017-0281-5]
- 17. A mathematical model of caspase function in apoptosis - PubMed [https://pubmed.ncbi.nlm.nih.gov/10888847/]
- 18. - Bcl proteins in 2 development and family ... | Oncotarget breast cancer [https://www.oncotarget.com/article/2792/text/]
- 19. gene: MedlinePlus Genetics TP 53 [https://medlineplus.gov/genetics/gene/tp53/]
- 20. Molecular alterations in anti- apoptotic proteins in BCL ... 2 family breast [https://pubmed.ncbi.nlm.nih.gov/36100115/]
- 21. Studies of apoptosis in breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1120573/]
- 22. Role of Apoptosis and its Modulation by Bcl - 2 ... | SpringerLink Family [https://link.springer.com/chapter/10.1007/978-1-59259-223-4_19]
- 23. Role of p53 Gene in Breast : Focus on Mutation Spectrum and... Cancer [https://pubmed.ncbi.nlm.nih.gov/30255744/]
- 24. Expression of full-length p53 and its isoform Δp53 in breast ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/1476-4598-5-47]
- 25. between Crosstalk -associated fibroblasts and regulated cell... cancer [https://pubmed.ncbi.nlm.nih.gov/38649701/]
- 26. Targeting the redox-programmed cell death axis in breast cancer: from molecular mechanisms to therapeutic resistance | Cell Death Discovery [https://www.nature.com/articles/s41420-025-02743-y]
- 27. Programmed cell death in triple-negative breast | Cellular... cancer [https://cmbl.biomedcentral.com/articles/10.1186/s11658-025-00789-5]
- 28. Cuproptosis, ferroptosis and PANoptosis in tumor immune microenvironment remodeling and immunotherapy: culprits or new hope | Molecular Cancer | Full Text [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02130-8]
- 29. Ferroptosis and pyroptosis are connected through autophagy: a new perspective of overcoming drug resistance | Molecular Cancer | Full Text [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02217-2]
- 30. Role of the Crosstalk between Autophagy and Apoptosis in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3687500/]
- 31. Frontiers | The Double-Edge Sword of Autophagy in Cancer: From Tumor Suppression to Pro-tumor Activity [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.578418/full]
- 32. Targeting ferroptosis in breast | Biomarker Research | Full Text cancer [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-020-00230-3]
- 33. A snapshot into the transcriptomic landscape of apoptosis and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11137012/]
- 34. Autophagy and Apoptotic Crosstalk: Mechanism of Therapeutic Resistance in HER2-Positive Breast Cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/26997868/]
- 35. HER 2: Biology, Detection, and Clinical Implications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3242418/]
- 36. HER2 - Wikipedia [https://en.wikipedia.org/wiki/HER2]
- 37. Regulation of Apoptosis by HER in 2 Breast Cancer [https://pubmed.ncbi.nlm.nih.gov/27088047/]
- 38. Apoptotic Resistance of Metastatic Tumor Cells in Triple Negative Breast Cancer: Roles of Death Receptor-5 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7021605/]
- 39. TP53 Mutation- Specific of Store-Operated Calcium... Dysregulation [https://pubmed.ncbi.nlm.nih.gov/40427112/]
- 40. Tp53 Mutation- Specific of Store-Operated... :: SSRN Dysregulation [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5071905]
- 41. lncRNA GAS5-promoted apoptosis in triple-negative breast cancer by targeting miR-378a-5p/SUFU signaling - PubMed [https://pubmed.ncbi.nlm.nih.gov/31692053/]
- 42. 3 antibody (25128-1-AP) | Proteintech Cleaved Caspase [https://www.ptglab.com/products/cleaved-Caspase-3-Antibody-25128-1-AP.htm]
- 43. -3 (Asp175) Antibody... | Cell Signaling Technology Cleaved Caspase [https://www.cellsignal.com/products/primary-antibodies/cleaved-caspase-3-asp175-antibody/9661]
- 44. targeted sequencing NGS | Paragon Genomics TP 53 panel [https://www.paragongenomics.com/when-the-guardian-loses-function/]
- 45. TP53 apoptosis biomarkers in breast cancer - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0009898125005571]
- 46. Biochemical Analysis of Apoptosis to Impact of Bacterial Extracellular Polymeric Substances Extract on Human Breast Cancer Cell Line (MCF-7) [https://www.sgo-iasgo.com/article/biochemical-analysis-of-apoptosis-to-impact-of-bacterial-extracellular-polymeric-substances-extract-on-human-breast-cancer-cell-line-mcf-7]
- 47. The Clinical Utility of Droplet Digital PCR for Profiling Circulating Tumor DNA in Breast Cancer Patients - PubMed [https://pubmed.ncbi.nlm.nih.gov/36553049/]
