Beyond PBS: Optimizing K+ and Na+ Levels for Physiologically Relevant Intracellular Mimicry in Biomedical Research
This article provides a comprehensive guide for researchers and drug development professionals on replicating the intracellular ionic environment in vitro.
Beyond PBS: Optimizing K+ and Na+ Levels for Physiologically Relevant Intracellular Mimicry in Biomedical Research
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on replicating the intracellular ionic environment in vitro. It explores the scientific foundation of intracellular potassium and sodium dynamics, details practical methodologies for creating cytomimetic buffers, addresses common challenges and optimization strategies, and presents validation techniques to bridge the gap between biochemical and cellular assay results. By focusing on the critical Na+/K+ ratio, this resource aims to enhance the predictive power and physiological relevance of in vitro studies, ultimately accelerating robust drug discovery.
The Scientific Basis of Intracellular Ion Homeostasis: Why K+ and Na+ Balance Matters
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions
Q1: Why are my experimental results inconsistent when I use a standard phosphate buffer to mimic the intracellular environment?
A: Standard phosphate buffers, often prepared at constant molarity, have a significant flaw: their ionic strength varies with pH. This can lead to unpredictable enzyme activity and inconsistent research results. For instance, studies on cathepsin L show its measured pH optimum appears higher in acetate-MES-Tris buffers of constant ionic strength compared to phosphate buffers of constant molarity. At physiological ionic strengths, the specific buffer ions present directly affect enzymatic activity. For reliable intracellular mimicry, use buffers that maintain a constant ionic strength across your desired pH range [1].
Q2: My cellular assay shows signs of fatigue or reduced function over time. Could ionic shifts be the cause?
A: Yes. Repetitive cellular activity, such as muscle contraction, leads to significant ionic shifts. Research on mouse soleus muscle shows that after stimulation, the intracellular potassium concentration ([K+]i) can decrease by 32 mM, while the interstitial potassium ([K+]inter) doubles. Simultaneously, intracellular sodium ([Na+]i) increases. This imbalance, where the potassium loss is three times greater than the sodium gain, is a key factor in metabolic fatigue. The recovery of these gradients happens slowly, with potassium reaccumulating at a rate of about 20 mM/min post-stimulation [2]. Ensure your experimental system accounts for and can replenish these ion losses.
Q3: How does inhibiting the sodium-potassium pump affect my experiment involving ion-dependent processes?
A: Inhibiting the Na+/K+ ATPase has profound and cascading effects. Direct inhibition by compounds like ouabain causes:
- Immediate ion gradient collapse: Intracellular Na+ builds up as K+ is lost from the cell [3].
- Disruption of secondary transport: The Na+ gradient is necessary for importing glucose and amino acids via symporters. Its collapse halts this nutrient uptake [4].
- Altered calcium signaling: The buildup of intracellular Na+ hinders the Na+/Ca2+ exchanger (NCX), leading to increased intracellular Ca2+ levels, which affects processes from muscle contractility to neuronal signaling [3] [4].
- Cell swelling: The failure of ionic osmoregulation can cause cells to swell and potentially lyse [4].
Q4: What is the fundamental difference between the intracellular and extracellular ionic milieus?
A: The environments are maintained in a state of non-equilibrium by the constant activity of the Na+/K+ pump [4]. The core differences are summarized in the table below.
| Parameter | Intracellular Milieu | Extracellular Milieu |
|---|---|---|
| Sodium (Na+) Concentration | Low (5-15 mM) [4] [5] | High (135-145 mM) [4] |
| Potassium (K+) Concentration | High (100-140 mM) [4] [5] | Low (3.5-5 mM) [4] |
| Primary Positive Charge | K+ | Na+ |
| Na+/K+ ATPase Role | Maintains gradient, consumes ATP [3] [4] | N/A |
| Net Electrical Charge | Negatively charged (relative to outside) | Positively charged (relative to inside) |
Troubleshooting Common Experimental Issues
Issue: Unexpectedly Low Enzyme Activity in Cell Lysate Assays
- Step 1: Understand the Problem
- Check if the enzyme's known pH and ionic strength optims align with your buffer system. The problem may not be the enzyme itself, but the milieu you've provided.
- Step 2: Isolate the Issue
- Change one thing at a time: Test your enzyme's activity in a buffer with constant ionic strength (e.g., acetate-MES-Tris) versus a constant molarity buffer (e.g., phosphate). Compare the results [1].
- Compare to a working model: Repeat the assay using a well-established, physiologically relevant medium like Hanks' Balanced Salt Solution (HBSS) as a benchmark for performance [1].
- Step 3: Find a Fix
- Solution: Switch to a buffer system that maintains a constant ionic strength. Document the specific buffer and ionic conditions used to ensure future reproducibility.
Issue: Poor Reproducibility in Studies of Neuronal Computation or Synaptic Plasticity
- Step 1: Understand the Problem
- Recognize that standard neuronal models often assume constant intracellular Na+ concentration. However, [Na+]i is dynamic and can act as a "memory" of past activity, influencing neuronal computation over longer time scales [5].
- Step 2: Isolate the Issue
- Dig deeper: Consider if your experimental protocol involves repeated stimulation, bursting, or extensive synaptic input. These conditions lead to Na+ loading that is not quickly reversed [5].
- Step 3: Find a Fix
- Workaround: Account for the slow dynamics of [Na+]i in your experimental design and data interpretation. Be aware of its effects on the sodium Nernst potential (reducing EPSP amplitude), Na+/K+ pump activity (causing hyperpolarization), and Na+/Ca2+ exchange (prolonging calcium elevation) [5].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Ion Mimicry Research |
|---|---|
| Ouabain/Digoxin | Specific inhibitors of the Na+/K+ ATPase. Used to study the effects of collapsed Na+/K+ gradients and for probing pump-related signaling pathways [3] [4]. |
| Ion-Selective Microelectrodes | Tools for directly measuring the intracellular chemical activities (free concentrations) of Na+ and K+, providing more accurate data than total content measurements [6]. |
| Hanks' Balanced Salt Solution (HBSS) | A model of the extracellular fluid with a defined ionic composition and physiological ionic strength. Useful for benchmarking enzyme activity or cellular function in a physiologically relevant medium [1]. |
| Acetate-MES-Tris Buffer System | A buffer that can be prepared to maintain a constant ionic strength across a range of pH values, avoiding the pitfalls of phosphate buffers and providing more consistent conditions for intracellular mimicry [1]. |
| Na+/K+ ATPase (from tissue extracts) | The key enzyme for establishing and maintaining the K+ and Na+ gradients. Used in reconstitution experiments and functional studies of ion transport [3] [4]. |
Experimental Protocols & Data Presentation
Protocol: Measuring Ion Gradient Recovery After Cellular Stimulation
This protocol is adapted from studies on muscle tissue [2] and can be modified for other cell types.
- Cell Preparation: Culture or prepare your target cells (e.g., skeletal muscle myotubes, neurons) on appropriate substrates.
- Baseline Measurement: Use ion-selective microelectrodes or fluorescent dyes to measure the resting concentrations of intracellular K+ ([K+]i) and Na+ ([Na+]i).
- Stimulation Phase: Apply a defined repetitive stimulus. For muscle cells, this could be electrical field stimulation to induce contraction (e.g., 960 pulses). For neurons, use a depolarizing current or synaptic activation protocol.
- Immediate Post-Stimulation Measurement: Rapidly measure [K+]i, [Na+]i, and interstitial K+ ([K+]inter) if possible, immediately after the stimulation ends.
- Recovery Phase Monitoring: Continue to measure ion concentrations at regular intervals (e.g., every 30 seconds for 5-10 minutes) under resting conditions to track the recovery of the gradients.
- Data Analysis: Plot the time course of [K+]i increase and [Na+]i decrease. The recovery rate can be quantified, for example, as mM of K+ reaccumulated per minute [2].
Quantitative Data on Ionic Shifts During Activity
The following table summarizes key data from in vitro muscle contraction studies, illustrating the magnitude of ionic changes researchers might encounter [2].
| Measurement | Soleus Muscle at Rest | Soleus Muscle Post-Stimulation (960 pulses) | Change |
|---|---|---|---|
| Intracellular K+ ([K+]i) | 168 mM | 136 mM | -32 mM |
| Intracellular Na+ ([Na+]i) | 12.7 mM | 23.3 mM | +10.6 mM |
| Resting Membrane Potential (RMP) | -69.8 mV | -57.9 mV | -11.9 mV |
| K+ Reuptake Rate (initial) | N/A | 20.4 mM/min | N/A |
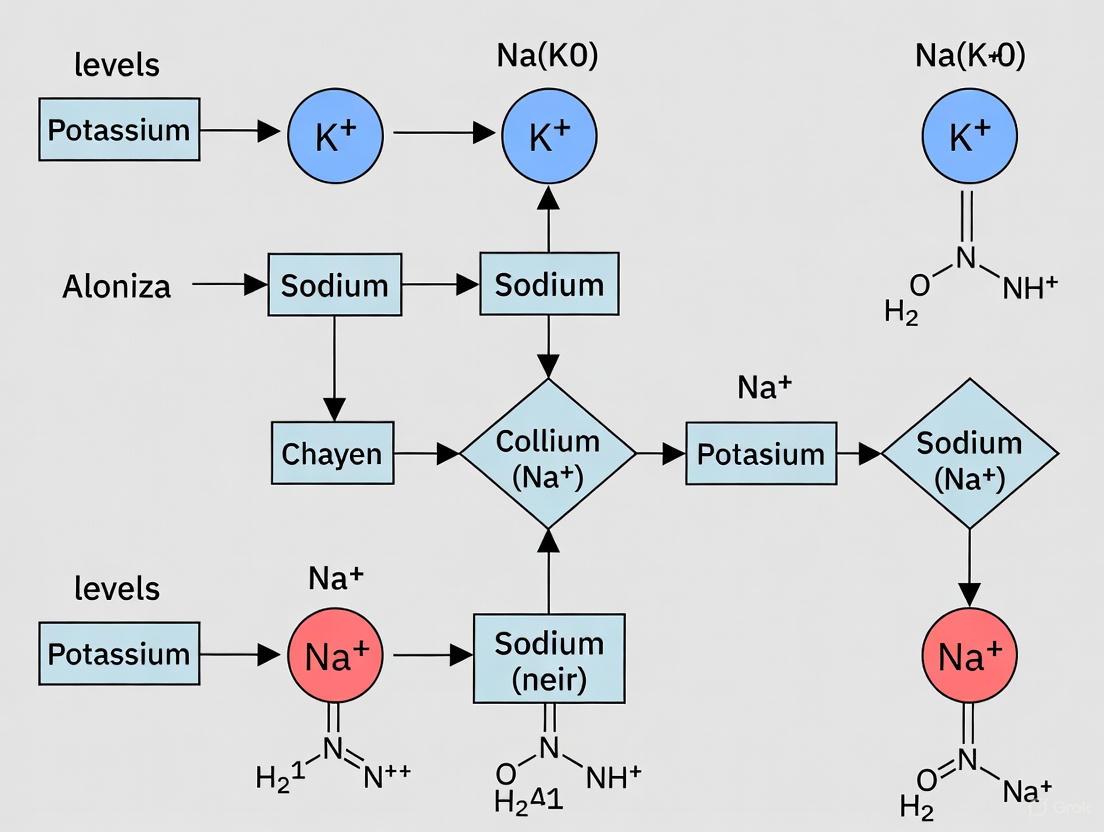
Signaling Pathways and Experimental Workflows
Diagram 1: Ion Shift & Fatigue Recovery Cycle
Diagram 2: Na+/K+ ATPase Ion Transport Mechanism
Frequently Asked Questions (FAQs)
Q1: What are the fundamental roles of sodium and potassium in generating the resting membrane potential?
The resting membrane potential is primarily established and maintained by the sodium-potassium pump (Na+/K+-ATPase) and the differential permeability of the membrane to these ions [7] [8].
- The Sodium-Potassium Pump: This pump is an electrogenic P-type ATPase that actively transports 3 Na+ ions out of the cell and 2 K+ ions into the cell for every ATP molecule hydrolyzed [9]. This action creates a concentration gradient for each ion and directly contributes a net negative charge inside the cell [7] [9].
- Ion Gradients: The pump maintains a high intracellular K+ concentration (approximately 140-180 mM) and a low intracellular Na+ concentration (approximately 12-15 mM), while the extracellular fluid has high sodium and low potassium [7] [2] [10].
- Membrane Potential: The combined effect of the ionic concentration gradients and the selective movement of K+ out of the cell through leak channels results in the interior of the cell being electrically negative relative to the exterior, typically around -70 mV in many cells [8] [9].
Q2: Why is the Na+/K+-ATPase so critical for more than just ion balance?
The Na+/K+-ATPase is a cornerstone of cellular energetics because its function extends far beyond simple ion homeostasis. Its activity is foundational for several critical processes [7] [11] [9]:
- Energetic Cost: It is a major consumer of cellular energy, accounting for up to 30% of a cell's total ATP expenditure in many cells and even more in highly active nerve and muscle cells [9].
- Driver for Secondary Active Transport: The steep sodium gradient created by the pump provides the energy to power the symport of essential nutrients like glucose and amino acids into the cell [7] [8].
- Regulation of Cell Volume: By managing intracellular solute levels, the pump helps prevent osmotic swelling and maintains cell volume [9].
- Electrical Signaling: The ionic gradients are essential for the generation and propagation of action potentials in neurons and muscle cells [8] [10].
Q3: My experimental cells show signs of stress or death during electrophysiological recording. Could this be related to K+/Na+ imbalance?
Yes, disruption of K+ and Na+ homeostasis is a common cause of cell stress and failure in experimental settings. Key factors and symptoms to investigate include [2] [10]:
- ATP Depletion: The Na+/K+-ATPase requires a constant supply of ATP. If your experimental conditions compromise cellular metabolism (e.g., inhibition of ATP production), the pump will fail, ionic gradients will collapse, and cells will swell and lyse [7] [9].
- Pump Inhibition: Certain drugs, like cardiac glycosides (e.g., digoxin), directly inhibit the Na+/K+-ATPase and can be used experimentally but will lead to a loss of ion gradients [9].
- Symptom - Cell Swelling: This indicates a failure to expel Na+ and regulate osmotic pressure [9].
- Symptom - Loss of Excitability: In neurons or muscle cells, an inability to fire action potentials suggests a dissipated Na+/K+ gradient [10].
- Symptom - Depolarization: A decay of the resting membrane potential towards zero is a direct sign of collapsing ion gradients [11].
Q4: How do shifts in intracellular K+ and Na+ concentrations during cellular activity, like muscle contraction, affect my experimental readings?
During high activity, such as repeated muscle contraction or neuronal firing, significant ion shifts occur that experimenters must account for [2]:
- Ion Fluxes: Intracellular K+ can decrease significantly (e.g., by 32-48 mM in muscle), while intracellular Na+ increases (e.g., by ~10 mM) [2]. The interstitial K+ concentration can double [2].
- Membrane Potential: These shifts cause a measurable depolarization of the resting membrane potential (e.g., decreases of 12-18 mV) [2].
- Recovery Time: Post-activity, the membrane potential and ion gradients recover with a time constant on the order of minutes (e.g., 0.9-1.5 minutes), driven by the Na+/K+-ATPase [2].
- Experimental Impact: These changes can alter cellular excitability, signal propagation, and the interpretation of electrophysiological data if not considered. It is crucial to allow adequate recovery time between stimulations.
Troubleshooting Guides
Problem 1: Rapid Depletion of ATP in Cell Culture
Potential Cause: Overactive ion pumping due to leaky membranes or constant electrical activity. Solution:
- Verify Reagent Purity: Check for contaminants in your media that might create non-specific membrane pores.
- Optimize Stimulation Protocol: If stimulating cells electrically, ensure the frequency and duration are not pushing cells into an unsustainable metabolic state. Refer to the ion flux data in Table 1 for expected changes.
- Supplement Energy Substrates: Ensure the culture media contains adequate glucose and other metabolic precursors to support ATP production.
- Monitor Intracellular Ions: If possible, use ion-sensitive fluorescent probes to track Na+ and K+ in real-time to confirm homeostasis.
Problem 2: Inconsistent Action Potential Measurements
Potential Cause: Unstable resting membrane potential due to inadequate ion gradient maintenance. Solution:
- Check Pipette Solutions: For patch-clamp experiments, ensure your intracellular (pipette) solution has the correct K+ concentration (e.g., ~140 mM) and low Na+ to mimic the physiological cytoplasm [2] [10].
- Confirm Bath Solution: Verify that your extracellular solution has high Na+ (e.g., ~145 mM) and low K+ (3.6-5.5 mM) [10].
- Allow for Equilibrium: After establishing a whole-cell configuration, allow sufficient time (several minutes) for the cell and pipette solutions to equilibrate and for the Na+/K+ pump to establish a stable baseline.
- Include ATP: Add Mg-ATP (e.g., 2-5 mM) to your pipette solution to power the Na+/K+-ATPase during recordings directly.
Problem 3: Inconsistent Results in Secondary Transport Assays
Potential Cause: A weakened Na+ gradient is failing to drive symport or antiport processes effectively. Solution:
- Prime the Gradient: Ensure cells are pre-incubated in a Na+-rich, nutrient-free buffer to build a strong outward Na+ gradient before initiating the transport assay.
- Inhibit the Pump Cautiously: Using a low dose of ouabain can help you test if your transport process is sensitive to the Na+ gradient. Observe if transport decreases upon partial pump inhibition.
- Control Temperature: Perform assays at a consistent, physiological temperature (37°C), as pump activity is temperature-sensitive.
Quantitative Data Reference
Table 1: Normal and Critical Physiological Concentrations of K+ and Na+ [2] [10]
| Ion / Parameter | Compartment | Normal Range | Critical / Activity-Altered Level | Key Functional Role |
|---|---|---|---|---|
| Sodium (Na+) | Extracellular Fluid | 135 - 145 mmol/L | > 160 mmol/L (Severe Hypernatremia) | Osmotic balance; Action potential initiation |
| Intracellular Fluid | ~12.7 mM (Resting) | Can increase by ~10 mM during activity [2] | Substrate for Na+/K+ ATPase; Gradient energy | |
| Potassium (K+) | Extracellular Fluid | 3.6 - 5.5 mmol/L | > 6.5 mmol/L (Severe Hyperkalemia) | Resting membrane potential |
| Intracellular Fluid | ~168-182 mM (Resting) | Can decrease by 32-48 mM during activity [2] | Main intracellular cation; Osmotic regulator |
Table 2: Sodium-Potassium Pump Operational Specifications [7] [8] [9]
| Characteristic | Specification | Experimental Implication |
|---|---|---|
| Stoichiometry | 3 Na+ out : 2 K+ in | Creates an electrogenic outward current [9]. |
| Energy Source | Hydrolysis of 1 ATP per cycle | Highly sensitive to metabolic inhibitors and hypoxia [7]. |
| ATP Consumption | Up to 30% of total cellular ATP | A major metabolic cost, especially in excitable cells [9]. |
| Primary Function | Maintains Na+ and K+ concentration gradients | Establishes the resting membrane potential [8]. |
| Impact on Membrane Potential | Directly contributes -5 to -10 mV | Must be considered in voltage calculations [11]. |
Experimental Protocols for Intracellular Mimicry
Protocol 1: Quantifying Na+/K+ ATPase-Dependent ATP Consumption
Objective: To measure the fraction of cellular ATP dedicated to maintaining K+ and Na+ gradients. Materials:
- Cell culture or cell line of interest
- ATP bioluminescence assay kit
- Ouabain (Na+/K+ ATPase inhibitor)
- Control buffer (e.g., Ringer's solution)
- Luminometer or plate reader
Methodology:
- Cell Preparation: Plate cells in a multi-well plate and grow to 80% confluency.