- 48. in Serum Circulating Cell-Free Tumor DNA As... TP 53 Mutations [https://pmc.ncbi.nlm.nih.gov/articles/PMC7175353/]
- 49. ERIC recommendations for TP analysis in chronic... 53 mutation [https://www.nature.com/articles/s41375-024-02267-x?error=cookies_not_supported&code=6706cedb-7ea5-433a-9c67-4fd9ac42f13a]
- 50. -inducing proteins with reduced expression in Apoptosis ... breast cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC11848494/]
- 51. Frontiers | Prognostic significance of circulating tumor DNA detection and quantification in cervical cancer: a systematic review and meta-analysis [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1566750/full]
- 52. Liquid biopsy – a narrative review with an update on current US governmental clinical trials targeting immunotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 53. - A pivotal test to help navigate clinical decisions at... Liquid biopsy [https://pubmed.ncbi.nlm.nih.gov/40919127/]
- 54. : current technology and clinical applications | Journal of... Liquid biopsy [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-022-01351-y]
- 55. A deep-learning model for quantifying circulating tumour DNA from the density distribution of DNA-fragment lengths - PubMed [https://pubmed.ncbi.nlm.nih.gov/40055581/]
- 56. Liquid Biopsy Approaches for Cancer Characterization, Residual Disease Detection, and Therapy Monitoring - PubMed [https://pubmed.ncbi.nlm.nih.gov/40305739/]
- 57. Interactions of multidomain pro - apoptotic and... | Oncotarget [https://www.oncotarget.com/article/28031/text/]
- 58. Frontiers | Research progress on natural plant metabolites targeting... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1624569/full]
- 59. Dual Inhibitor Overcomes Gemcitabine Resistance in TNBC [https://bioengineer.org/dual-inhibitor-overcomes-gemcitabine-resistance-in-tnbc/]
- 60. Frontiers | Synergistic antiproliferative and pro-apoptotic effects of Prunus armeniaca and bee venom on breast cancer cells [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1647710/full]
- 61. A guide to automated apoptosis detection: How to make sense of imaging flow cytometry data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5955558/]
- 62. A quantitative real-time approach for discriminating apoptosis and necrosis | Cell Death Discovery [https://www.nature.com/articles/cddiscovery2016101]
- 63. Naringenin impairs mitochondrial function via ROS to induce ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11967926/]
- 64. Promoting Apoptosis, a Promising Way to Treat Breast Cancer With Natural Products: A Comprehensive Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8836889/]
- 65. Recent advances in reactive oxygen species (ROS)-responsive drug delivery systems for photodynamic therapy of cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11725102/]
- 66. ROS-activated anticancer prodrugs: a new strategy for tumor-specific damage - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3566582/]
- 67. Frontiers | Mechanisms of ROS - induced -dependent... mitochondria [https://www.frontiersin.org/journals/marine-science/articles/10.3389/fmars.2024.1499109/full]
- 68. -mediated activation and ROS translocation of CaMKII... mitochondrial [https://jeccr.biomedcentral.com/articles/10.1186/s13046-019-1201-4]
- 69. Isoalantolactone induces in human apoptosis cells via... breast cancer [https://link.springer.com/article/10.1007/s12272-016-0815-8]
- 70. Treatment Strategies: Promising... Breast Cancer Targeted [https://pubmed.ncbi.nlm.nih.gov/31642415/]
- 71. Frontiers | Nanotechnology in cancer treatment: revolutionizing... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1548588/full]
- 72. Targeted apoptosis in breast cells via niosome-mediated... cancer [https://link.springer.com/article/10.1007/s11033-025-10241-8]
- 73. Kinetic quantification of apoptosis [https://www.news-medical.net/whitepaper/20251027/Kinetic-quantification-of-apoptosis-using-Incucytec2ae-live-cell-imaging-assays.aspx]
- 74. Apoptosis - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/sites/books/NBK499821/]
- 75. Frontiers | Low-dose statins restore innate immune response in breast ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1492305/full]
- 76. and SNPs as prognostic and predictive factors in... TP 53 mutations [https://www.spandidos-publications.com/ol/16/1/34]
- 77. p53 protein patterns associated with expression in... TP 53 mutations [https://pmc.ncbi.nlm.nih.gov/articles/PMC11230957/]
- 78. of Mechanisms - PMC Apoptosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC1885741/]