- Equilibration: Replace media with a balanced salt solution and equilibrate for 1 hour.
- Inhibition: Treat test wells with a defined concentration of ouabain (e.g., 1 mM). Leave control wells untreated.
- ATP Extraction: At timed intervals (e.g., 0, 15, 30, 60 minutes), lyse cells and quantify ATP levels using the bioluminescence assay according to the kit's instructions.
- Calculation: The difference in ATP depletion rate between ouabain-treated and control cells represents the ATP consumption dedicated to Na+/K+ pumping.
Protocol 2: Measuring Activity-Dependent Ion Shifts Using Ion-Selective Microelectrodes
Objective: To directly monitor changes in intracellular K+ and Na+ activities during stimulated cellular activity [6] [2]. Materials:
- Ion-selective microelectrodes for K+ and Na+
- Conventional microelectrode for membrane potential recording
- Tissue preparation or single-cell system (e.g., isolated muscle fiber)
- Stimulation apparatus
- High-impedance amplifier and data acquisition system
Methodology:
- Electrode Preparation and Calibration: Fabricate and calibrate ion-selective microelectrodes in standard solutions of known K+ and Na+ concentration [6].
- Impalement: Impale a single cell with both the ion-selective electrode and the conventional potential-sensing electrode.
- Baseline Recording: Record the resting membrane potential and the baseline intracellular ion activities [2].
- Stimulation: Apply a defined repetitive stimulation protocol (e.g., 960 stimuli at a specific frequency) [2].
- Data Collection: Continuously record the changes in membrane potential and ion activities during and after the stimulation period until recovery to baseline.
- Analysis: Correlate the magnitude of ion shifts (e.g., decrease in [K+]i, increase in [Na+]i) with the degree of membrane depolarization and the time course of recovery [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for K+ and Na+ Homeostasis Research
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| Ouabain (or other cardiac glycosides) | Specific inhibitor of the Na+/K+-ATPase [9]. | Used to dissect the pump's contribution to membrane potential and ATP consumption. |
| Ionophore (e.g., Gramicidin, Monensin) | Creates ion-specific pores in the membrane, allowing ions to flow down their gradients. | Used to deliberately collapse ion gradients for control experiments. |
| Ion-Sensitive Fluorescent Dyes (e.g., SBFI-AM for Na+, PBFI-AM for K+) | Ratiometric dyes that change fluorescence upon binding specific ions. | For live-cell imaging and real-time tracking of intracellular ion concentrations. |
| ATP Bioluminescence Assay Kit | Precisely measures ATP concentration in cell lysates via a luminescent reaction. | For quantifying the metabolic cost of ion pumping (see Protocol 1). |
| Defined Ionic Bath & Pipette Solutions | Artificial extracellular and intracellular solutions with precisely controlled ion concentrations [10]. | Essential for electrophysiology experiments to establish and control the ionic environment. |
Signaling and Metabolic Pathway Visualizations
Sodium-Potassium Pump Cycle
Ion Homeostasis Experimental Workflow
FAQs: Core Concepts and Troubleshooting
Q1: What is the fundamental electrogenic function of the Na+/K+-ATPase?
The Na+/K+-ATPase is electrogenic because it transports ions against their concentration gradients in an unequal ratio. For every molecule of ATP hydrolyzed, the pump exports three sodium ions (Na+) from the cell and imports two potassium ions (K+). This results in a net export of one positive charge per cycle, which directly contributes to the negative resting membrane potential of the cell [4] [3] [12].
Q2: My cell volume assays are showing swelling. Could this be related to Na+/K+-ATPase function?
Yes, directly. A primary function of the pump is cell volume regulation. Cells contain numerous organic metabolites that create an osmotic drive for water influx. The Na+/K+-ATPase continuously expels sodium ions to counteract this, maintaining osmotic equilibrium. If the pump fails or is inhibited, the resulting increase in intracellular solute concentration leads to water influx and cell swelling, which can progress to cell lysis [4] [12].
Q3: Why is the Na+/K+-ATPase considered a signal transducer, not just a pump?
Beyond ion transport, the Na+/K+-ATPase acts as a sophisticated signaling receptor. When it binds cardiac glycosides like ouabain, it can initiate intracellular signaling cascades without necessarily inhibiting pumping activity (especially at low, nanomolar concentrations). The pump interacts with proteins like Src kinase to form a signaling complex that can activate key pathways, including MAPK/ERK and PI3K, influencing cell growth, proliferation, and differentiation [4] [12].
Q4: I'm observing altered neuronal firing patterns in my experiments. How might the Na+/K+-ATPase be involved?
Recent research shows the pump is a key information processing element in the brain, not just a housekeeping molecule. In neurons like cerebellar Purkinje cells, the pump's activity, which depends on intracellular Na+ concentration (itself a record of recent firing activity), can dictate whether a neuron is tonic, bursting, or quiescent. It can generate afterhyperpolarizations (AHPs) that act as a form of short-term memory, influencing the timing and duration of subsequent firing [13].
Q5: My research involves neurodevelopmental disorders. Are there therapeutic targets related to this pump?
Indirectly, yes. While the Na+/K+-ATPase itself is a target in cardiology, its function is closely linked to chloride transporters that determine neuronal chloride concentration. The NKCC1 importer and KCC2 exporter set the intracellular [Cl-], which dictates whether GABAergic transmission is inhibitory or excitatory. Altered NKCC1/KCC2 ratios are observed in disorders like Down syndrome and autism. Selective NKCC1 inhibitors (e.g., ARN23746) are in preclinical development to restore healthy chloride levels and correct excitatory/inhibitory imbalances in the brain [14] [15].
Table 1: Key Functional Metrics of the Na+/K+-ATPase
| Parameter | Value | Experimental Context / Significance |
|---|---|---|
| Transport Stoichiometry | 3 Na+ out : 2 K+ in | Fundamental electrogenic property; net export of one positive charge per cycle [4] [3] |
| Energy Consumption in Neurons | Up to 70-75% of ATP | In nerve cells and gray matter, highlighting its massive metabolic cost [4] [3] |
| Typical Intracellular [Na+] | 5-15 mM | Gradient maintained by the pump against a high extracellular [Na+] (135-145 mM) [4] |
| Typical Intracellular [K+] | 100-140 mM | Gradient maintained by the pump against a low extracellular [K+] (3.5-5 mM) [4] |
| IC50 of ARN23746 for NKCC1 | ~11.1 μM (in neurons) | Potency of the NKCC1 inhibitor in a physiological neuronal Ca2+-influx assay [15] |
Table 2: Endogenous and Exogenous Modulators of Na+/K+-ATPase
| Modulator | Type | Effect and Mechanism |
|---|---|---|
| Ouabain/Digoxin | Exogenous (pharmacological) | Cardiac glycosides that inhibit pump function by binding to the K+ site, leading to increased intracellular Ca2+ and cardiac contractility [4] [3] |
| Endogenous Ouabain | Endogenous (hormone) | Mammalian-derived hormone that binds the pump to trigger Src kinase signaling pathways, acting as a signal transducer [12] |
| cAMP | Endogenous (second messenger) | Upregulates the Na+/K+-ATPase. Ligands of Gs-coupled GPCRs increase cAMP and thus pump activity [4] |
| 5-InsP7 | Endogenous (signaling molecule) | Negatively regulates the pump by driving its endocytosis and degradation [4] |
| Thyroid Hormone (T3) | Endogenous (hormone) | Increases the synthesis of Na+/K+-ATPase, raising the basal metabolic rate [4] [3] |
| Intracellular Ca2+ | Endaneous (ion) | Can either stimulate or inhibit pump activity depending on cell type and presence of regulatory proteins like calmodulin [16] |
Experimental Protocols
Protocol 1: Investigating Pump Electrogenicity and its Contribution to Resting Membrane Potential
This protocol allows for the dissection of the pump's direct electrical contribution to the membrane potential.
- Cell Preparation: Use a standard patch-clamp setup on your target cell type (e.g., neuron, HEK293 cell).
- Baseline Recording: In current-clamp mode, record the stable resting membrane potential.
- Pump Inhibition: Apply a specific Na+/K+-ATPase inhibitor (e.g., 100 µM Ouabain) to the extracellular solution. Observe the depolarization (shift to a more positive potential) of the membrane. This depolarization represents the combined effect of running down the Na+ and K+ concentration gradients and the loss of the pump's hyperpolarizing electrogenic current.
- Ionic Gradient Dissociation (Optional): To isolate the pure electrogenic contribution, perform an experiment in voltage-clamp mode. Block all major voltage-gated and ligand-gated ion channels. Apply a rapid pulse of K+ to the extracellular solution to activate the pump. The resulting outward current is the direct electrogenic pump current [13].
Protocol 2: Activating and Measuring Na+/K+-ATPase-Mediated Intracellular Signaling
This protocol outlines how to probe the signal transduction function of the pump independent of its ion-pumping activity.
- Cell Stimulation: Treat cells with low, nanomolar concentrations (1-10 nM) of Ouabain. These concentrations are often sufficient to activate signaling cascades without causing significant inhibition of ion transport or cell death.
- Pathway Activation: Allow a short incubation period (e.g., 5-30 minutes).
- Signal Detection:
- Protein Phosphorylation: Lyse the cells and perform a Western blot analysis on the extracted proteins. Probe for phosphorylated (active) forms of key signaling proteins such as ERK1/2 (MAPK pathway) and Src kinase (Tyr-416 phosphorylation) [4] [12].
- Immunoprecipitation: To confirm direct protein-protein interactions, immunoprecipitate the Na+/K+-ATPase α-subunit and probe for co-precipitated Src kinase [4].
- Downstream Effects: Assess functional downstream outcomes such as changes in gene expression (via RT-qPCR), cell proliferation (via MTT assay), or cell adhesion.
Signaling Pathway Visualization
NKA Signal Transduction Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying Na+/K+-ATPase Function
| Reagent / Material | Function in Research | Key Considerations |
|---|---|---|
| Ouabain Octahydrate | A specific, high-affinity inhibitor of the Na+/K+-ATPase. Used to inhibit ion-pumping function and to activate pump-mediated signal transduction at low concentrations. | Use micromolar concentrations for full pump inhibition; nanomolar concentrations may selectively activate signaling. Cell-type specificity of isoforms should be considered [4] [12]. |
| Digoxin / Digitoxin | Cardiac glycosides used to study pump inhibition in a cardiac physiology context, leading to increased intracellular Ca2+ and positive inotropy. | These compounds have a narrower therapeutic index and different pharmacokinetics compared to ouabain [3]. |
| ARN23746 | A selective, brain-penetrant inhibitor of the NKCC1 chloride importer. Used in neurodevelopmental disorder research to restore GABAergic inhibition. | Not a direct pump inhibitor, but targets a transporter critically dependent on the Na+ gradient established by the Na+/K+-ATPase [14] [15]. |
| HEK293 Cells | A common mammalian cell line used for heterologous expression and functional characterization of Na+/K+-ATPase isoforms and associated mutants. | Easily transfectable; allows for controlled overexpression and purification of the pump protein [15]. |
| Primary Neuronal Cultures | Essential for studying the physiological role of the pump and its signaling in electrically excitable cells, including its effect on firing patterns and synaptic transmission. | Reveals cell-type-specific functions, such as the role in setting intrinsic activity modes in Purkinje neurons [13]. |
| Patch-Clamp Electrophysiology Setup | The gold-standard technique for measuring the electrogenic properties of the pump (pump current) and its effect on membrane potential and neuronal excitability. | Allows for real-time, dynamic assessment of pump function in living cells under voltage- or current-clamp [13] [17]. |
| Phospho-Specific Antibodies (e.g., p-ERK, p-Src) | Critical tools for detecting the activation of signaling pathways downstream of the Na+/K+-ATPase signalosome, typically via Western blot. | Confirms the receptor-like function of the pump independent of its ion-pumping activity [4] [12]. |
Technical Support Center
Troubleshooting Guides
FAQ 1: How can ionic imbalance disrupt my cellular assay results?
Ionic imbalances, particularly of K+ and Na+, can significantly skew experimental outcomes by affecting cellular viability, enzyme kinetics, and signal transduction pathways.
- Underlying Cause: The primary mechanism involves the disruption of transmembrane electrochemical gradients essential for maintaining cellular homeostasis. This affects Na+/K+ ATPase activity, membrane potential, and cellular volume.
- Manifestation in Assays: You may observe increased oxidative stress markers, impaired ATPase function, and abnormal cellular responses in your data.
- Solution:
- Validate Ionic Conditions: Prior to main experiments, conduct a dose-response using your buffer system to establish a non-toxic, homeostatic range for K+ and Na+ concentrations.
- Monitor Key Biomarkers: Incorporate assays for oxidative stress (e.g., malondialdehyde for lipid peroxidation) and ionic balance (e.g., Na+/K+ ATPase activity) as part of your standard protocol to detect subtle imbalances.
- Use Physiological Standards: Ensure your control groups use ionic concentrations that mimic the intracellular or extracellular environment relevant to your research model. Reference values can be found in the table below.
FAQ 2: What are the key experimental readouts for confirming K+ and Na+ imbalance in a cell model?
Key quantitative and observational readouts can confirm a state of ionic imbalance.
- Direct Measurement:
- Intracellular Ion Concentrations: Use ion-sensitive fluorescent dyes (e.g., SBFI for Na+, PBFI for K+) or ion-selective microelectrodes for direct quantification.
- ATPase Activity Assay: Measure the activity of Na+/K+ ATPase, a key regulator of ionic balance. A significant decrease in activity is a strong indicator of disruption.
- Downstream Consequences:
- Oxidative Stress Markers: Quantify markers like hydrogen peroxide, malondialdehyde (MDA), and protein carbonyl content. Elevations indicate pro-oxidant-antioxidant imbalance often triggered by ionic stress [18] [19].
- Metabolic Profile: Analyze shifts in metabolic intermediates, such as fatty acid composition, which have been linked to Co²⁺-induced disruption of Na+K+ and Mg²+ ATPases [18].
- Morphological Assessment: For tissue or primary cell models, histopathological examination (e.g., of gill structures in fish models) can reveal structural damage caused by ionic imbalance [18] [19].
Data Presentation
Table 1: Quantitative Shifts in Intracellular Ions and Metabolites Under Ionic Stress
| Model System | Induced Imbalance | Change in [K+]i | Change in [Na+]i | Change in ATPase Activity | Key Metabolic Shift |
|---|---|---|---|---|---|
| Mouse Soleus Muscle | In vitro repetitive stimulation [2] | Decrease by 32 mM | Increase by 10.6 mM | Data not provided | N/A |
| Common Carp Gill | Co²⁺ exposure (45.37 µg/L, 72h) [18] | Indirect evidence of disruption | Indirect evidence of disruption | Significant inhibition | Significant shift in fatty acid profile [18] |
| Human Erythrocytes | Altered extracellular K+ [20] | Controlled variable | Increase from 8.29 to 9.19 mEq/L | Ouabain-insensitive pathway affected | N/A |
Table 2: Normal and Critical Electrolyte Ranges for Experimental Reference
| Electrolyte | Normal Serum Range | Critical Imbalance Levels | Primary Physiological Function |
|---|---|---|---|
| Sodium | 135-145 mmol/L [10] | Hyponatremia: <135 mmol/L [10] | Controls extracellular fluid volume, nerve impulse transmission [21] |
| Potassium | 3.6-5.5 mmol/L [10] | Hypokalemia: <3.6 mmol/L [10] | Regulates heart rhythm, nerve and muscle function [21] |
Experimental Protocols
Detailed Methodology: Quantifying Ionic Imbalance-Induced Oxidative Stress and ATPase Inhibition in Tissue Homogenates
This protocol is adapted from studies on cobalt toxicity in common carp, focusing on measurable endpoints of ionic imbalance [18].
Key Reagents and Equipment:
- Tissue homogenizer
- Spectrophotometer or microplate reader
- Centrifuge
- Phosphate Buffered Saline (PBS), pH 7.4
- Thiobarbituric Acid (TBA) for Malondialdehyde (MDA) assay
- Reagents for ATPase activity (ATP, Mg²⁺, Na⁺, K⁺ in buffered solution)
- Commercial Ferric Reducing Antioxidant Power (FRAP) assay kit
Step-by-Step Procedure:
Sample Preparation:
- Sacrifice the model organism according to ethical guidelines.
- Dissect and rapidly excise the target tissue (e.g., gill, muscle). Rinse in ice-cold PBS to remove blood/contaminants.
- Homogenize 100 mg of tissue in 1 mL of ice-cold PBS. Centrifuge the homogenate at 3,000 x g for 10 minutes at 4°C.
- Collect the clear supernatant for subsequent assays.
Lipid Peroxidation Assay (Malondialdehyde - MDA):
- Mix 0.5 mL of tissue supernatant with 1 mL of TBA reagent.
- Incubate the mixture in a boiling water bath for 15 minutes.
- Allow it to cool and measure the absorbance at 532 nm.
- Calculate MDA concentration using its molar extinction coefficient and express as nmol MDA per mg protein [18].
Antioxidant Capacity Assay (FRAP):
- Follow the instructions provided with the commercial FRAP assay kit.
- Briefly, mix the sample with the FRAP working reagent and incubate.
- Measure the absorbance at 593 nm. Quantify antioxidant power against a standard curve of Ferrous Sulphate [18].
Na+/K+ ATPase Activity Assay:
- Prepare an assay mixture containing ATP, Mg²⁺, Na⁺, and K⁺ in a suitable buffer.
- Split the mixture into two aliquots. Add ouabain (a specific Na+/K+ ATPase inhibitor) to one aliquot.
- Add the tissue supernatant to both tubes and incubate at 37°C for 30 minutes.
- Stop the reaction and measure the inorganic phosphate (Pi) released.
- Na+/K+ ATPase activity is calculated as the difference in Pi released between the ouabain-free and ouabain-treated tubes, expressed as µmol Pi per mg protein per hour [18].
Mandatory Visualization
Diagram: Ionic Imbalance Disruption Pathway
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Ionic Imbalance Research
| Reagent / Material | Function in Experiment | Specific Example of Use |
|---|---|---|
| Ouabain (G-Strophanthin) | Specific inhibitor of Na+/K+ ATPase activity. | Used to isolate and quantify the contribution of Na+/K+ ATPase to total ATP hydrolysis in enzyme activity assays [18] [20]. |
| Ionophores (e.g., Valinomycin for K+) | Facilitates the passive transport of specific ions across cell membranes. | Used to experimentally manipulate intracellular ion concentrations and study the effects on membrane potential and cell signaling. |
| Ion-Selective Microelectrodes | Directly measures the activity of specific ions (e.g., K+, Na+) in intracellular or extracellular spaces. | Enabled precise measurement of [K+]i and [Na+]i shifts during muscle contraction in mouse soleus and EDL muscles [2]. |
| Thiobarbituric Acid (TBA) | Reacts with malondialdehyde (MDA), a byproduct of lipid peroxidation, to form a colored adduct. | Key reagent for quantifying oxidative stress in tissue homogenates, such as in gill tissue of cobalt-exposed fish [18]. |
| Potassium Chloride (KCl) | Used to adjust extracellular K+ concentration and study its effects on ion transport and cellular function. | In erythrocyte studies, used to demonstrate how extracellular K+ influences ouabain-insensitive 22Na+ uptake and intracellular sodium pools [20]. |
Building a Better Buffer: A Practical Guide to Cytomimetic Formulation
Key Concentration Ranges for Intracellular Mimicry
For research aimed at replicating the intracellular environment, targeting physiologically accurate ion concentrations is fundamental. The tables below summarize the target and disturbed concentration ranges for potassium and sodium ions, which are crucial for setting up controlled experimental conditions.
Table 1: Target and Pathological Intracellular K+ Concentrations
| Condition | Approximate [K+]i | Physiological Context |
|---|---|---|
| Healthy Resting Neuron | ~150 mM [22] | Baseline for most experimental controls. |
| During Seizure-like Activity | Decreases | Large-scale decrease resolvable by genetically encoded sensors [22]. |
| During Peri-Infarct Depolarizations | Decreases | Indicates a significant pathological shift [22]. |
Table 2: Target and Pathological Intracellular Na+ Concentrations
| Condition | Approximate [Na+]i | Physiological Context |
|---|---|---|
| Healthy Resting State | Low (Concentration gradient ~10x higher outside) [23] | Maintained by the Na+/K+ ATPase pump; creates a strong electrochemical driving force. |
| Prolonged Spiking (Model) | Increases by several mM [24] | Slow accumulation over seconds of activity; reduces action potential amplitude. |
| Lidocaine Exposure (Model) | Increases | Mediated through Na+-H+ exchanger activation [25]. |
Troubleshooting Guides
FAQ 1: Why can't I detect changes in intracellular K+ during single action potentials?
Issue: Your sensor system may lack the temporal resolution or sensitivity for small, rapid flux events.
Solutions:
- Verify Sensor Capability: The genetically encoded sensor lc-LysM GEPII 1.0, for example, resolves large [K+]i decreases during intense activity but requires optimization to detect the subtler changes from single action potentials [22].
- Check Expression & Targeting: Ensure robust expression of the biosensor in the correct subcellular compartment (e.g., cytosol). Use appropriate promoters (e.g., neuronal hSyn promoter) and confirm sensor localization [22].
- Confirm Experimental Model: Intense, seizure-like or optogenetically evoked activity is more likely to produce a detectable signal with current technologies [22].
FAQ 2: My recordings show an unexplained, slow hyperpolarization after a period of neuronal activity. What could be the cause?
Issue: This is likely an activity-dependent phenomenon linked to ion concentration dynamics and pump activity.
Solutions:
- Investigate Sodium Dynamics: A burst of activity causes [Na+]i to accumulate. This increased [Na+]i stimulates the electrogenic Na+-K+ ATPase pump, which hyperpolarizes the cell by exporting 3 Na+ for every 2 K+ imported [3] [24].
- Confirm with Protocol: This "slow after-hyperpolarization (AHP)" is pronounced immediately after a train of action potentials and slowly decays as pump activity restores baseline [Na+]i [24].
- Model the Effect: Incorporate dynamic ion concentrations and Na+-K+ pump currents into your computational models to predict and confirm this effect [5] [24].
FAQ 3: Why do my neurons show a sudden switch from regular firing to an intermittently interrupted, burst-like pattern during prolonged stimulation?
Issue: This is a characteristic sign that the extracellular ionic environment has been significantly disturbed.
Solutions:
- Measure Extracellular K+: Accumulation of K+ in the restricted extracellular space ([K+]o) during prolonged activity can qualitatively alter neuronal excitability. This can switch the spike-generating mechanism from a regular spiking mode to a bistable, intermittent bursting mode [24].
- Consider Sodium's Role: Concurrent intracellular Na+ accumulation reduces the sodium Nernst potential, which decreases action potential amplitude and contributes to excitability changes [24].
- Review Perfusate Volume: Ensure adequate volume and flow rate of your perfusion system to prevent local ion accumulation in in vitro setups.
Core Experimental Protocols
Protocol: Measuring Intracellular K+ with Genetically Encoded Sensors
This protocol details the use of the FRET-based biosensor lc-LysM GEPII 1.0 to monitor [K+]i in neurons.
Workflow Overview:
Materials:
- Plasmids: lc-LysM GEPII 1.0 cDNA in an AAV backbone (e.g., pAAV-hSyn for neuronal expression) [22].
- Cells/Animals: Primary cultured neurons or suitable animal model (e.g., mouse cortex) [22].
- Key Equipment: Two-photon fluorescence lifetime imaging microscope (2P-FLIM) [22].
Step-by-Step Procedure:
- Sensor Selection and Cloning: Subclone the lc-LysM GEPII 1.0 open reading frame into an AAV vector under a cell-type-specific promoter (e.g., CAG for ubiquitous, hSyn for neuronal, or GFAP for astrocytic expression). Confirm sequence integrity [22].
- Viral Packaging: Package the construct into adeno-associated viral (AAV) particles using a system like AAV-DJ in HEK293T cells. Purify and concentrate the viral particles [22].
- Delivery: Transfert primary cultured neurons or inject the AAV particles stereotaxically into the target brain region of live mice for in vivo expression [22].
- Imaging: Perform 2-photon fluorescence lifetime imaging. Excite the sensor at ~850 nm and collect emission at 450-500 nm. Record the fluorescence lifetime shift, which is inversely correlated with [K+]i [22].
- Data Analysis & Calibration: Analyze fluorescence lifetime changes. For quantification, perform an in vitro calibration by recording the sensor's lifetime in solutions with known K+ concentrations (0-150 mM, with osmolarity balanced by Na+) [22].
Protocol: Tracking Intracellular Na+ Dynamics in Computational Models
Incorporating dynamic [Na+]i is essential for modeling prolonged neuronal activity and its effects on excitability.
Workflow Overview:
Model Components:
- Define the State Variable: Add [Na+]i as a dynamic variable in your multi-compartmental neuronal model (e.g., in the NEURON simulation environment) [5].
- Model Key Fluxes:
- Influx: Calculate Na+ entry through voltage-gated Na+ channels (INa) and glutamatergic synaptic channels. The rate of change is given by:
d[Na+]i/dt = INa / (F * V), where F is Faraday's constant and V is compartment volume [5]. - Efflux: Implement the electrogenic Na+-K+ ATPase pump current (Ipump). This can be modeled as a sigmoidal function of [Na+]i and [K+]o that saturates at high concentrations [26] [24].
- Diffusion: Include longitudinal diffusion of Na+ between adjacent compartments, as Na+ is not buffered like Ca2+ and diffusion is a major factor in its dynamics [5].
- Influx: Calculate Na+ entry through voltage-gated Na+ channels (INa) and glutamatergic synaptic channels. The rate of change is given by:
- Couple to Membrane Potential: Allow the updated [Na+]i to modulate the sodium Nernst potential (ENa) in real-time, which will affect spike amplitude and synaptic drive [5] [24].
- Simulation and Validation: Run simulations with prolonged stimuli (seconds) to observe slow accumulation of [Na+]i and its effects, such as spike amplitude reduction and pump-induced hyperpolarization. Validate model predictions against electrophysiological recordings [24].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Ion Concentration Research
| Reagent/Tool | Function/Application | Key Characteristics |
|---|---|---|
| lc-LysM GEPII 1.0 | Genetically encoded K+ biosensor [22] | FRET-based; usable in vitro and in vivo (2P-FLIM); resolves large [K+]i decreases. |
| Sodium-Binding Benzofuran Isophthalate (SBFI) | Ratiometric, fluorescent Na+ indicator dye [25] | Chemical dye for intracellular sodium imaging. |
| Valinomycin | K+ ionophore [27] | Used experimentally to manipulate K+ gradients across membranes. |
| Ouabain / Digoxin | Na+/K+ ATPase pump inhibitors [3] | Cardiac glycosides; used to study pump function and disrupt ion homeostasis. |
| Furosemide | Cotransporter inhibitor (KCC, NKCC) [28] | Used to investigate the role of chloride cotransporters in [Cl-]i regulation, which is often linked to Na+-dependent transport. |
| Na+-H+ Exchanger Antagonists (e.g., EIPA) | Inhibits Na+-H+ exchange [25] | Used to probe mechanisms of Na+ influx and intracellular pH coupling. |
The biochemical assessment of a ligand's activity, typically expressed as Kd or IC50 values, is conventionally established using purified protein targets in simplified buffer systems like Phosphate-Buffered Saline (PBS) [29]. However, a significant and persistent discrepancy often exists between the activity values obtained from these biochemical assays (BcAs) and subsequent cellular assays (CBAs), even when factors such as compound permeability and stability are accounted for [29]. This inconsistency primarily stems from the fundamental differences between the well-controlled, dilute conditions of standard in vitro assays and the complex, crowded intracellular milieu where these compounds are ultimately intended to function [29].
The eukaryotic cytoplasm is a densely packed environment with macromolecular concentrations ranging between 200 and 300 mg/mL, creating a crowded milieu that profoundly influences molecular interactions, diffusion, and enzymatic kinetics [29] [30]. Standard buffers like PBS, which closely mimic extracellular fluid with high sodium (157 mM) and low potassium (4.5 mM) levels, are physiologically inaccurate for simulating the intracellular environment where this ratio is reversed—potassium concentrations reach ~140-150 mM while sodium levels are approximately 14 mM [29]. Furthermore, PBS fails to replicate other critical cytoplasmic properties, including macromolecular crowding, viscosity, and cosolvent content, all of which can alter dissociation constants (Kd) by up to 20-fold or more compared to standard buffer measurements [29].
Therefore, employing cytomimetic buffers—solutions engineered to mimic the intracellular environment—is crucial for generating biologically relevant data in in vitro experiments, particularly for drug development where most targets reside inside the cell [29]. This technical resource details the key components of these buffers and provides troubleshooting guidance for researchers aiming to bridge the gap between biochemical and cellular assays in intracellular mimicry research, with a specific focus on optimizing potassium and sodium levels.
Core Components of a Cytomimetic Buffer
A effective cytomimetic buffer must replicate the multifaceted physicochemical (PCh) conditions of the cytoplasm. The table below summarizes the four key component categories and their target concentrations for intracellular mimicry.
Table 1: Key Components and Target Concentrations for a Cytomimetic Buffer
| Component Category | Specific Agents | Target Intracellular Concentration/Range | Primary Function |
|---|---|---|---|
| Salt Composition | Potassium (K⁺) | ~140-150 mM | Dominant intracellular cation; maintains membrane potential and osmotic balance [29] |
| Sodium (Na⁺) | ~14 mM | Minor intracellular cation; reverse ratio to extracellular fluid is critical [29] | |
| Macromolecular Crowding Agents | Synthetic Polymers (e.g., PEG, Ficoll) | 200-300 mg/mL total macromolecules | Simulates volume exclusion and altered diffusion; impacts equilibrium constants [29] [30] |
| Physiological Crowders (e.g., protein lysates) | 200-300 mg/mL total macromolecules | Provides more accurate mimicry including electrostatic/hydrophobic interactions [30] | |
| pH Modulators | HEPES, PIPES | Cytosolic pH ~7.2 | Maintains physiological intracellular pH; different from extracellular pH [29] |
| Viscosity & Cosolvent Modulators | Glycerol, Sucrose | Varies to match cytoplasmic viscosity | Modifies solution viscosity and lipophilicity to influence binding kinetics [29] |
Salt Composition: Optimizing K+ and Na+ Levels
The ionic composition is a foundational element of a cytomimetic buffer. The cytoplasm is a potassium-rich environment, a condition that is the inverse of the sodium-dominated extracellular space [29].
- Rationale for High K+/Low Na+: The high intracellular potassium concentration (~140-150 mM) is maintained by the Na+/K+ ATPase pump and is crucial for numerous cellular processes, including enzyme activity, protein synthesis, and maintaining the resting membrane potential [29]. Using a buffer like PBS (Na+: 157 mM, K+: 4.5 mM) for intracellular target studies creates an unphysiological ionic environment that can skew protein-ligand interactions and enzyme kinetics [29].
- Impact on Molecular Interactions: The specific ionic atmosphere, determined by the types and concentrations of ions present, can shield electrostatic interactions between proteins and ligands, thereby affecting the measured binding affinity (Kd). Therefore, replicating the correct K+ to Na+ ratio is not merely about ionic strength but about creating the correct biochemical context [29].
Macromolecular Crowding Agents
Macromolecular crowding is perhaps the most defining yet frequently overlooked characteristic of the intracellular environment.
- Mechanisms of Action: High concentrations of inert macromolecules create a crowded space that reduces the available volume (volume exclusion effect), which can favor compact states of proteins and enhance the association of interacting molecules [29] [30]. This crowding can dramatically alter both equilibrium constants and reaction kinetics.
- Agent Selection: Early studies relied on synthetic polymers like polyethylene glycol (PEG) and Ficoll. While effective at mimicking volume exclusion, they lack the complex interplay of electrostatic and hydrophobic interactions found in cells [30]. A more physiologically accurate approach involves using concentrated cell lysates, which provide a heterogeneous mixture of macromolecules closer to the native state [30]. Experimental data has shown that enzyme kinetics can change by as much as 2000% under appropriate crowding conditions [29].
pH Modulators and Buffering Systems
The cytosolic pH is typically maintained around 7.2, which is distinct from the slightly more alkaline extracellular pH. Using an appropriate buffer system like HEPES or PIPES to maintain this pH at 37°C is critical, as pH can profoundly influence protein charge, structure, and ligand binding [29]. Furthermore, the intracellular environment is more reducing than the extracellular space due to high glutathione levels. While including reducing agents like DTT can mimic this, caution is advised as they may disrupt proteins reliant on disulfide bonds for stability [29].
Additional Modulators: Viscosity and Cosolvents
Beyond crowding, cytoplasmic viscosity and the presence of various cosolvents (e.g., amino acids, sugars) contribute to the overall PCh environment. These factors can be modulated by adding compounds like glycerol or sucrose to match the internal milieu, further fine-tuning the buffer to better reflect in-cell conditions and improve the correlation between BcAs and CBAs [29].
Diagram 1: Core Components of a Cytomimetic Buffer and Their Targets.
Experimental Protocols & Methodologies
Protocol 1: Formulating a Basic Cytomimetic Buffer
This protocol outlines the steps to prepare a liter of a basic cytomimetic buffer for biochemical assays.
Table 2: Formulation of a Basic Cytomimetic Buffer
| Component | Final Concentration | Purpose | Notes |
|---|---|---|---|
| HEPES | 20 mM | pH Buffering | Maintains pH ~7.2 at 37°C [29] |
| Potassium Glutamate | 140 mM | Major Ionic Component | Glutamate is a common intracellular anion [30] |
| Sodium Chloride | 14 mM | Minor Ionic Component | Represents residual intracellular Na+ [29] |
| Magnesium Glutamate | 3-5 mM | Divalent Cation | Critical for ATP-dependent processes and enzyme function [30] |
| PEG 8000 | 100 mg/mL | Crowding Agent | Common synthetic crowder; adjust concentration as needed [30] |
| DTT | 1 mM (Optional) | Redox Environment | Mimics reducing cytoplasm; use with caution [29] |
| Glycerol | 5% v/v (Optional) | Viscosity Modifier | Adjusts solution viscosity [29] |
Preparation Steps:
- Dissolve Components: In approximately 800 mL of purified water, dissolve the HEPES, potassium glutamate, sodium chloride, and magnesium glutamate. Stir until fully dissolved.
- Adjust pH: Using KOH or HCl, adjust the pH of the solution to 7.2 at room temperature. Note that pH can be temperature-dependent.
- Add Crowding Agent: Slowly add the PEG 8000 (or alternative crowding agent) while vigorously stirring to prevent clumping. This may take considerable time to fully dissolve.
- Add Optional Components: If required, add DTT and glycerol. DTT should be added fresh from a stock solution just before use.
- Final Volume: Bring the final volume to 1.0 L with purified water. Sterile filter if necessary (note: high viscosity from crowding agents may make filtration difficult).
- Verification: Confirm the final pH and osmolality. Store at 4°C for short-term use.
Protocol 2: Assessing Buffer Efficacy via Biomolecule Diffusion
This methodology uses Fluorescence Recovery After Photobleaching (FRAP) to validate that the cytomimetic buffer replicates the size-dependent diffusion observed in real cells [30].
Principle: The diffusion coefficient (D) of a molecule is inversely related to the viscosity and macromolecular crowding of its environment. By measuring the D of probes of different sizes (e.g., a small dye, GFP, and ribosomes) in the cytomimetic buffer versus standard buffer, you can quantify how well the buffer mimics cytoplasmic constraints.
Procedure:
- Sample Preparation:
- Incorporate fluorescent probes into the buffer or a liposome-based protocell filled with the cytomimetic buffer [30].
- Probe 1 (Small Molecule): Use NBDG (0.34 kDa) to represent metabolites. Expected D should remain high (>26 μm²/s) even under crowding [30].
- Probe 2 (Medium Protein): Use Green Fluorescent Protein (GFP, 27 kDa). Expected D should decrease significantly with crowding (e.g., from ~35 to ~2 μm²/s) [30].
- Probe 3 (Large Complex): Use labeled 70S ribosomes (2.7 MDa). Expected D should drop dramatically (e.g., from ~0.7 to <0.1 μm²/s), becoming almost immobile at high crowding [30].
- FRAP Measurement:
- Use a confocal microscope to photobleach a defined region of interest (ROI) in the sample.
- Monitor the fluorescence recovery in the bleached area over time.
- Data Analysis:
- Plot the normalized fluorescence intensity in the ROI against time.
- Fit the recovery curve to an appropriate diffusion model to calculate the diffusion coefficient (D) for each probe.
- Compare the D values obtained in the cytomimetic buffer to those in a standard buffer (e.g., PBS) and to literature values from in-cell measurements [30].
Diagram 2: Workflow for Validating Buffer Efficacy via Diffusion.
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: Why does my cytomimetic buffer cause protein precipitation or aggregation? A: This is a common issue when introducing crowding agents. First, ensure your protein is pure and monodisperse in a standard buffer. Then, introduce crowding gradually. The final crowded state may not be at thermodynamic equilibrium, and the crowded environment can accelerate aggregation of marginally stable proteins. Try different types of crowding agents (e.g., switch from PEG to a protein-based crowder like BSA) and ensure that the ionic strength and pH are correctly set, as crowding can exacerbate sensitivity to these conditions [29] [30].
Q2: My biochemical assay kinetics are slower in the cytomimetic buffer. Is this expected? A: Yes, this is a predicted and validated effect. Macromolecular crowding increases the solution viscosity and reduces the diffusion coefficients of enzymes and substrates, particularly larger molecules. This can shift the reaction kinetics from being reaction-rate limited to diffusion-limited. This slowdown is a sign that your buffer is effectively mimicking a key physical property of the cytoplasm. You should compare the kinetics to a standard buffer and in-cell measurements to determine if the slowdown is physiologically relevant [29] [30].