- 79. Oxidative Stress and Redox : Common Mechanisms in... Imbalance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988017/]
- 80. Interplay of oxidative stress and antioxidant mechanisms in cancer ... [https://link.springer.com/article/10.1007/s00204-025-04146-5]
- 81. Mechanisms of Chemotherapy Resistance in Triple-Negative Breast Cancer—How We Can Rise to the Challenge - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6770896/]
- 82. Apoptosis and Molecular Targeting Therapy in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4075070/]
- 83. cDTL contributes to breast cancer progression through regulating redox homeostasis via affecting the function of system xc - PubMed [https://pubmed.ncbi.nlm.nih.gov/39706052/?fc=None&ff=20241221220035&v=2.18.0.post9+e462414]
- 84. Drug uptake-based chemoresistance in breast cancer treatment - PubMed [https://pubmed.ncbi.nlm.nih.gov/32272110/]
- 85. Frontiers | Epigenetic modifications in breast : from immune... cancer [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1584087/full]
- 86. Breast Cancer and Tumor Microenvironment: The Crucial Role of Immune Cells | MDPI [https://www.mdpi.com/1718-7729/32/3/143]
- 87. Cellular Epigenetic Targets and Epidrugs in Breast Cancer Therapy: Mechanisms, Challenges, and Future Perspectives [https://www.mdpi.com/1424-8247/18/2/207]
- 88. Epigenetic Regulation in Breast Cancer: Insights on Epidrugs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9953240/]
- 89. Recent progress in immune evasion mechanisms of triple-negative... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07370-w]
- 90. Frontiers | Editorial: Advances in tumor microenvironment, immunology and immunotherapy of breast cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1664563/full]
- 91. and Tumor Implications in Microenvironment ... Epigenetic Breast [https://link.springer.com/chapter/10.1007/978-3-031-66686-5_2]
- 92. mechanisms in Epigenetic ... | Nature Communications breast cancer [https://www.nature.com/articles/s41467-021-22024-3?error=cookies_not_supported&code=0691297e-3268-4989-a8e3-9ee5e0ff0057]
- 93. in Apoptosis : from pathogenesis to treatment | Journal of... cancer [https://jeccr.biomedcentral.com/articles/10.1186/1756-9966-30-87]
- 94. TRAIL combinations : The new ‘trail’ for cancer (Review) therapy [https://www.spandidos-publications.com/10.3892/ol.2014.1922]
- 95. Potent pro- apoptotic is highly effective in... combination therapy [https://www.nature.com/articles/s41418-021-00869-x?error=cookies_not_supported]
- 96. Co-treatment With HIV Protease Inhibitor Nelfinavir Greatly Increases... [https://pubmed.ncbi.nlm.nih.gov/31262902/]
- 97. Apoptosis | Abcam [https://www.abcam.com/en-us/technical-resources/guides/cell-health-guide/apoptosis]
- 98. Apoptosis: A Comprehensive Overview of Signaling Pathways, Morphological Changes, and Physiological Significance and Therapeutic Implications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11592877/]
- 99. Understanding Apoptosis and Apoptotic Pathways Targeted Cancer Therapeutics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6664112/]
- 100. Prognostic Potential of Apoptosis-Related Biomarker Expression in Triple-Negative Breast Cancers [https://www.mdpi.com/1422-0067/26/15/7227]
- 101. - Caspase and caspase-8 expression in 3 : breast - cancer is... caspase 3 [https://pubmed.ncbi.nlm.nih.gov/27798717/]
- 102. Caspase-3 and caspase-8 expression in breast cancer: caspase-3 is associated with survival - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5306438/]
- 103. - Caspase over-expression is associated with poor... | Oncotarget 3 [https://www.oncotarget.com/article/23667/text/]
- 104. Prognostic value of inhibitors of apoptosis proteins (IAPs) and... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-015-1839-z]
- 105. Novel Apoptosis - Inducing for the Treatment of Cancer... Agents [https://pmc.ncbi.nlm.nih.gov/articles/PMC6721450/]
- 106. Cell Death: Mechanisms and Potential Targets in Breast Cancer Therapy [https://www.mdpi.com/1422-0067/25/17/9703]
- 107. Molecular regulation of apoptotic machinery and lipid... | Oncotarget [https://www.oncotarget.com/article/11490/text/]
- 108. Research on the synergistic effect of a novel apoptosis ... inducer [https://archrazi.areeo.ac.ir/article_132293.html]
- 109. Potential therapeutic GSK-3β inhibitor 9-ING-41 is active in... [https://pubmed.ncbi.nlm.nih.gov/41220107/]