Q3: How critical is the specific choice of anion (e.g., glutamate vs. chloride) in the buffer? A: It can be very significant. The cytoplasm contains a complex mixture of anions, with glutamate and other organic anions being prevalent. Chloride is more characteristic of extracellular fluid. The choice of anion can influence protein stability and activity through specific binding or general ionic atmosphere effects. Using glutamate or a mixture of physiological anions is generally recommended over a chloride-only system for a more accurate cytomimetic buffer [29] [30].
Troubleshooting Guide
Table 3: Troubleshooting Common Issues with Cytomimetic Buffers
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High/Abnormal Assay Background | Crowding agents or other components causing non-specific light scattering or aggregation. | Centrifuge the buffer at high speed before use to remove aggregates. Include proper background controls (e.g., no-substrate, no-enzyme). Verify that the crowding agent is compatible with your detection method. |
| Inconsistent Kd/IC50 Values | Buffer not fully equilibrated; component degradation; inaccurate simulation of a key PCh parameter. | Prepare buffer fresh for critical experiments. Ensure all components are stable and stored correctly. Systematically vary one PCh parameter at a time (e.g., crowding level, K+ concentration) to identify the most influential factor for your target. |
| Poor Correlation with Cellular Data | The buffer may be missing a key intracellular factor (e.g., specific metabolites, correct redox potential). | Consider adding a more complex component, like a dialyzed cell lysate, as a crowder. Re-evaluate the redox potential requirements for your specific protein target, potentially adding or removing reducing agents [29]. |
| High Viscosity Clogging Equipment | Use of high concentrations of large crowding agents (e.g., high MW PEG). | Use lower molecular weight crowding agents (e.g., PEG 4000 vs. PEG 8000) at a higher concentration to achieve similar % weight/volume. Alternatively, use a different type of crowder or dilute the sample just before reading if the assay endpoint allows. |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Resources for Cytomimetic Research
| Reagent/Resource | Function/Description | Example Suppliers / Notes |
|---|---|---|
| Physiological Salt Solutions | Pre-mixed solutions with high K+/low Na+ for intracellular mimicry. | Formulate in-house for control; various chemical suppliers provide high-purity salts (K-glutamate, Mg-glutamate). |
| Macromolecular Crowding Agents | Synthetic (PEG, Ficoll) or physiological (BSA, lysozyme, cell lysates) agents to simulate crowded cytoplasm. | Sigma-Aldrich, Thermo Fisher Scientific. Cell lysates can be prepared in-lab from relevant cell lines (e.g., E. coli, HeLa) [30]. |
| Fluorescent Probes for Validation | Molecules of different sizes (NBDG, GFP, labeled ribosomes) for FRAP-based diffusion measurements. | Thermo Fisher Scientific, Novus Biologicals, Abcam. Ribosomes require purification and labeling [30]. |
| Liposome Preparation Kits | For creating protocells (vesicles) to contain the cytomimetic environment for in-depth validation. | Merck, Avanti Polar Lipids. Microfluidic methods are also highly effective for producing monodisperse liposomes [30]. |
| Cell Lysate-based CFE Systems | Commercial cell-free expression systems that provide a naturally crowded, functionally active cytoplasmic environment. | Thermo Fisher Scientific, Promega, New England Biolabs. Can be used directly or as a base for further buffer optimization [30]. |
Step-by-Step Protocol for Preparing and Validating a Cytomimetic Buffer
This guide provides a detailed protocol for preparing and validating a cytomimetic buffer, a crucial reagent designed to mimic the intracellular ionic environment for in vitro studies. Properly formulated and validated cytomimetic buffers are foundational for research in cell biology, physiology, and drug development, particularly for experiments investigating intracellular signaling pathways, ion channel function, and transporter activity. The following sections offer a step-by-step preparation method, a robust validation framework, and troubleshooting resources to ensure experimental reproducibility and accuracy.
Buffer Composition and Preparation Protocol
Rationale and Target Composition
The cytomimetic buffer is formulated to replicate the key ionic and osmotic conditions found inside a typical mammalian cell. The target composition is based on established physiological concentrations, with potassium (K+) as the primary cation and low sodium (Na+) levels [31] [6] [2]. The buffer also includes essential components to maintain pH, provide energy, and stabilize the cellular milieu.
Table 1: Target Composition of Cytomimetic Buffer
| Component | Final Concentration | Function & Physiological Rationale |
|---|---|---|
| Potassium (K+) | 120 - 150 mM | Primary intracellular cation; crucial for maintaining membrane potential and osmotic balance [6] [2]. |
| Sodium (Na+) | 5 - 15 mM | Maintains low extracellular-like Na+ levels to mimic the intracellular environment accurately. |
| HEPES | 10 - 20 mM | Buffer to maintain physiological intracellular pH. |
| Magnesium ATP | 1 - 5 mM | Energy source for ATP-dependent processes. |
| EGTA | 0.5 - 2 mM | Calcium chelator; controls free Ca2+ concentration. |
| D-Glucose | 5 - 10 mM | Metabolic energy substrate. |
| Osmolarity | 280 - 300 mOsm/kg | Adjusted to match intracellular osmotic pressure. |
Step-by-Step Preparation
Materials Required:
- High-purity deionized water
- Analytical balance
- pH meter
- Osmometer
- Magnetic stirrer and stir bar
- Volumetric flasks and graduated cylinders
- 0.22 µm sterile filter unit
Reagent Solutions:
- Table 2: Research Reagent Solutions
Item Specification Function KCl High Purity (>99%) Source of Potassium Ions NaCl High Purity (>99%) Source of Sodium Ions HEPES Biological Grade pH Buffering Mg-ATP Cell Culture Grade Energy Substrate EGTA Cell Culture Grade Calcium Chelation D-Glucose Anhydrous, High Purity Energy Source
Preparation Procedure:
- Solution Preparation: In a clean beaker, add approximately 800 mL of deionized water. While stirring continuously, dissolve the reagents in the following order to prevent precipitation:
- HEPES powder
- KCl and NaCl
- Mg-ATP
- D-Glucose
- EGTA
- pH Adjustment: Once all components are fully dissolved, slowly adjust the pH of the solution to 7.2 - 7.4 using a concentrated KOH solution. Using KOH prevents the introduction of non-physiological Na+ ions during pH adjustment.
- Final Volume: Transfer the solution to a 1 L volumetric flask and bring the final volume to 1.0 L with deionized water. Mix thoroughly.
- Sterile Filtration: Aseptically filter the buffer through a 0.22 µm sterile filter into a sterile container to remove any particulate matter or microbial contaminants.
- Osmolarity Check: Measure the final osmolarity of the buffer using an osmometer. Adjust if necessary by adding small amounts of deionized water (to decrease) or a neutral osmolyte like sucrose (to increase).
- Aliquoting and Storage: Aliquot the buffer into sterile tubes to avoid repeated freeze-thaw cycles. Store at -20°C for long-term storage. For working solutions, store at 4°C and use within one week.
Diagram 1: Cytomimetic Buffer Preparation Workflow
Buffer Validation Framework
A comprehensive validation strategy ensures the cytomimetic buffer performs as intended and supports reliable experimental outcomes.
Analytical Validation
Table 3: Key Validation Parameters and Methods
| Parameter | Target Specification | Validation Method | Acceptance Criterion |
|---|---|---|---|
| Ion Concentration | [K+] = 120-150 mM[Na+] = 5-15 mM | Ion Chromatography orFlame Photometry | Within ±5% of target |
| Final pH | 7.2 - 7.4 | Calibrated pH Meter | Within ±0.1 unit |
| Osmolarity | 280 - 300 mOsm/kg | Osmometer | Within ±5% of target |
| Sterility | No microbial growth | Sterility Test (e.g.,Culture in LB broth) | No contamination after 72h |
| Functional Performance | Maintains cell/intracellular function | Relevant Bioassay (e.g.,enzyme activity) | Activity >90% of control |
Functional Validation in a Model System
A critical step is to confirm the buffer's functionality in a biological context.
- Recommended Assay: Validate the buffer using an assay that monitors an intracellular process, such as the activity of a potassium-dependent enzyme.
- Protocol:
- Reconstitution: Reconstitute the enzyme in the prepared cytomimetic buffer and a control buffer (e.g., a commercial assay buffer).
- Reaction: Initiate the enzyme-specific reaction according to the manufacturer's protocol.
- Measurement: Measure the reaction rate (e.g., by absorbance or fluorescence) over time.
- Analysis: Compare the enzymatic activity in the cytomimetic buffer to the control. The activity in the cytomimetic buffer should be at least 90% of the control activity to indicate proper functional mimicry.
Diagram 2: Cytomimetic Buffer Validation Protocol
Troubleshooting Guide & FAQs
This section addresses common issues encountered during buffer preparation and use.
Troubleshooting Guide
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Incorrect final pH | HEPES not fully dissolved; inaccurate pH meter calibration. | Ensure all components are dissolved before adjusting pH. Calibrate pH meter with fresh standards before use. |
| Precipitation observed | Components added in incorrect order; Mg-ATP can precipitate with other ions. | Always dissolve components in the specified order. If precipitate forms, warm solution slightly and re-filter. |
| Abnormal bioassay results | Buffer ion concentration is incorrect; buffer is contaminated. | Re-validate ion concentrations via ion chromatography. Prepare a fresh aliquot under sterile conditions. |
| High background in assays | Particulate matter or chemical contaminants in the buffer. | Ensure sterile filtration is performed correctly. Use high-purity water and reagent-grade chemicals. |
| Short shelf-life/instability | Repeated freeze-thaw cycles; chemical degradation (e.g., ATP). | Store in single-use aliquots. Confirm stability of labile components like ATP and consider adding stabilizers. |
Frequently Asked Questions (FAQs)
Q1: Why is it critical to use KOH instead of NaOH for pH adjustment? A: Using KOH maintains the high K+ to Na+ ratio essential for intracellular mimicry. Introducing NaOH would increase the Na+ concentration, altering the fundamental ionic composition and potentially invalidating the buffer's purpose [6].
Q2: How long can the buffer be stored, and what is the optimal storage condition? A: For best results, aliquot the buffer and store it at -20°C for up to 6 months. Avoid repeated freeze-thaw cycles. Once thawed, store the working aliquot at 4°C and use it within one week to maintain stability, particularly for labile components like ATP.
Q3: My experimental results are inconsistent. How can I determine if the buffer is the source of the problem? A: First, re-run the analytical validation tests (pH, osmolarity) on the specific buffer batch in question. If those are correct, perform a side-by-side functional validation assay with a freshly prepared buffer batch and a known commercial control. This will help isolate the buffer as the variable [32].
Q4: Can this buffer be used for permeabilized cell studies? A: Yes, this cytomimetic buffer is well-suited for use with permeabilized cells to study intracellular mechanisms. The buffer provides a controlled ionic environment that mimics the cytoplasm, allowing for the investigation of organelle function and intracellular signaling pathways without the confounding factor of the plasma membrane. Ensure you use an appropriate permeabilization agent compatible with your targets [33] [34].
Frequently Asked Questions (FAQs)
Q1: What is the significance of binding kinetics in drug discovery, and how is it measured?
Binding kinetics, specifically the association (k_on) and dissociation (k_off) rates, determine the time-dependent interaction between a drug and its target. The dissociation rate is often expressed as residence time (RT = 1/k_off), which can impact a drug's efficacy and duration of action in vivo [35] [36]. A longer residence time can allow a target to remain affected even after systemic drug concentrations have declined [35]. Techniques such as isothermal titration calorimetry (ITC) can be used to measure these parameters directly from the heat changes during binding [35]. Alternatively, direct binding assays monitored in real-time (e.g., using FRET or SPR) can generate association curves, from which the observed rate constants are derived [36].
Q2: How can I troubleshoot a ligand-binding assay that is not reaching equilibrium?
Failure to reach equilibrium can lead to inaccurate determination of affinity (K_d). Key steps for troubleshooting include:
- Verify Incubation Time: Perform kinetic experiments to determine the time required for the specific radioligand and receptor preparation to reach steady state. The incubation time in saturation or competition assays must exceed this period [37].
- Check Temperature: Binding reactions are temperature-sensitive. Ensure the assay is conducted at a consistent and appropriate temperature (often 4°C, 25°C, or 37°C), as this will affect kinetic rates [37].
- Avoid Ligand Depletion: If a high fraction of the ligand is bound to the receptor (typically >10%), the free ligand concentration is significantly reduced, distorting the binding curve. This can be corrected by using a lower concentration of receptor protein [37].
Q3: What are the advantages of using Isothermal Titration Calorimetry (ITC) in hit-to-lead optimization?
ITC provides a label-free method to directly measure the thermodynamic profile of a protein-ligand interaction in a single experiment [35]. It yields the binding affinity (K_d), enthalpy change (ΔH), and stoichiometry (n). The enthalpic contribution (ΔH) can be a key indicator for optimization, as forming high-quality interactions (e.g., hydrogen bonds) is often more challenging than improving entropic contributions (often linked to lipophilicity) later in the process [35]. Furthermore, ITC is not susceptible to optical interference from compounds (PAINS), making it a robust method for validating hits [35].
Q4: In High-Throughput Screening (HTS), what is a common method for ensuring data quality? The Z-factor is a widely used statistical parameter for assessing the quality and robustness of an HTS assay. It evaluates the separation between the signal of a positive control and a negative control, while accounting for the variability of both signals. An assay with a Z-factor ≥ 0.5 is considered excellent for HTS purposes, indicating a good dynamic range and low data variation [38].
Troubleshooting Guides
Guide: Poor Signal-to-Noise in Direct Binding Assays
Problem: The specific binding signal is weak and indistinguishable from background noise.
| Possible Cause | Verification Method | Solution |
|---|---|---|
| Low Receptor Concentration | Measure total protein concentration; perform a saturation binding experiment to determine B_max. |
Increase the amount of receptor membrane preparation in the assay, while ensuring ligand depletion does not occur [37]. |
| Low Specific Activity of Radioligand | Check the manufacturer's specification for the radioligand; recalculation of the concentration. | Use a tracer with higher specific activity or increase the concentration of the radioligand within a range that does not cause excessive nonspecific binding [37]. |
| High Nonspecific Binding | Compare total binding with binding in the presence of a high concentration of a cold competitor. | Optimize the composition of the assay buffer (e.g., add cations like Mg²⁺ or detergents); switch the type of filter used for separation [37]. |
| Instability of Reagents | Pre-incubate reagents to check for activity loss over time. | Prepare fresh reagent stocks; add protease inhibitors to the receptor preparation; run the assay at a lower temperature to slow degradation [37]. |
Guide: Inconsistent Results in Enzyme Kinetic Studies
Problem:
High variability in the calculated enzyme inhibition parameters (IC₅₀, K_i) for a test compound.
| Possible Cause | Verification Method | Solution |
|---|---|---|
| Incomplete Equilibrium | Measure reaction rates at different pre-incubation times of the enzyme and inhibitor. | Ensure the enzyme-inhibitor mixture reaches equilibrium before starting the reaction with the substrate. For slow-binding inhibitors, this may require a longer pre-incubation [36]. |
| Unaccounted for Inhibitor Depletion | Measure the free inhibitor concentration after incubation with the enzyme. | Reduce the enzyme concentration in the assay to ensure the free inhibitor concentration is not significantly depleted [37]. |
| Solvent Effects (e.g., DMSO) | Test the enzyme activity across the range of solvent concentrations used in the assay. | Standardize the final concentration of solvent (e.g., DMSO) across all assay wells and keep it as low as possible (typically ≤1%) [38]. |
| Human Error in Liquid Handling | Use a colored dye to check pipetting accuracy and consistency across a microtiter plate. | Implement automated liquid handling systems for greater precision and reproducibility, especially in HTS formats [39] [38]. |
Table 1: Key Kinetic and Thermodynamic Parameters in Drug Discovery
This table summarizes the core parameters used to characterize ligand-target interactions and their significance in drug discovery [35] [36].
| Parameter | Symbol | Unit | Interpretation | Experimental Method |
|---|---|---|---|---|
| Dissociation Constant | K_d |
M (e.g., nM) | Affinity; concentration at which 50% of receptors are occupied. Lower K_d = higher affinity. |
ITC, Saturation Binding [35] [37] |
| Association Rate Constant | k_on |
M⁻¹s⁻¹ | Speed of complex formation. | ITC (kinetic mode), Direct real-time binding assays [35] [36] |
| Dissociation Rate Constant | k_off |
s⁻¹ | Speed of complex breakdown. | ITC (kinetic mode), Direct real-time binding assays [35] [36] |
| Residence Time | RT | s | Average lifetime of the complex; RT = 1/k_off. Longer RT may correlate with prolonged efficacy. |
Calculated from k_off [36] |
| Enthalpy Change | ΔH | kcal/mol | Heat released/absorbed; indicates formation of non-covalent bonds (e.g., H-bonds). | ITC [35] |
| Entropy Change | ΔS | cal/mol·K | Change in disorder; often driven by release of ordered water molecules. | Calculated from K_d and ΔH [35] |
Table 2: HTS Plate Formats and Typical Assay Volumes
The trend in HTS is toward miniaturization to reduce reagent costs and increase throughput [39] [38].
| Microplate Format | Number of Wells | Typical Assay Volume | Primary Use Case |
|---|---|---|---|
| 96-well | 96 | 50 - 200 µL | Low-complexity assays; secondary screening. |
| 384-well | 384 | 5 - 50 µL | Standard for primary HTS campaigns. |
| 1536-well | 1536 | 2 - 10 µL | High-throughput primary screening. |
| 3456-well | 3456 | 1 - 2 µL | Ultra-High-Throughput Screening (uHTS). |
Experimental Protocols
Detailed Protocol: DeterminingK_dandB_maxviaSaturation Binding
Objective: To characterize the affinity of a radiolabeled ligand for its receptor and the density of receptor sites in a preparation.
Materials:
- Receptor preparation (e.g., cell membranes)
- Radioligand (e.g., ³H or ¹²⁵I-labeled) in a stock solution of known concentration and specific activity
- Assay buffer (e.g., phosphate-buffered saline, often requiring optimization of K⁺ and Na⁺ levels for intracellular mimicry)
- Unlabeled ligand (for defining nonspecific binding)
- Microtiter plates and harvesting equipment (e.g., cell harvester with glass fiber filters)
Method:
- Prepare Ligand Dilutions: Create a dilution series of the radioligand, typically spanning a concentration range from ~0.1 ×
K_dto 10 ×K_d. Use at least 10-12 different concentrations. - Set Up Assay Tubes/Wells:
- Total Binding: Receptor + increasing concentrations of radioligand.
- Nonspecific Binding: Receptor + increasing concentrations of radioligand + a high concentration (100 ×
K_d) of unlabeled competitor ligand.
- Initiate Binding: Add a fixed, low concentration of the receptor preparation to all tubes/wells. The total reaction volume is kept constant.
- Incubate: Incubate the mixture at the chosen temperature (e.g., 25°C) for a duration previously confirmed to be sufficient to reach equilibrium (e.g., 60-120 minutes).
- Separate Bound from Free: Rapidly filter the contents under vacuum to trap the receptor-bound radioligand on the filter. Immediately wash the filter with cold buffer to remove unbound ligand.
- Quantify Bound Ligand: Measure the radioactivity on the filters using a scintillation or gamma counter.
- Data Analysis:
- Calculate Specific Binding = Total Binding - Nonspecific Binding.
- Plot Specific Binding (y-axis) against the concentration of free radioligand (x-axis).
- Fit the data to a one-site binding model (hyperbola) using nonlinear regression software to determine
B_max(binding site density) andK_d(equilibrium dissociation constant) [37].
Detailed Protocol: Determining InhibitorK_iviaCompetition Binding
Objective: To determine the affinity (K_i) of an unlabeled test compound for the receptor by its ability to compete with a fixed concentration of radioligand.
Method:
- Prepare Compound Dilutions: Serially dilute the unlabeled test compound over a broad range (e.g., from 10⁻¹² M to 10⁻⁵ M) in assay buffer.
- Set Up Assay: To all tubes/wells, add:
- A fixed concentration of receptor preparation.
- A fixed concentration of radioligand (typically at or below its
K_dvalue). - Increasing concentrations of the test compound.
- Define Controls: Include wells for Total Binding (radioligand + receptor) and Nonspecific Binding (radioligand + receptor + excess unlabeled ligand).
- Incubate and Harvest: Follow steps 4-6 from the Saturation Binding protocol.
- Data Analysis:
- Calculate % Specific Binding = (Binding in test well - Nonspecific Binding) / (Total Binding - Nonspecific Binding) × 100.
- Plot % Specific Binding versus the logarithm of the test compound concentration. Fit the data to a sigmoidal dose-response curve to determine the
IC₅₀(concentration that inhibits 50% of specific binding). - Calculate the inhibition constant
K_iusing the Cheng-Prusoff equation:K_i=IC₅₀/ (1 + [L]/K_d), where [L] is the free concentration of the radioligand andK_dis its dissociation constant [37].
Signaling Pathways and Workflow Diagrams
Diagram 1: Generic ligand binding assay workflow.
Diagram 2: High-throughput screening hit identification process.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Binding & Screening Studies
| Item | Function & Application |
|---|---|
| Microtiter Plates (96 to 1536-well) | The standard labware for HTS and assay development, allowing for miniaturization and parallel processing of samples [39] [38]. |
| Ion-Selective Microelectrodes | Used to directly monitor the chemical activities of specific ions (e.g., K⁺, Na⁺) within the cytoplasm, crucial for research on intracellular mimicry [6]. |
| Radiolabeled Ligands (Tritium, ¹²⁵I) | Provide a highly sensitive and direct method for detecting and quantifying ligand binding to receptors in saturation and competition experiments [37]. |
| Fluorescent/Luminescent Probes | Enable homogeneous, real-time "mix-and-read" assays (e.g., FRET, TR-FRET) ideal for kinetic studies and HTS without separation steps [36] [39]. |
| Isothermal Titration Calorimetry (ITC) | A label-free instrument that directly measures the heat change during binding, providing both thermodynamic (K_d, ΔH, ΔS) and kinetic data in one experiment [35]. |
| Biacore Surface Plasmon Resonance (SPR) | A biosensor-based technology for label-free, real-time analysis of biomolecular interactions, providing detailed kinetic (kon, koff) and affinity (K_d) data [36]. |
Solving the Discrepancy: Troubleshooting Biochemical and Cellular Assay Mismatches
Troubleshooting Guide: Key Questions and Answers
FAQ 1: Why is my measured membrane potential not matching the predicted Nernst potential for potassium, despite correct bulk concentrations?
The Problem: You have calculated the expected potassium equilibrium potential (EK) using the Nernst equation and confirmed your intra- and extracellular K+ solution concentrations, but your experimental measurements consistently deviate.
The Diagnosis: The issue likely lies in the distinction between ionic concentration and ionic activity or is related to incorrect assumptions about membrane permeability [6] [40].
- Ionic Activity vs. Concentration: The Nernst equation depends on ionic activities, not the total chemical concentrations you use to prepare your solutions [6]. A significant portion of intracellular K+ and Na+ may be compartmentalized or otherwise not freely available in the cytoplasm, meaning the effective activity is lower than the total concentration [6].
- Sodium Permeability Influence: The resting membrane potential is a weighted average of the equilibrium potentials for all permeable ions, not just K+. Even at rest, the membrane has a small but non-zero permeability to Na+ (PNa) [40]. The Goldman-Hodgkin-Katz equation more accurately describes this scenario. If your solutions have high sodium or your membrane preparation has a higher-than-expected PNa, it will depolarize the cell (make the potential less negative), pulling it away from EK [40].
The Solution:
- Verify Permeability Assumptions: Use the Goldman-Hodgkin-Katz equation to model your membrane potential, incorporating estimated permeabilities for K+, Na+, and Cl- [41].
- Use Ion-Selective Microelectrodes: Directly measure the intracellular activity of K+ with ion-selective microelectrodes, rather than relying on calculated concentrations [6] [2].
- Pharmacological Blockade: Apply low concentrations of tetrodotoxin (TTX) to block voltage-gated Na+ channels or other specific channel blockers to reduce Na+ permeability and see if the measured potential shifts closer to EK.
FAQ 2: My potassium salt is not dissolving in the artificial intracellular solution at the required concentration. What are my options?
The Problem: You are unable to achieve the desired, often high, concentration of a potassium salt in your buffered solution, preventing accurate ionic mimicry.
The Diagnosis: This is a classic drug development solubility challenge, but it applies directly to creating concentrated ionic research solutions [42] [43]. The intrinsic solubility of the salt form you have chosen is too low for your experimental needs.
The Solution:
- Change the Salt Form: This is the most effective strategy. The choice of counter-anion dramatically influences a salt's aqueous solubility [43]. As shown in Table 1, different potassium salts have vastly different solubilities. Potassium chloride (KCl) is highly soluble and is often the best choice for basic ionic strength adjustments.
- Physical Modifications: For salts with inherently poor solubility, techniques like micronization (reducing particle size to increase surface area) can increase the dissolution rate, though they may not change the equilibrium solubility [42].
- Adjust pH: For salts of weak acids or bases, the solubility is highly dependent on the pH of the solution. Adjusting the pH of your buffer away from the pKa of the ion can enhance solubility [43].
Table 1: Aqueous Solubility of Common Potassium Salts at ~25°C
| Potassium Salt | Chemical Formula | Approximate Solubility (g/100mL) | Notes |
|---|---|---|---|
| Potassium Chloride | KCl | ~34 | High solubility; standard for ionic strength |
| Potassium Acetate | CH3COOK | ~269 | Very high solubility |
| Potassium Bromide | KBr | ~67 | High solubility |
| Potassium Phosphate (monobasic) | KH2PO4 | ~33 | Buffer component; moderate solubility |
| Potassium Sulfate | K2SO4 | ~12 | Lower solubility; can be limiting |
FAQ 3: I am using the correct soluble salt, but my experimental results suggest potassium is not effectively crossing the membrane or impacting the intracellular environment. Why?
The Problem: Even with a soluble potassium salt in the extracellular solution, the expected physiological effect (e.g., membrane depolarization, modulation of transport) is not observed.
The Diagnosis: The permeability of the salt across the membrane is low. Permeability is not solely a property of the K+ ion but is strongly influenced by the lipophilicity of the salt's anion and its ability to form neutral ion-pairs [44].
The Solution:
- Select a Permeable Salt Pairing: The passive diffusion of potassium salts across lipid membranes follows the Hofmeister series. Lipophilic anions (e.g., PF6-, ClO4-) form more neutral ion-pairs with K+, dramatically increasing permeability compared to small, hydrophilic anions like Cl- [44].
- Permeability Ranking (High to Low): KPF6 > KClO4 > KBr > KBF4 > CH3COOK > KCl [44].
- Validate with Direct Measurement: Use ion-selective microelectrodes to directly measure the change in extracellular or (if possible) intracellular K+ activity when applying different salts to confirm the permeability differences [44] [2].
- Consider Active Transport: In living cell systems, remember that the Na+/K+-ATPase pump actively regulates K+ and Na+ levels. Your results may reflect a balance between passive diffusion and active transport [40].
Table 2: Troubleshooting Summary: Permeability vs. Solubility vs. Ionic Environment
| Symptom | Likely Culprit | Diagnostic Experiments | Potential Solutions |
|---|---|---|---|
| Membrane potential deviates from Nernst prediction. | Ionic Environment: Incorrect ionic activities or competing permeabilities (e.g., PNa). | Measure ionic activities with ISMs [6]. Model potential with GHK equation [41]. | Use ion-selective microelectrodes. Apply specific channel blockers. |
| Salt will not dissolve at target concentration. | Solubility: Intrinsic solubility of the chosen salt form is too low. | Check solubility tables for the salt. Test in pure water vs. buffer. | Switch to a more soluble salt (e.g., KCl, KAcetate) [43]. |
| Salt is soluble but shows no biological effect. | Permeability: The anion prevents passive diffusion across the membrane. | Compare effects of different K+ salts from the Hofmeister series [44]. Measure [K+] change with ISMs. | Use a salt with a lipophilic anion (e.g., KPF6). Consider facilitated or active transport pathways. |
| Ionic effects are inconsistent or non-reproducible. | All Three: Complex interaction of factors. | Systematic review of solution recipes, membrane model, and measurement techniques. | Follow the diagnostic workflow below to isolate the key variable. |
Experimental Protocols for Key Diagnostic Experiments
Protocol 1: Measuring Intracellular K+and Na+Activities with Ion-Selective Microelectrodes
This protocol is adapted from methodologies used to directly measure ion activities in muscle fibers and neurons [6] [2].
Principle: Ion-selective microelectrodes contain a liquid ion exchanger in their tip that generates a potential dependent on the activity of a specific ion (e.g., K+), which is different from the potential generated by the membrane itself.
Key Reagents and Functions:
- Potassium Ionophore I Cocktail A: The hydrophobic membrane that selectively binds K+ ions [44].
- Dimethyldichlorosilane: Used to silanize the microelectrode pipette, making the glass hydrophobic to ensure the ionophore forms a stable membrane over the tip [44].
- Backfill Solution (10 mM KCl): Provides a stable internal reference potential for the microelectrode [44].
Methodology:
- Microelectrode Preparation: Pull borosilicate glass capillaries to a fine tip (1-2 µm). Expose the tip to dimethyldichlorosilane vapors to silanize. Front-fill the tip with the potassium ionophore and backfill with 10 mM KCl [44].
- Calibration: Before and after impalement, calibrate the microelectrode in a series of standard KCl solutions (e.g., 1, 10, 100 mM) to generate a voltage vs. log[K+] curve. Only use electrodes with a Nernstian response (~58 mV per decade change in [K+] at 25°C) [44].
- Impalement and Recording: Impale the cell with both the ion-selective microelectrode and a conventional microelectrode (to measure membrane potential). The true intracellular ion activity is derived from the difference in potential between these two electrodes [6] [2].
Protocol 2: Assessing the Impact of Salt Lipophilicity on Passive Permeability
This protocol is based on experiments demonstrating the Hofmeister effect on K+ salt permeability across the blood-brain barrier [44].
Principle: Different potassium salts with anions of varying lipophilicity will passively diffuse across membranes at different rates, which can be quantified by their ability to elevate extracellular K+ and induce excitability.
Key Reagents and Functions:
- Hofmeister Series Salts: KPF6, KClO4, KBr, KBF4, CH3COOK, KCl. These provide a gradient of lipophilicity [44].
- Ion-Selective Microelectrodes: As described in Protocol 1, to directly measure changes in K+ concentration [44].
Methodology:
- Preparation: Set up your experimental system (e.g., in vitro brain preparation, cell culture, artificial membrane).
- Perfusion: Arterially perfuse or bath-apply different K+ salts at a fixed concentration (e.g., 14.2 mM), each for a set duration (e.g., 15 minutes), followed by a washout period with control solution [44].
- Measurement: Simultaneously perform extracellular recordings to monitor changes in tissue excitability (e.g., epileptiform activity) and use K+-sensitive microelectrodes to measure the real-time change in extracellular K+ concentration [44].
- Analysis: Rank the effectiveness of the salts in inducing K+ elevation and physiological effects. The expected order, from most to least effective, follows the Hofmeister series for anion lipophilicity [44].
Diagnostic Workflow and Ion Pathway Visualization
The following diagram illustrates the logical decision-making process for diagnosing issues related to potassium and sodium in intracellular mimicry experiments.
Diagram 1: Diagnostic Pathway for Ionic Experimental Issues
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for K⁺ and Na⁺ Intracellular Mimicry Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Ion-Selective Microelectrodes | Direct measurement of intracellular K+ or Na+ activity [6] [2]. | Requires careful calibration and silanization. Provides data on biologically available ions, not just concentration. |
| Potassium Ionophore I (Cocktail A) | The selective sensor for K+ in ion-selective microelectrodes [44]. | Critical for creating a valid K+-sensitive electrode. |
| Potassium Chloride (KCl) | The standard salt for adjusting ionic strength and K+ concentration due to its high solubility [43]. | Low membrane permeability due to hydrophilic Cl- anion [44]. |
| Hofmeister Series Salts (KPF₆, KClO₄) | Used to study and enhance passive K+ permeability across membranes [44]. | Caution: Salts like KClO₄ can be explosive or hazardous; review safety protocols. |
| Na⁺/K⁺-ATPase Inhibitors (e.g., Ouabain) | Pharmacological tool to block active ion transport, allowing study of passive ion fluxes [40]. | Useful for isolating passive permeability effects from active pump activity. |
| Tetrodotoxin (TTX) | Specific blocker of voltage-gated sodium channels [40]. | Used to reduce sodium permeability (PNa) when diagnosing membrane potential discrepancies. |
| Constant Chemical Potential MD (CμMD) | Advanced simulation algorithm to model solubility and crystal growth/dissolution of organic salts in complex solutions [45]. | Helps predict solubility in solvent mixtures before wet-lab experiments. |
FAQs: Sodium-Potassium Balance in Cellular Research
1. Why is the sodium-potassium (Na+:K+) ratio critical for intracellular mimicry?
The Na+:K+ ratio is fundamental for maintaining the resting membrane potential, cell volume, and proper function of the sodium-potassium pump (Na+/K+-ATPase) [46] [47]. This pump actively transports 3 sodium ions out of the cell for every 2 potassium ions it brings in, creating essential electrochemical gradients [47]. An imbalanced ratio disrupts cellular homeostasis, affecting everything from nerve signal transmission and muscle contraction to the activity of various neurotransmitter receptors, which can compromise the validity of your intracellular mimicry models [46] [47].
2. What is the target dietary Na+:K+ ratio for in vivo studies, and how does it relate to cellular research?
While not a direct recipe for cell culture media, the dietary intake ratio provides insight into physiological balance. Major health authorities suggest aiming for a potassium intake of approximately 4,700 mg per day and a sodium intake of less than 2,300 mg per day [48]. This equates to a Na+:K+ ratio of about 1:2 by weight [48]. This ratio is considered optimal for cardiovascular health and counteracting the effects of high sodium, which is a valuable reference point for establishing physiologically relevant conditions in animal studies that underpin cellular research [49] [48].
3. How can I accurately measure the Na+:K+ ratio in an experimental setting?
The gold standard method is to calculate the ratio from multiple days of 24-hour urine collection [50]. However, this is often impractical. A more feasible approach is to measure the ratio in casual (spot) urine samples. For the most reliable estimate of the 24-hour ratio from a single sample, research suggests collecting a second-morning void (around 9 a.m.) [50]. It is crucial to note that a single casual urine sample has limitations and can sometimes underestimate the true 24-hour ratio [50].
4. What are common symptoms or experimental outcomes of an imbalanced Na+:K+ ratio?
In cellular or animal models, an imbalance may manifest indirectly. Signs can include elevated blood pressure in animal subjects, fluid retention, and disrupted cellular signaling [48] [46]. At a molecular level, imbalance can affect vascular smooth muscle cell proliferation, platelet aggregation, and insulin secretion [46]. In the context of neuronal research, inhibition of the Na+/K+-pump can lead to depolarization of neurons and altered rhythmic activity [47].
Troubleshooting Guides
Problem 1: Inconsistent Results in Cellular Assays
- Potential Cause: Uncontrolled or unmeasured Na+:K+ ratio in your culture media or buffers.
- Solution:
- Standardize Reagents: Use high-purity salts and document the exact concentrations of sodium and potassium in all media and reagent formulations.
- Measure Baseline: Use ion-selective electrodes or flame photometry to verify the actual Na+ and K+ concentrations in your prepared solutions.
- Systematic Variation: Design experiments where the Na+:K+ ratio is the independent variable to establish a dose-response curve for your specific cell type and assay.
Problem 2: Translating In Vitro Findings to In Vivo Models
- Potential Cause: A significant disconnect between the ionic environment of your cell culture system and the physiological conditions in a living organism.
- Solution:
- Reference Physiological Data: Consult literature for measured serum and intracellular Na+ and K+ levels in your target tissue or organism.
- Mirror Physiological Ratios: Adjust your culture conditions to mimic the serum Na+:K+ ratio, which is typically around 28:1 in mmol/L (e.g., ~140 mM Na+ to ~5 mM K+), while recognizing the intracellular ratio is reversed [51].
- Validate with Biomarkers: In animal studies, correlate your experimental ratio with established biomarkers, such as the urine Na/K ratio, which is recommended to be 2 or lower [50].
Key Quantitative Data for Experimental Design
The following tables summarize critical quantitative data for planning your experiments.
Table 1: Recommended Dietary & Physiological Ratios for In Vivo Context
| Context | Recommended Sodium | Recommended Potassium | Target Ratio (Na+:K+) | Basis |
|---|---|---|---|---|
| Dietary Intake (Human) | < 2,300 mg/day | 4,700 mg/day | ~1:2 (by weight) | Public health guidelines for chronic disease risk reduction [48] |
| Urine Excretion (Biomarker) | N/A | N/A | 2 (molar ratio) | Japanese Society of Hypertension consensus target for healthy individuals [50] |
| Serum (Molar Ratio) | ~137-142 mmol/L | ~3.8-5.0 mmol/L | ~28:1 to 35:1 | Standard clinical laboratory reference ranges |
Table 2: Experimental Na+:K+ Ratio Impact in Model Systems
| Model System | Ratio / Concentration Context | Observed Effect |
|---|---|---|
| Locusta Malpighian Tubule Cells | Incubation in Rb-Ringer (K+ replacement) | Cellular K+ dramatically fell; K+-rich urine secretion continued despite low intracellular [K+], suggesting complex regulatory mechanisms [52]. |
| Mammalian & Invertebrate Neurons | Inhibition of Na+/K+-ATPase with Ouabain/Strophanthidin | Depolarization of the resting membrane potential by ~3-8 mV, and disruption of rhythmic (bursting) activity [47]. |
| (KxNa1-x)NbO3 Ceramics (Materials Science) | Extreme K/Na ratios (e.g., 45/55) | Significant enhancement of piezoelectric properties (e.g., energy storage, converse piezoelectric response), demonstrating the profound functional impact of cation stoichiometry [53] [54]. |
Essential Experimental Protocols
Protocol 1: Measuring the Urine Na/K Ratio as a Biomarker
This protocol is adapted from methods discussed in hypertension research for use in animal studies or clinical trials [50].