- 110. Induction of apoptosis in cells | Abcam [https://www.abcam.com/en-us/technical-resources/protocols/induce-apopotosis]
- 111. Combinatorial therapy regimens targeting preclinical models of melanoma resistant to immune checkpoint blockade [https://www.ovid.com/journals/jcin/fulltext/10.1172/jci185220~combinatorial-therapy-regimens-targeting-preclinical-models]
- 112. Preclinical efficacy of combinatorial B7-H3 CAR T cells and ONC206 against diffuse intrinsic pontine glioma | Sciety [https://sciety.org/articles/activity/10.1101/2025.09.01.673023]
- 113. Therapeutic advances and application of PARP inhibitors in breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12142329/]
- 114. Frontiers | The role of BCL - 2 family proteins in regulating apoptosis ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.985363/full]
- 115. Calcium-Sensing Receptor Antagonist NPS-2143 Inhibits Breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9106957/]
- 116. of Biomarkers | British Journal of Cancer apoptosis [https://www.nature.com/articles/6604519?error=cookies_not_supported&code=752f6e57-960f-4b2f-ae8d-c56ae34033ef]
- 117. Expression of microRNAs ‘let-7d and miR-195’ and apoptotic genes... [https://www.researchsquare.com/article/rs-2850226/v1]
- 118. antagonizing transcription factor expression and its... Apoptosis [https://pubmed.ncbi.nlm.nih.gov/39911629/]
- 119. Triple negative breast : approved treatment options and their... cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC10314854/]
- 120. Prognostic Significance and Molecular Classification of Triple Negative Breast Cancer: A Systematic Review - European Journal of Breast Health [https://eurjbreasthealth.com/articles/prognostic-significance-and-molecular-classification-of-triple-negative-breast-cancer-a-systematic-review/ejbh.galenos.2025.2024-10-2]
- 121. Targeting apoptosis in cancer therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8211386/]
- 122. Regulation of Apoptosis by HER2 in Breast Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4830426/]
- 123. Frontiers | Immunotherapy resistance in triple-negative breast cancer: Molecular mechanisms, tumor microenvironment, and therapeutic implications [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1630464/full]
- 124. of DNA Repair and Related Biomarkers : Significance of... Pathways [https://pubmed.ncbi.nlm.nih.gov/29604922/]
- 125. The prognosis comparison of different molecular subtypes of breast tum [https://www.dovepress.com/the-prognosis-comparison-of-different-molecular-subtypes-of-breast-tum-peer-reviewed-fulltext-article-CMAR]
- 126. Management of advanced-stage HER2+ breast cancer: current evidence and future perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12327481/]
- 127. Recent advances in the bench - to - bedside of translation ... cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC11873642/]
- 128. Nanomedicine in Cancer Therapeutics: Current Perspectives from... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02368-w]
- 129. From Bench : Lessons Learned in to Preclinical... Bedside Translating [https://pmc.ncbi.nlm.nih.gov/articles/PMC3787906/]
- 130. Better translation from bench to bedside: breakthroughs in the individualized treatment of cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/19104222/]
- 131. - Bench - to of podophyllotoxin-based... bedside translation [https://www.oaepublish.com/articles/microstructures.2025.71]
- 132. Targeting kinases that regulate programmed cell death: a new therapeutic strategy for breast cancer | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06367-9]
- 133. Frontiers | Targeting the inhibitors of apoptosis proteins... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1562167/full]
- 134. Smac mimetics as novel promising modulators of apoptosis in the... [https://pubmed.ncbi.nlm.nih.gov/30506843/]
- 135. Icariin inhibits autophagy and promotes apoptosis by regulating... [https://pubmed.ncbi.nlm.nih.gov/41242617/]
- 136. Treatment in Germany Stage | BookingHealth 4 Breast Cancer 2025 [https://bookinghealth.com/blog/diagnoses-and-treatment/diagnosis-and-treatment/688280-treatment-of-stage-4-breast-cancer-in-germany.html]
- 137. Current Status of Immune Checkpoint Inhibitors and Treatment Responsive Biomarkers for Triple-Negative Breast Cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/40324951/]
- 138. Integration of machine learning and experimental validation to identify the prognostic signature related to diverse programmed cell deaths in breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11744720/]