- Sample Collection: Collect urine samples from subjects. For the most accurate reflection of the 24-hour ratio, collect the second-morning void (around 9 a.m.) over at least 4 non-consecutive days. Pool samples if using a multi-day average.
- Storage: Freeze samples at -20°C or below until analysis to prevent degradation.
- Analysis: Measure sodium and potassium concentrations (in mmol/L) using standard clinical chemical analyzers or ion-selective electrodes.
- Calculation: Calculate the Na/K ratio for each sample using the formula:
Urine Na/K Ratio = [Na+] (mmol/L) / [K+] (mmol/L) - Interpretation: Average the ratios from multiple collections. A ratio of 2 or lower is considered an optimal target in some physiological contexts [50].
Protocol 2: Modifying Ionic Environment in Cell Culture
This protocol outlines a method for systematically studying the effects of Na+:K+ ratio in vitro.
- Prepare Basal Media: Start with a custom basal culture medium lacking sodium and potassium chloride.
- Add Salts: Supplement with NaCl and KCl to achieve the desired final concentrations and Na+:K+ ratio. Maintain a constant osmolarity and chloride concentration across all conditions to isolate the effects of the cation ratio.
- Ion-Specific Buffers: For acute experiments, consider using ion-specific buffers to clamp extracellular K+ concentrations while varying Na+, or vice versa.
- Validate: Confirm final ion concentrations in the media using an ion analyzer or flame photometer before applying to cells.
- Assay Endpoints: Measure functional endpoints relevant to your research, such as membrane potential changes (using fluorescent dyes), expression of ion transporters, intracellular calcium signaling, or cell viability/proliferation.
Signaling Pathways & Experimental Workflows
Sodium-Potassium Homeostasis & Cellular Impact
Experimental Workflow for Ratio Optimization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Na+/K+ Ratio Research
| Reagent / Material | Function in Research | Example Use Case |
|---|---|---|
| Ouabain (G-Strophanthin) | Specific, high-affinity inhibitor of the Na+/K+-ATPase pump [47]. | Used to experimentally block the sodium-potassium pump to study its role in maintaining membrane potential and cellular homeostasis in neuronal or muscle preparations [47]. |
| Ion-Selective Electrodes | Measure the activity of specific ions (Na+, K+) in solutions. | Verifying the exact concentration of ions in custom-prepared cell culture media, artificial cerebrospinal fluid (aCSF), or biological fluids like urine [50]. |
| Custom Cell Culture Media | Allows precise control over the concentration of every component, including NaCl and KCl. | Systematically varying the Na+:K+ ratio in an otherwise identical environment to study its specific effects on cell function [46]. |
| Potassium Chloride (KCl) | Source of K+ ions for adjusting media and buffers. | Used in electrophysiology to depolarize cells by altering the K+ equilibrium potential, or to correct for hypokalemia in animal models. |
| Sodium Chloride (NaCl) | Source of Na+ ions for adjusting media and buffers. | The primary salt for maintaining osmotic pressure; its concentration is carefully controlled when varying K+ to avoid confounding osmotic effects. |
| Portable Urine Na/K Meter | Provides immediate, on-site measurement of the urine sodium-to-potassium ratio [50]. | Useful in longitudinal animal studies or human clinical trials for rapid feedback on dietary or pharmacological interventions aimed at modifying electrolyte balance. |
A Technical Support Center for Intracellular Mimicry Research
This technical support resource provides troubleshooting guides and FAQs for researchers working to optimize K+ and Na+ levels in experiments involving macromolecular crowding, a key factor for accurate intracellular mimicry.
Frequently Asked Questions (FAQs)
1. What is macromolecular crowding and why is it critical for intracellular mimicry? Macromolecular crowding refers to the densely packed environment inside a cell, where macromolecules (proteins, nucleic acids, etc.) occupy 5–40% of the total cellular volume [55]. Contrary to typical in vitro media, this environment is "crowded" because no single molecular species is necessarily at a high concentration, but the total concentration of all macromolecules is very high [55]. This crowding strongly affects biochemical activities by reducing the available solvent volume for other molecules, a phenomenon known as the excluded-volume effect [55]. For research aiming to mimic the intracellular environment, incorporating crowding agents is essential to replicate the physiologically relevant thermodynamics, diffusion rates, and reaction kinetics of a living cell [55].
2. How does macromolecular crowding affect the diffusion and activity of ions like K+ and Na+? While crowding agents do not directly change the primary sequence of ions, they profoundly alter the physical environment. Crowding reduces the diffusion coefficients of proteins and other molecules [55]. In the context of ion regulation, this means that the mobility of ions and the proteins that transport them (such as Na+/H+ exchangers and cation-Cl− cotransporters) can be significantly impacted [55]. Furthermore, the function of these transporters is often dependent on cytoplasmic pH and ATP levels, which are also influenced by the crowded milieu [55]. Therefore, an increase in crowding agent concentration can affect the kinetics and equilibrium of ion transport systems crucial for maintaining K+ and Na+ levels.
3. My experimental reaction rates are slower than expected in a crowded system. Is this normal? Yes, this is a documented effect of macromolecular crowding. A sudden increase in crowding concentration, similar to what occurs during osmotic stress, has been shown to slow down biochemical processes, including signaling pathways and protein transport [55]. For example, in yeast, a reduction in cell volume (which increases crowding) decreased the diffusion coefficient of the Hog1p protein, as well as its phosphorylation rate and nuclear import [55]. This suggests that your observations may be physiologically consistent. The reduction is often reversible upon a return to less crowded conditions, mirroring a regulatory volume increase (RVI) in cells [55].
4. Can changes in intracellular K+ and Na+ levels influence macromolecular crowding itself? Absolutely. Cell volume regulation is considered a byproduct of regulating cytosolic macromolecular crowding, ion pumps, and channels [55]. Ion transporters like Na+/H+ exchangers and Cl−/HCO3− exchangers work together to import NaCl, which can lead to a regulatory volume increase (RVI) [55]. Therefore, perturbations in K+ and Na+ levels can directly affect cell volume, which in turn directly alters the concentration of macromolecular crowding agents in the cytoplasm, creating a feedback loop [55].
5. Under crowded conditions, some of my proteins are forming filaments or large aggregates. Is this an artifact? Not necessarily. Macromolecular crowding can promote molecular associations and is a known driver of protein fibrillation and the formation of large complexes [55]. For instance, under stress conditions like low nutrients (which can be linked to cytoplasmic acidification and volume changes), the enzyme glutamine synthetase (Gln1) has been observed to form filaments in yeast cells [55]. This structural reorganization, driven by crowding, can be a physiological mechanism to inactivate and store metabolic enzymes during stress [55].
Troubleshooting Guides
Issue: Inconsistent Results in Ion-Sensitive Assays Under Crowded Conditions
Problem Description: Measurements of K+ and Na+ activity or concentration yield highly variable data when macromolecular crowding agents are introduced into the in vitro system.
| Potential Cause | Description & Diagnostic Steps | Solution |
|---|---|---|
| Incorrect Osmolarity | Crowding agents significantly contribute to solution osmolarity, potentially causing unintended shrinkage or swelling of any cellular components or vesicles in the assay. | Use an osmometer to measure the final osmolarity of your crowded buffer. Adjust with salts or water to match physiological conditions (typically ~290 mOsm). |
| Altered Electrostatic Environment | High concentrations of crowding agents (especially if charged) can shield ionic interactions or create a local ionic environment that affects ion-sensitive electrodes or dyes. | • Characterize the charge of your crowding agent.• Run a standard curve for your ion assay in the exact crowded buffer.• Consider using a different, neutral crowding agent like Ficoll. |
| Precipitated Reagents | Some salts or assay components may have limited solubility in the presence of high concentrations of crowding agents, leading to precipitation and inconsistent availability. | Visually inspect solutions for cloudiness. Centrifuge the crowded buffer prior to assay to remove any insoluble material. Confirm all components are soluble under crowded conditions. |
Issue: Unexpected Reduction in Enzyme Kinetics or Signaling Pathway Activity
Problem Description: After adding crowding agents to mimic the intracellular environment, the activity of a studied enzyme or signaling pathway is significantly lower than in dilute buffer.
| Potential Cause | Description & Diagnostic Steps | Solution |
|---|---|---|
| Reduced Molecular Diffusion | Crowding physically hinders the movement of molecules, leading to slower diffusion-limited encounters between enzymes and substrates or signaling molecules [55]. | This may be an expected effect. Confirm by measuring the diffusion coefficient of a fluorescently labeled tracer protein (e.g., GFP) in your system using FRAP or FCS. |
| Viscosity Artifacts | The increased viscosity from crowding agents can slow down pipetting and mixing steps, leading to poor reagent homogeneity and inaccurate timing in kinetic assays. | • Pre-mix all crowded solutions thoroughly and allow them to equilibrate to the assay temperature.• Use positive displacement pipettes for highly viscous solutions.• Validate mixing efficiency. |
| Non-Specific Binding | Proteins may exhibit low-affinity, non-specific binding to the crowding agents themselves, effectively reducing the concentration of free, active protein. | Perform a control experiment using a density variation of the crowding agent. If activity decreases linearly with increased crowding beyond the expected effect, non-specific binding may be occurring. |
Experimental Protocols & Workflows
Protocol 1: Systematically Titrating Crowding Agents to Modulate K+ and Na+ Transporter Activity
Objective: To establish a dose-response relationship between the concentration of macromolecular crowding agents and the activity of a specific ion transporter (e.g., Na+/K+ ATPase) in a reconstituted system.
Materials:
- Purified ion transporter protein or membrane vesicles.
- Macromolecular crowding agents (e.g., Ficoll 70, PEG 8000, Dextran).
- Assay buffer (appropriate pH and base osmolarity).
- ATP regeneration system.
- Method for quantifying ion transport (e.g., radioactive tracers, fluorescent dyes, ATP consumption assay).
Methodology:
- Prepare Crowding Stocks: Create highly concentrated, sterile stocks of your chosen crowding agents in the assay buffer.
- Osmolarity Matching: Measure the osmolarity of each crowding stock. Prepare a dilution series of the crowding agent in assay buffer, ensuring the final osmolarity is identical across all conditions by adding precise amounts of a concentrated salt solution or water. This isolates the effect of crowding from the effect of osmolarity.
- Reconstitute Transporter: Incorporate the purified transporter or vesicles into each crowding condition. Allow the system to equilibrate.
- Initiate Reaction: Start the transport reaction by adding ATP or the required initiator.
- Measure Activity: At designated time points, quantify transport activity using your chosen method.
- Data Analysis: Plot transporter activity (e.g., initial velocity) against the volume fraction of the crowding agent.
Protocol 2: Investigating the Combined Effects of Crowding and Cytosolic Acidification on Protein Aggregation
Objective: To study how a drop in intracellular pH, often linked to stress and ion imbalance, influences protein aggregation in a crowded environment.
Materials:
- Protein of interest (e.g., a metabolic enzyme like glutamine synthetase).
- Macromolecular crowding agents.
- Buffers with varying pH (e.g., pH 7.4 and pH 6.5).
- Dynamic Light Scattering (DLS) instrument or analytical ultracentrifuge.
- Negative stain electron microscopy supplies.
Methodology:
- Set Up Conditions: Prepare solutions containing your protein in buffers at physiological (pH 7.4) and acidic (pH 6.5) pH, both with and without a high concentration of crowding agent.
- Incubate: Incubate all samples at the experimental temperature for a set period (e.g., 1-2 hours).
- Monitor Aggregation:
- Use DLS to measure the hydrodynamic radius of the particles in solution over time. A shift to larger sizes indicates aggregation or filament formation [55].
- Alternatively, use sedimentation assays or centrifugation to separate soluble and insoluble fractions.
- Visualize: For samples showing significant aggregation, use negative stain electron microscopy to visualize the morphology of the aggregates (e.g., amorphous aggregates vs. structured filaments) [55].
The following workflow diagram outlines this experimental process:
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and their functions for experiments in crowded environments.
| Reagent / Material | Primary Function in Experiment |
|---|---|
| Ficoll 70 | A neutral, highly branched polysaccharide used to mimic the steric (excluded volume) effects of macromolecular crowding without significant electrostatic interactions. Its ~70 kDa size is similar to many cytoplasmic proteins [55]. |
| PEG (Polyethylene Glycol) | A flexible polymer used to induce crowding. Different molecular weights (e.g., PEG 8000) allow tuning of the pore size of the crowded network. Can promote protein compaction and aggregation. |
| Dextran | A branched polysaccharide crowding agent available in various molecular weights. Used to study the effects of crowders with different physical properties on biochemical reactions. |
| Na+/K+ ATPase (Purified) | The primary ion transporter responsible for maintaining K+ and Na+ gradients across the plasma membrane. A key protein for studying ion regulation in crowded, mimicry-based systems. |
| Ion-Sensitive Fluorescent Dyes | Dyes (e.g., Sodium Green, PBFI) whose fluorescence changes upon binding specific ions (Na+, K+). Allow real-time monitoring of ion flux in crowded environments. |
| Osmometer | A critical instrument for measuring the total osmolarity of solutions. Essential for controlling and matching osmolarity when adding crowding agents to avoid confounding osmotic effects. |
The logical relationship between crowding, cellular conditions, and experimental outcomes is summarized below:
For researchers in intracellular mimicry and drug development, replicating the native cellular environment is paramount for obtaining physiologically relevant data. The careful optimization of potassium (K+) and sodium (Na+) levels is a cornerstone of this process, directly influencing crucial parameters like osmolarity, membrane stability, and redox potential. Imbalances in these electrolytes can compromise experimental integrity, leading to aberrant cellular behavior and unreliable results. This guide addresses specific, common pitfalls associated with K+ and Na+ management in cell culture systems, providing targeted troubleshooting strategies to enhance the reproducibility and biological significance of your research.
Troubleshooting Guides
Problem 1: Inconsistent Cell Growth and Viability
Problem Statement: Cell cultures exhibit poor growth rates, decreased viability, or morphological changes between passages, suspected to be caused by suboptimal culture conditions, specifically osmolarity stress from electrolyte imbalance.
Investigation & Diagnosis:
- Check Culture Media: Verify the documented K+ and Na+ concentrations in your basal media and any supplements. Calculate the final theoretical ratio and osmolarity.
- Measure Osmolarity: Use an osmometer to measure the actual osmolarity of your prepared culture medium. Compare it to the optimal range for your specific cell type (typically ~280-300 mOsm/kg for mammalian cells).
- Assess Viability: Quantify cell viability using trypan blue exclusion or a similar assay.
- Review Protocol: Scrutinize your media preparation logs for inconsistencies in salt stock concentrations, dilution errors, or incomplete mixing.
Solution: Re-constitute and pH-balance your culture media according to a standardized, documented protocol. Fine-tune the K+/Na+ ratio based on the specific needs of your cell type. For intracellular mimicry, evidence suggests that maintaining a cellular K+/Na+ ratio above 10 is a target, influenced by a dietary K/Na ratio well above 1, and preferably 5 or higher [56]. Ensure consistent preparation to avoid batch-to-batch variability.
Problem 2: Elevated Oxidative Stress in Cultures
Problem Statement: Cells in culture show signs of elevated reactive oxygen species (ROS), leading to increased DNA damage, chronic inflammation, and hindered regeneration, potentially linked to high sodium conditions.
Investigation & Diagnosis:
- Quantify ROS: Use a fluorescent ROS probe (e.g., DCFDA) or a glutathione assay kit to measure oxidative stress levels in treated vs. control cultures.
- Analyze DNA Damage: Perform a comet assay or immunostaining for DNA damage markers like γH2AX.
- Review Sodium Load: Evaluate if the sodium concentration in your media is unnecessarily high. Note that high salt environments have been shown to increase DNA breaks and promote a pro-inflammatory milieu conducive to cancer formation [57].
Solution: Modulate the culture medium to reduce sodium content while increasing potassium, aiming for a more physiologically balanced K+/Na+ ratio. Incorporate ROS-scavenging agents into your culture system. Research on bioscaffolds has demonstrated that incorporating antioxidant agents like quercetin, allantoin, and caffeic acid can effectively neutralize ROS levels and promote a regenerative microenvironment [58].
Problem 3: Disrupted Intracellular Signaling and Transmembrane Potential
Problem Statement: Experimental outcomes indicate aberrant cell signaling, disrupted membrane potentials, and abnormal responses to external stimuli, potentially stemming from a dysfunctional sodium-potassium pump (Na+/K+ ATPase).
Investigation & Diagnosis:
- Measure Electrolytes: If feasible, use techniques like 23NaMRI to accurately determine intracellular Na+ and K+ concentrations without disrupting cellular membranes [57].
- Monitor Membrane Potential: Use potentiometric dyes to assess changes in the transmembrane potential.
- Check Inhibitors: Confirm that no experimental compounds in use are unintended inhibitors of the Na+/K+ ATPase.
Solution: Ensure the culture medium provides an adequate and balanced supply of both K+ and Na+ to fuel the sodium-potassium pump. Chronic lowering of the transmembrane potential due to reduced activity of this pump can initiate and sustain mitosis, altering fundamental cellular behavior [57]. The optimal ratio is critical for maintaining resting membrane potentials, especially in cardiac and neural cells [59].
Frequently Asked Questions (FAQs)
FAQ 1: What is the optimal potassium-to-sodium ratio for cell culture media aimed at intracellular mimicry? While the ideal ratio can be cell-type specific, a foundational goal is to mimic the high intracellular K+/Na+ ratio found in vivo. Evidence points to a target cellular K+/Na+ ratio above 10 [56]. This is supported by evolutionary and epidemiological data indicating that a high dietary K/Na ratio is associated with positive health outcomes, suggesting that media formulations with a K/Na ratio well above 1 (preferably 5 or higher) are a sound starting point for creating a physiologically normal ionic environment [56].
FAQ 2: How can high sodium levels in my culture system increase oxidative stress? High salt environments can induce intracellular sodium accumulation even when plasma (extracellular) concentrations appear normal [57]. This elevated intracellular Na+ acts as an environmental stressor, leading to increased production of Reactive Oxygen Species (ROS) [57]. High ROS levels can, in turn, cause significant DNA damage and create a pro-inflammatory, pro-carcinogenic microenvironment that can derail experiments focused on normal cellular processes [57].
FAQ 3: What are the clinical manifestations of potassium imbalance that can inform in vitro models? Understanding the systemic effects of electrolyte imbalance in humans can provide clues for cellular-level phenomena in culture. The table below summarizes the clinical manifestations.
Table: Clinical Manifestations of Potassium Imbalances as an Analog for Cellular Dysfunction
| Imbalance | Clinical Manifestations (Human) | Potential Parallels in Cell Culture |
|---|---|---|
| Hypokalemia (Low K+) | Muscle weakness, cramps, cardiac arrhythmias (depressed T waves, prolonged PR interval), constipation, fatigue [60]. | Reduced contractility, aberrant electrophysiology, decreased metabolic activity, and general loss of cellular function. |
| Hyperkalemia (High K+) | Muscle weakness, flaccid paralysis, cardiac arrhythmias (peaked T waves, bradycardia) [60]. | Hyperexcitability followed by cessation of signaling, uncontrolled contraction, and cell death. |
FAQ 4: Which essential reagents are critical for managing K+ and Na+ levels in culture? Key reagents are needed to establish, maintain, and monitor the ionic environment. The following table lists essential items for the researcher's toolkit.
Table: Research Reagent Solutions for K+ and Na+ Management
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Potassium Chloride (KCl) / Sodium Chloride (NaCl) Stocks | To supplement and fine-tune the base electrolyte concentrations in culture media. | Use high-purity, cell culture-grade reagents. Prepare concentrated stock solutions for accurate, sterile addition. |
| Osmometer | To measure the total solute concentration (osmolarity) of the prepared culture medium. | Critical for verifying that media preparation is consistent and within the physiological range for your cells. |
| Sodium-Potassium Pump Inhibitors (e.g., Ouabain) | Pharmacological tools to intentionally disrupt the Na+/K+ gradient for mechanistic studies. | Use at validated concentrations to avoid complete, toxic inhibition. |
| ROS-Scavenging Agents (e.g., Quercetin, Allantoin) | To modulate oxidative stress in culture, which can be exacerbated by high Na+ conditions [58]. | Can be incorporated into delivery systems like bioscaffolds or directly solubilized in media. |
| Ion-Specific Electrodes / 23NaMRI | For direct measurement of intracellular K+ and Na+ concentrations. | 23NaMRI allows for non-invasive and non-destructive determination in viable cells and tissues [57]. |
Experimental Protocols
Protocol 1: Optimizing K+/Na+ Ratio in a Custom Culture Medium
Objective: To systematically determine the K+/Na+ ratio that maximizes cell viability and growth for a specific cell line in a custom intracellular mimicry model.
Materials:
- Basal medium (low in K+ and Na+)
- High-purity KCl and NaCl
- Cell line of interest
- Cell culture plates
- Cell counter and viability assay kit (e.g., trypan blue)
- Osmometer
Methodology:
- Prepare Media Variants: Prepare a series of media formulations where the total ionic strength is kept constant, but the K+/Na+ ratio is varied (e.g., 1:1, 2:1, 5:1, 10:1).
- Verify Osmolarity: Measure and confirm the osmolarity of each media variant is within the acceptable range for your cell type.
- Seed Cells: Seed cells at a standardized density in triplicate for each media condition.
- Maintain and Harvest: Culture cells for 72-96 hours, maintaining standard conditions (37°C, 5% CO2).
- Analyze Growth: Harvest cells at 24-hour intervals and perform cell counts and viability assays.
- Data Analysis: Plot growth curves and viability for each condition. The ratio supporting the highest viability and most consistent growth rate without morphological changes is the optimal starting point for further experiments.
Protocol 2: Quantifying Oxidative Stress Under Different Electrolyte Conditions
Objective: To measure the level of ROS in cells cultured in media with high Na+ versus a balanced K+/Na+ ratio.
Materials:
- Control medium (balanced K+/Na+)
- High-Na+ test medium
- Fluorescent ROS probe (e.g., DCFDA)
- Microplate reader or flow cytometer
- 96-well black-walled plates or flow cytometry tubes
Methodology:
- Culture Cells: Culture cells in the control and high-Na+ media for 48 hours.
- Load Probe: Harvest cells, wash with PBS, and incubate with the ROS probe according to the manufacturer's instructions.
- Measure Fluorescence: For plate readers, transfer cells to a 96-well plate and measure fluorescence. For flow cytometry, analyze the fluorescence intensity of the cell population.
- Statistical Analysis: Compare the mean fluorescence intensity between the control and test groups. A significant increase in the high-Na+ group confirms elevated oxidative stress [57].
Signaling Pathways and Workflows
Sodium-Potassium Pump & Stress Pathway
This diagram illustrates the core function of the Na+/K+ ATPase pump in maintaining the electrochemical gradient and how its disruption leads to downstream stress pathways.
Experimental Optimization Workflow
This flowchart outlines the systematic process for diagnosing and correcting electrolyte-related issues in cell culture.
Benchmarking Success: Validating and Comparing Cytomimetic Assay Performance
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between Kd, IC50, and EC50? These three metrics are often confused but measure distinct aspects of a molecular interaction.
- Kd (Dissociation Constant): Measures the binding affinity between two molecules, such as a drug and its target. A lower Kd value indicates stronger binding. It is a direct measure of the binding equilibrium [61].
- IC50 (Half-Maximal Inhibitory Concentration): Measures the potency of an inhibitor. It is the concentration of a drug needed to inhibit a biological process or response by 50%. A lower IC50 indicates higher inhibitory potency [61].
- EC50 (Half-Maximal Effective Concentration): Measures the potency of an agonist. It is the concentration of a compound required to induce a 50% response. A lower EC50 indicates higher efficacy at triggering a response [61].
It is a common mistake to assume a lower IC₅₀ or EC₅₀ always means stronger binding (lower Kd). Functional potency (IC₅₀/EC₅₀) can be influenced by experimental conditions and downstream cellular processes, and may not directly reflect the pure binding affinity measured by Kd [61].
Q2: Why is it crucial to verify equilibration time when measuring in-cell Kd? An equilibrium state, by definition, does not change with time. Failing to ensure that a binding reaction has reached equilibrium is a primary source of incorrect Kd values [62].
- The Risk: Without demonstrating that the fraction of bound complex is constant over time, a reported "equilibrium" Kd value may be inaccurate, potentially leading to biological misinterpretations [62].
- The Solution: The reaction must be monitored over time until the binding signal stabilizes. For a simple binding process, reaching five half-lives (96.6% completion) is a conservative standard to ensure equilibration. The required time is highly dependent on the dissociation rate constant (k~off~); tighter binders (with very low Kd) often have very slow k~off~ values and can require exceptionally long incubation times to reach equilibrium [63] [62].
Q3: How can intracellular K+ and Na+ levels affect my binding experiments? The gradients of K+ and Na+ across the cell membrane are fundamental to cellular physiology and can directly impact assay systems and drug mechanisms.
- Ion Gradients: In a resting cell, potassium ions (K+) are highly concentrated inside the cell, while sodium ions (Na+) are highly concentrated outside. This gradient is maintained by the sodium-potassium pump (Na+/K+ ATPase), which actively transports 3 Na+ ions out for every 2 K+ ions it brings in [64] [65].
- Cellular Consequences: The Na+/K+ ATPase is critical for maintaining the resting membrane potential and overall cellular homeostasis [64]. Blocking this pump, for example with a compound like strophanthidin, disrupts ion balance, leading to a rise in intracellular Na+ and a loss of intracellular K+, which can depolarize the cell and increase excitability [66] [67]. This can alter the cellular context in which you are measuring drug binding or activity.
- Relevance for In-Cell Kd: Using live cells for Kd measurements preserves the native membrane environment and physiological ion gradients, which can be crucial for the target receptor's 3D structure and function. Measured Kd values can vary significantly if the receptor is presented on live cells versus as an isolated recombinant protein [63].
Troubleshooting Guides
Issue 1: Discrepancy Between Flow Cytometry and LigandTracer Kd Values
Problem: You are measuring the affinity of a therapeutic antibody for its cell-surface receptor using both end-point flow cytometry and real-time LigandTracer. The calculated Kd values from the two methods do not match.
Investigation and Solutions:
- Root Cause 1: Lack of Equilibration in Flow Cytometry.
- Description: Flow cytometry often involves incubating cells with a fluorescent ligand for a fixed time before measurement. If this incubation time is insufficient for the system to reach true equilibrium, the resulting titration curve will be distorted, leading to an incorrect Kd [63].
- Solution:
- Perform a time-course experiment. Measure binding at your highest and lowest ligand concentrations across multiple time points (e.g., 30 min, 1 hr, 2 hr, 4 hr, 8 hr).
- Confirm that the measured binding signal has reached a stable plateau at all concentrations before taking your final measurement for the titration curve [62].
- Root Cause 2: Titration Artifact.
- Description: This occurs when the concentration of the receptor on the cells (the limiting component) is too high relative to the Kd being measured (R0 >> KD). This can deplete the free ligand concentration and skew the binding isotherm, resulting in an overestimated Kd [63] [62].
- Solution:
- Ensure that the receptor concentration is less than or equal to the Kd (R0 ≤ KD). If the receptor expression level is unknown, empirically demonstrate that the measured Kd is independent of cell concentration [62].
- LigandTracer, which analyzes binding kinetics over time, is less susceptible to this artifact and can provide a more reliable Kd from which the flow cytometry data can be re-analyzed [63].
- Root Cause 3: Instrument and Live-Cell Context.
- Description: LigandTracer provides real-time, kinetic data on live cells, giving direct access to kon and koff rates (KD = koff/kon). Flow cytometry is an end-point method that infers Kd from a single snapshot in time [63].
- Solution: Use the kinetic rate constants (k~on~ and k~off~) obtained from LigandTracer to model the expected binding at the specific time point used in your flow cytometry protocol. This can help reconcile the two datasets and confirm if the flow cytometry incubation time was sufficient [63].
Issue 2: High Background or Non-Specific Binding in Live-Cell Assays
Problem: Your binding signal is weak or inconsistent due to high background noise from non-specific interactions.
Investigation and Solutions:
- Root Cause 1: Non-optimized assay buffer or cell health.
- Description: Serum components or cellular debris can contribute to non-specific binding. Furthermore, unhealthy or stressed cells may have leaky membranes, altering the assay background [63] [67].
- Solution:
- Include relevant controls such as unlabeled competitor compounds or isotype control antibodies to block specific binding and quantify non-specific signal.
- Use a buffer with a carrier protein like BSA to block non-specific sites.
- Ensure cells are healthy and used at an appropriate passage number. Monitor intracellular ion levels if pump inhibitors or ionophores are used, as these can affect viability and membrane integrity [66] [67].
Issue 3: No Binding Signal Detected
Problem: You cannot detect any specific binding of your ligand to the live cells.
Investigation and Solutions:
- Root Cause 1: Inactive protein or incorrect cell line.
- Description: The protein may have lost activity during purification or labeling. Alternatively, the cell line may not express the target receptor [62].
- Solution:
- Determine Active Protein Fraction: Use an independent method or a known standard to determine the fraction of your protein that is functionally active. An underestimated active concentration will lead to an incorrect Kd [62].
- Verify Cell Line and Reagents: Confirm target receptor expression in your cell line via PCR or western blot. Validate that all fluorescent labels are functional and do not interfere with binding [63].
Experimental Protocols & Data Presentation
Protocol 1: Time-Resolved Binding Measurement on Live Cells using LigandTracer
This protocol is adapted from methods used to characterize therapeutic antibodies [63].
1. Key Research Reagent Solutions
| Reagent/Material | Function in the Protocol |
|---|---|
| SKBR3, SKOV3, or Daudi Cells | Live cell systems expressing the native, target receptor of interest (e.g., HER2, CD20). |
| Trastuzumab, Rituximab, etc. | Model therapeutic antibodies that bind to specific cell-surface receptors. |
| Fluorescent Label (e.g., CF 488A, FITC) | Tags the antibody to allow for real-time detection of binding. |
| Tilted Cell Culture Dish | Specialized dish that facilitates gentle mixing and continuous monitoring in the LigandTracer instrument. |
| LigandTracer Instrument | Platform that enables real-time, kinetic monitoring of ligand-receptor binding on live cells. |
2. Methodology
- Cell Seeding: Lift cells with Accutase, count, and resuspend at a density of 3.3 × 10^5^ cells/mL. Seed 3 mL of the suspension into a tilted Petri dish. Allow cells to adhere for 4 hours at 37°C, then replace medium with 12 mL of fresh medium and incubate horizontally overnight. Perform experiments 2-3 days post-seeding [63].
- Labeling: Label the antibody of interest (e.g., Trastuzumab) according to the manufacturer's instructions for the labeling kit (e.g., Mix-n-Stain CF 488A) or using standard protocols for FITC conjugation. Purify the labeled antibody using a NAP-5 column and store in aliquots at -20°C [63].
- Binding Measurement: Place the cell dish on the LigandTracer stage. The instrument will rotate the dish, alternately moving the cell layer in and out of the detection area. Gradually add increasing concentrations of the fluorescently labeled antibody to the dish. Monitor the increase in binding signal over time for each concentration during the "association" phase. Subsequently, replace the ligand solution with fresh medium to monitor the decrease in signal over time ("dissociation" phase) [63].
- Data Analysis: Globally fit the association and dissociation curves for all concentrations to a suitable binding model (e.g., 1:1 interaction) to extract the kinetic rate constants, k~on~ and k~off~. The equilibrium dissociation constant is calculated as KD = k~off~/k~on~ [63].
Protocol 2: Validating Equilibration Time for End-Point Binding Assays
This protocol is critical for techniques like flow cytometry or fluorescence anisotropy [62].
1. Methodology
- Prepare samples with a fixed concentration of cells/receptor and two key ligand concentrations: one near your estimated Kd and a saturating concentration (e.g., 10 × Kd).
- Instead of a single incubation, incubate multiple replicates for different time periods (e.g., 0.5, 1, 2, 4, 8, 16 hours).
- At each time point, measure the binding signal (e.g., mean fluorescence intensity via flow cytometry).
- Plot the binding signal versus time for both concentrations. The minimum incubation time required for your assay is the point after which both curves have clearly plateaued.
2. Data Interpretation The diagram below illustrates the logic of this validation experiment.
Table 1: Relationship Between Theoretical KD, Kon, and Time to Equilibrium This table estimates the time required to reach equilibrium based on binding kinetics, assuming a diffusion-limited kon of 10^8^ M^-1^s^-1^. In practice, kon may be slower, requiring longer incubation [62].
| KD Value | koff (s⁻¹)* | Estimated Time to ~97% Equilibrium (5 × t½) | Practical Consideration |
|---|---|---|---|
| 1 µM | 100 | ~40 ms | Very fast; standard incubations are sufficient. |
| 1 nM | 0.1 | ~40 seconds | Still rapid; easy to achieve equilibrium. |
| 1 pM | 0.0001 | ~10 hours | Challenging; requires long incubation and high system stability. |
*Calculated as k~off~ = K~D~ × k~on~.
Table 2: Comparison of Binding Measurement Techniques
| Technique | Measures | Key Advantage | Key Limitation | Live-Cell Context? |
|---|---|---|---|---|
| LigandTracer | Kinetics (k~on~, k~off~), Kd | Directly measures kinetics on live cells; avoids titration artifacts. | Lower throughput; requires specialized instrument. | Yes [63] |
| Flow Cytometry | Kd (end-point) | High throughput; can analyze heterogeneous cell populations. | Prone to errors from insufficient equilibration time. | Yes [63] |
| Isothermal Titration Calorimetry (ITC) | Kd, ΔH, ΔS | Label-free; provides full thermodynamic profile. | Typically uses purified components, not live cells. | No [62] |
| Surface Plasmon Resonance (SPR) | Kinetics (k~on~, k~off~), Kd | High-quality kinetic data; label-free. | Typically requires immobilized recombinant protein. | No [62] |
FAQs & Troubleshooting Guides
Frequently Asked Questions
1. Why is PBS not suitable for experiments aiming to mimic the intracellular environment?
PBS is designed to mimic extracellular fluid, not the conditions inside a cell. Its ionic composition is the inverse of the cytoplasm. The dominant cation in PBS is sodium (Na+ at ~157 mM), with very low potassium (K+ at ~4.5 mM). In contrast, the intracellular environment is characterized by high K+ (~140-150 mM) and low Na+ (~14 mM) concentrations [29]. Using PBS to study intracellular targets or processes therefore creates a non-physiological ionic environment, which can skew binding affinity (Kd) measurements and other biochemical data [29].
2. We often see a poor correlation between the activity of a compound in a biochemical assay and its activity in a subsequent cellular assay. Could the buffer choice be a factor?
Yes, this is a common and significant issue, and buffer choice is very likely a contributing factor [29]. The discrepancy between biochemical assay (BcA) and cell-based assay (CBA) results is often attributed to compound permeability or stability. However, even when these factors are accounted for, differences can persist because the simplified conditions of a standard BcA (e.g., in PBS) do not replicate the crowded, viscous, and chemically distinct environment of the cytoplasm [29]. These physicochemical differences can cause Kd values measured in vitro to be orders of magnitude different from those in a cellular context [29].
3. What are the key characteristics of a cytomimetic buffer?
A true cytomimetic buffer should replicate several physicochemical conditions of the cytoplasm [29]:
- Ionic Composition: High K+ (~140-150 mM) and low Na+ (~14 mM) concentrations [29].
- Macromolecular Crowding: Inclusion of crowding agents (e.g., PEG, Ficoll) to mimic the high concentration of macromolecules in the cell, which affects binding kinetics and protein stability [29].
- Viscosity: Modification of viscosity to match the cytoplasmic environment [29].
- pH: Maintenance of a physiological cytoplasmic pH [29].
- Redox Potential: Consideration of the more reducing environment of the cytosol, though caution is needed as common reducing agents (e.g., DTT) can denature some proteins [29].
4. For long-term mechanical testing of tissues, why might PBS be problematic?
Research on tendon fascicles has shown that incubation in PBS increases tissue water content (swelling) and decreases tensile stiffness [68]. Furthermore, small solutes like NaCl (a key component of PBS) can diffuse into the tissue over long periods (e.g., 8 hours), which can alter the measured mechanical properties. For long-term tests, alternative buffers using large polymers like polyethylene glycol (PEG) are recommended to maintain hydration without solute diffusion and mechanical artifacts [68].
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| Discrepancy between biochemical and cellular assay results. | Biochemical assay buffer (e.g., PBS) does not mimic intracellular conditions, altering compound binding affinity [29]. | Develop a cytomimetic buffer with high K+, low Na+, and molecular crowding agents for the biochemical assay [29]. |
| High background in flow cytometry when using a primary antibody from the same species as the sample. | Secondary antibody cross-reacts with endogenous immunoglobulins in the sample [69]. | Use a primary antibody raised in a species different from your sample. If unavoidable, use a blocking step or select chimeric antibodies [69]. |
| Tissue swelling and altered mechanical properties during long-term biomechanical testing. | Solutes in standard saline buffers (e.g., in PBS) diffuse into tissue, changing hydration and mechanics [68]. | Switch to an alternative bathing solution like PEG or a PEG-NaCl mixture (SPEG) to maintain hydration without solute diffusion [68]. |
| Poor conjugation efficiency when labeling a primary antibody. | Carrier proteins (e.g., BSA) or preservatives (e.g., sodium azide) in the antibody storage buffer compete for the label [69]. | Purchase antibody formulations without carriers or preservatives for conjugation experiments [69]. |
| Low signal from a low-abundance intracellular target. | Direct detection with a conjugated primary antibody may not provide sufficient signal amplification [69]. | Use an indirect detection method with a conjugated secondary antibody, which allows multiple secondary antibodies to bind to each primary, amplifying the signal [69]. |
Experimental Data & Protocols
Quantitative Comparison of Buffer Compositions
Table 1: Ionic composition of standard PBS versus the physiological intracellular environment.
| Ion / Parameter | Standard PBS (1x) | Intracellular Environment (Cytosol) |
|---|---|---|
| Na+ Concentration | ~157 mM [29] [70] | ~14 mM [29] |
| K+ Concentration | ~4.5 mM [29] [70] | ~140-150 mM [29] [65] |
| Cl- Concentration | ~140 mM [70] | Information missing |
| Primary Cation | Sodium (Na+) [29] | Potassium (K+) [29] |
Table 2: Impact of physicochemical parameters on molecular interactions.
| Parameter | Standard Buffer (e.g., PBS) Conditions | Cytoplasmic Conditions | Impact on Binding (Kd) & Activity |
|---|---|---|---|
| Macromolecular Crowding | Dilute, non-crowded solution [29] | Highly crowded (20-30% of volume occupied) [29] | Kd values can differ by up to 20-fold or more; enzyme kinetics can change significantly (up to 2000%) [29]. |
| Cationic Composition | High Na+, Low K+ [29] | High K+, Low Na+ [29] | Alters electrostatic interactions and protein-ligand binding affinities that are cation-sensitive [29]. |
| Viscosity | Low viscosity [29] | High viscosity [29] | Affects diffusion rates and binding kinetics of molecules [29]. |
Detailed Experimental Protocols
Protocol 1: Measuring the Effect of Buffer Conditions on Ligand-Protein Binding Affinity (Kd)
This protocol outlines a method to compare the binding affinity of a ligand to its target protein in a standard buffer versus a cytomimetic buffer.
- Protein Purification: Purify the recombinant target protein using standard methods (e.g., affinity chromatography) [71].
- Buffer Preparation:
- Standard Buffer: Prepare a standard buffer such as PBS or Tris-buffered saline.
- Cytomimetic Buffer: Prepare a cytomimetic buffer containing, for example, 140 mM KCl, 10 mM NaCl, 10 mM HEPES (pH 7.4), and a crowding agent like 5% w/v PEG 8000 [29].
- Sample Preparation: Dilute the purified protein to the same concentration in both buffers.
- Binding Measurement: Use a technique like surface plasmon resonance (SPR) or isothermal titration calorimetry (ITC) to measure the binding affinity.
- For SPR, immobilize the protein on a sensor chip and flow the ligand at varying concentrations in the respective buffers.
- For ITC, titrate the ligand solution into the protein solution, both prepared in the same buffer.
- Data Analysis: Analyze the resulting data to calculate the equilibrium dissociation constant (Kd) for the interaction in each buffer. Compare the Kd values to assess the impact of the buffer environment.
Protocol 2: Testing Buffer Effects on Tissue Mechanics
This protocol, adapted from tendon research, assesses how different buffers affect tissue hydration and mechanics over time [68].
- Tissue Harvesting: Harvest tissue samples (e.g., rat tail tendon fascicles) and divide them into matched groups.
- Buffer Incubation: Incubate each group in a different buffer solution for a defined period (e.g., 15 minutes vs. 8 hours). Test buffers can include:
- PBS (0.9% NaCl)
- High-concentration NaCl (25%)
- Polyethylene glycol (PEG) solution (8%)
- A combination of NaCl and PEG (SPEG) [68]
- Hydration Test:
- Weigh the sample after incubation (
W_wet). - Dry the sample completely and weigh again (
W_dry). - Calculate the apparent water content:
φ_app = (W_wet - W_dry) / W_wet[68].
- Weigh the sample after incubation (
- Mechanical Testing:
- Mount the incubated sample on a mechanical testing system.
- Perform a tensile test or a stress-relaxation test to determine parameters like elastic modulus and equilibrium stress.
- Analysis: Compare the hydration levels and mechanical properties of tissues incubated in different buffers to identify solutions that maintain native tissue properties.
Research Reagent Solutions
Table 3: Essential materials for cytomimetic buffer research.
| Reagent | Function / Explanation |
|---|---|
| Potassium Chloride (KCl) | The primary salt used to achieve the high intracellular K+ concentration (~140-150 mM) in cytomimetic buffers [29]. |
| Macromolecular Crowding Agents (e.g., PEG, Ficoll) | Inert polymers used to simulate the crowded intracellular environment, which significantly influences molecular interactions and protein stability [29]. |
| HEPES Buffer | A buffering agent used to maintain physiological pH in vitro. Its pKa (7.5) is suitable for maintaining a cytosolic pH [71]. |
| Recombinant Antibodies | Antibodies produced using synthetic genes. They offer superior specificity, reproducibility, and long-term supply compared to traditional monoclonal or polyclonal antibodies, reducing experimental variability [69]. |
| Fc Receptor Blocking Reagents | Used in flow cytometry to block non-specific binding of antibodies to Fc receptors on immune cells, reducing background signal and improving data quality [33]. |
Visualizations
Diagram 1: Experimental workflow for buffer comparison
Diagram 2: Buffer impact on experimental outcomes
Technical Support Center
Troubleshooting Guide: Genetically Encoded Ion Sensors
FAQ 1: My potassium sensor shows a slow or no response to neuronal activity. What should I check?
- Problem: The FRET-based K+ biosensor lc-LysM GEPII 1.0 may fail to resolve small intracellular potassium changes during brief activity patterns like single action potentials [22].
- Solution:
- Validate with intense stimulation: Test sensor functionality by inducing large potassium fluxes first. Use seizure-like activity or intense optogenetic stimulation to trigger measurable [K+] decreases [22].
- Optimize sensor targeting: Ensure proper subcellular localization. The sensor can be targeted to the cytosol (cyto), plasma membrane (SubPM), or mitochondria (mito) using specific targeting sequences [22].
- Confirm expression and functionality: Purify the sensor protein and test its functionality in vitro using a plate reader or microscope, recording excitation/emission spectra and calibration curves with varying K+ concentrations [22].
FAQ 2: How can I improve the signal-to-noise ratio for in vivo potassium imaging?
- Problem: Measurements in live animals can be affected by background noise, motion artifacts, or low signal strength.
- Solution:
- Use Fluorescence Lifetime Imaging (FLIM): For FRET-based sensors like lc-LysM GEPII 1.0, perform 2-photon fluorescence lifetime imaging in vivo. The lifetime metric is more robust against motion artifacts and variations in excitation light or sensor concentration than intensity-based measurements [22].
- Employ cell-type-specific expression: Use cell-specific promoters (e.g., the neuronal hSyn promoter) to restrict sensor expression to the cell population of interest, reducing background signal [22].
- Ensure proper viral delivery: Use high-titer adeno-associated viral (AAV) particles, produced in HEK293T cells and purified, for efficient in vivo sensor delivery [22].
FAQ 3: My ion-selective measurements are unstable and show significant drift.
- Problem: potentiometric measurements are highly temperature-dependent [72].
- Solution:
- Control temperature rigorously: A 5°C temperature discrepancy can alter concentration readings by at least 4%. Ensure the sensor and solutions are in full thermal equilibrium, which can take 30-60 minutes under non-ideal conditions [72].
- Calibrate correctly: Always use a two-point calibration with solutions that bracket the expected sample concentration (interpolation), not extrapolation. Calibration standards should closely mirror the ionic background of your sample [72].
- Avoid air bubbles: Install the sensor at a 45-degree angle above horizontal to prevent air bubbles from adhering to the sensing membrane and causing erratic readings [72].
Table 1: Troubleshooting Genetically Encoded Ion Sensors
| Problem | Potential Cause | Solution |
|---|---|---|
| Slow/No Sensor Response [22] | Small [K+] changes; low-affinity sensor | Use intense stimulation; validate with large flux events. |
| Poor Signal in Live Imaging [22] | Motion artifacts; low expression; background | Use FLIM; employ cell-specific promoters; ensure high-titer AAV. |
| Signal Drift/Instability [72] | Temperature fluctuations; improper calibration | Ensure thermal equilibrium; use two-point interpolation calibration. |
Troubleshooting Guide: In-Cell NMR
FAQ 1: How can I ensure successful delivery of protein and RNA components for in-cell NMR studies?
- Problem: In-cell NMR requires intracellular delivery of biomolecules at sufficient concentrations without compromising cell viability or biomolecule functionality [73].
- Solution:
- Use a two-step delivery strategy: For RNA-protein complexes, endogenously express the protein (e.g., HIV-1 Tat) via plasmid transfection. Subsequently, introduce the RNA component (e.g., Tat RNA aptamer) using electroporation [73].
- Verify delivery and localization: Use confocal fluorescence microscopy to confirm nuclear co-localization of the protein and RNA, ensuring the interaction occurs in the correct subcellular compartment [73].
- Check expression levels: Validate protein expression by Western blotting and monitor transfection efficiency using a co-delivered reporter like GFP on a separate plasmid [73].
FAQ 2: The in-cell NMR spectrum has poor quality or low signal. What are the common causes?
- Problem: Sample-related issues or incorrect NMR parameters can lead to poor spectral quality.
- Solution:
- Avoid high salt concentrations: High salt can disrupt automatic tuning and matching (ATM). For critical samples, consider manually adjusting the tuning or disabling ATM with NMR staff assistance [74].
- Use proper dataset naming: NMR data processing can fail if the dataset name contains spaces or special characters. Use short names with underscores (e.g., "abc_1001") instead of spaces [74].
- Handle solvent suppression correctly: For samples in protonated solvents (e.g., H2O), set the solvent to "None" and use specific experiments like "WATER.ucl" to suppress the large solvent peak [74].
FAQ 3: How do I confirm that an interaction observed via in-cell NMR is specific and biologically relevant?
- Problem: The crowded cellular environment can cause non-specific interactions.
- Solution:
- Look for characteristic NMR signatures: Monitor for Chemical Shift Perturbations (CSPs) and specific Nuclear Overhauser Effect (NOE) patterns that indicate a structured complex, as demonstrated for the HIV Tat-aptamer complex in cells [73].
- Compare with in vitro data: Directly compare in-cell NMR spectra with spectra of the purified complex obtained in vitro. A close match confirms the structural integrity and specificity of the intracellular complex [73].
- Perform control experiments: Use mutagenesis or binding-deficient variants of the protein or RNA to confirm that the observed NMR changes are due to a specific interaction [75].
Table 2: Troubleshooting In-Cell NMR Experiments
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor Biomolecule Delivery [73] | Low efficiency; cell death | Use two-step strategy (transfection + electroporation); confirm with microscopy. |
| Poor Spectral Quality [74] | High salt; improper parameters | Manually tune/match for salty samples; use correct dataset naming. |
| Uncertain Interaction Specificity [73] | Non-specific crowding effects | Check for CSPs/NOEs; compare with in vitro spectra; run binding-deficient controls. |
Experimental Protocols
Detailed Protocol: Characterizing a Genetically Encoded Potassium Sensor in Neurons
This protocol is adapted from in vitro and in vivo characterization of lc-LysM GEPII 1.0 [22].
1. Sensor Preparation and Validation
- Cloning: Subclone the sensor ORF (e.g., cytosolic-targeted cyto-lc-LysM GEPII 1.0) into an AAV backbone under a neuron-specific promoter (e.g., hSyn).
- Protein Purification: Transform a bacterial expression plasmid into Rosetta (DE3) cells. Induce protein expression with 0.5 mM IPTG at 18°C for 16 hours. Purify the 6xHis-tagged sensor using Ni-NTA affinity chromatography.
- In Vitro Characterization: Dilute purified protein in HEPES buffer with K+ concentrations ranging from 0-150 mM (maintain total ion concentration with Na+). Acquire fluorescence lifetime calibration curves using a microscope or plate reader.
2. In Vitro Neuronal Imaging
- Primary Neuron Culture: Plate primary neurons and transfer with the AAV-sensor construct.
- Imaging Setup: Use a microscope capable of FRET/FLIM imaging. For lc-LysM GEPII 1.0, two-photon excitation at 850 nm and emission collection at 450-500 nm is suitable.
- Stimulation and Recording: To elicit large K+ fluxes, perfuse with a solution inducing seizure-like activity or use optogenetic stimulation (e.g., Channelrhodopsin). Record fluorescence lifetime changes at a frame rate of 1 frame/2 seconds.
3. In Vivo Imaging in Mouse Cortex
- Viral Injection: Produce AAV particles in HEK293T cells and inject them into the mouse cortex for neuronal expression of the sensor.
- Cranial Window Surgery: Implant a cranial window over the injection site for optical access.
- Two-Photon FLIM: Anesthetize the mouse and perform in vivo 2-photon fluorescence lifetime imaging. Induce events like peri-infarct depolarizations and record the associated lifetime increases, which indicate a decrease in intracellular neuronal [K+].
Detailed Protocol: Observing Endogenous RNA-Protein Complexes in Human Cells via In-Cell NMR
This protocol is based on the study of the HIV Tat protein and its RNA aptamer in HeLa cells [73].
1. Intracellular Expression and Delivery
- Cell Culture: Grow HeLa cells in high-glucose DMEM with 10% FBS at 37°C and 5% CO2.
- Protein Expression: Transfert cells with a plasmid encoding the full-length HIV-1 Tat protein (under a CMV promoter) using a transfection reagent like Lipofectamine 3000. Incubate for 48 hours.
- RNA Electroporation: Introduce the purified Tat RNA aptamer into the Tat-expressing cells via electroporation.
2. In-Cell NMR Spectroscopy
- Sample Preparation: After electroporation, transfer the cells into an NMR tube. The cell density must be sufficiently high to obtain a good signal.
- Data Acquisition: Acquire 1H-15N HSQC spectra to monitor chemical shift perturbations. To obtain structural information, conduct NOESY experiments directly in the living cells.
- Specificity Controls: Compare the in-cell NMR spectra with in vitro spectra of the purified Tat-aptamer complex. The similarity of CSPs and NOE patterns confirms specific binding within the cell.
3. Validation via Confocal Microscopy
- In parallel, use confocal fluorescence microscopy to validate the nuclear co-localization of the Tat protein and the RNA aptamer, confirming the interaction occurs in the correct functional compartment.
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| lc-LysM GEPII 1.0 | FRET-based genetically encoded K+ ion indicator for measuring intracellular [K+] dynamics [22]. | Can be targeted to cytosol, plasma membrane, or mitochondria. Requires characterization for small vs. large [K+] changes. |
| HIV-1 Tat Protein | Model intrinsically disordered protein for studying RNA-protein interactions in cells [73]. | Full-length (86 aa) protein can be expressed endogenously in HeLa cells from a mammalian expression plasmid. |
| Tat RNA Aptamer | Engineered RNA with high-affinity for HIV-1 Tat protein; mimics native TAR element [73]. | Used to study de novo complex formation inside living human cells; introduced via electroporation. |
| AAV Vectors | For cell-type-specific delivery and expression of genetically encoded sensors in vitro and in vivo [22]. | Use with specific promoters (e.g., hSyn for neurons, GFAP for astrocytes). AAV-DJ serotype provides broad tropism. |
| HEK293T Cells | Workhorse cell line for producing AAV vectors and for protein expression [22]. | Used in AAV production via triple transfection with pHelper and pAAV-DJ plasmids. |
Experimental Workflows and Signaling Pathways
Diagram 1: Workflow for In-Cell NMR Study of an RNA-Protein Complex
Diagram 2: Neuronal Potassium Sensing with a Genetically Encoded Indicator
Diagram 3: Key Signaling Pathway Linking Neuronal Activity to Potassium Flux
FAQs: Cytomimetic Conditions & Ion Optimization
Q1: What is the fundamental role of potassium (K+) and sodium (Na+) in cytomimetic experiments? K+ and Na+ are critical electrolytes that form the sodium-potassium pump (Na+/K+ ATPase). This pump regulates the cellular movement of sodium and potassium ions, which determines how much water stays inside or outside your cells. This mechanism is fundamental for maintaining the body's fluid levels, supporting nerve signaling, regulating muscle contractions, and balancing blood pressure [48]. In cytomimetic research, replicating this ionic environment is essential for creating biologically relevant conditions that accurately reflect cellular physiology.
Q2: Why is the K+:Na+ ratio specifically important for creating valid cytomimetic conditions? An optimal potassium-to-sodium intake ratio is crucial for cardiovascular health and overall wellness. While it's widely believed that a low-sodium diet has health benefits, it's more critical to achieve a balanced sodium-to-potassium intake. Evidence highlights the importance of this balance to support optimal cardiovascular health. For most adults, the optimal sodium-to-potassium ratio is approximately 4700 mg of potassium to 2300 mg of sodium per day, which is a ratio of about 1:2 in terms of sodium to potassium [48]. An imbalance can disrupt various cellular processes.
Q3: What are the common signs that my cytomimetic ionic conditions are suboptimal? Common signs of imbalanced sodium and potassium levels that can mirror issues in cellular models include high blood pressure, fluid retention and swelling, muscle cramps, irritability, and a rapid heartbeat [48]. In a research context, these translate to poor cell viability, erratic signaling behavior, and unreliable assay data.
Q4: Which medications should I be cautious of, as they might interfere with cellular K+ and Na+ levels? Hundreds of medications can affect potassium levels. When designing experiments, consider that compounds like Angiotensin-converting enzyme (ACE) inhibitors, Angiotensin receptor blockers (ARBs), and potassium-sparing diuretics can cause hyperkalemia (high potassium). Conversely, diuretics like hydrochlorothiazide and furosemide, as well as medications for COPD, can cause hypokalemia (low potassium) [76]. This is a critical consideration when testing drug candidates in cytomimetic systems.
Troubleshooting Guides
Issue 1: Poor Biomimicry and Unpredictable Cellular Behavior
Potential Cause: Incorrect intracellular and extracellular ionic concentrations, leading to a failure in replicating the native environment for the cells or cellular components being mimicked.
Solution:
- Step 1: Quantitatively validate the ion concentrations in your buffers and media. The following table summarizes key quantitative targets based on physiological principles:
Table 1: Target Ionic Concentrations for Cytomimetic Conditions
| Ion | Recommended Daily Physiological Intake [48] | Considerations for Cytomimetic Media |
|---|---|---|
| Potassium (K+) | 4700 mg (~120 mmol) | Crucial for maintaining resting membrane potential. |
| Sodium (Na+) | 2300 mg (~100 mmol) | Primary contributor to extracellular osmolarity and action potentials. |
| K+:Na+ Ratio | 1:2 (Sodium to Potassium) | A target for balancing electrochemical gradients. |
- Step 2: Incorporate the use of the "Nonlinear Bernoulli Cell Formalism" (NBCF). This is a transistor-level synthesis framework capable of converting coupled, nonlinear biological differential equations into coupled, nonlinear electrical differential equations and subsequently into ultra-low power log-domain electrical circuits, or "Cytomimetic" circuits. This systematic approach ensures your electronic or chemical models accurately compute nonlinear biological dynamics [77].
- Step 3: For research involving viral mechanisms, be aware that molecular mimicry is a common strategy. Ensure your cytomimetic systems can account for this, as viruses mimic host protein structures to evade the immune system, which can be a confounder in assays [78].
Issue 2: Low Signal-to-Noise Ratio in Binding or Uptake Assays
Potential Cause: Inefficient competition between cytomimetic decoys and native cellular receptors.
Solution:
- Step 1: Optimize the stoichiometry of your decoy receptors. Proof-of-concept studies on cytomimetics, such as ACE2-functionalized particles for SARS-CoV-2 research, have demonstrated that particle-functionalized receptors are stoichiometrically superior to soluble versions. These cytomimetic particles can bind viral proteins with high affinity at a ratio of greater than 1:2.5 (viral protein: cytomimetic receptor) [79].
- Step 2: Choose the appropriate cytomimetic platform. Inhaled delivery of cell-mimetic microparticles (cytomimetics) has proven effective for prophylactically restricting viral uptake in respiratory epithelium, showcasing a viable method for interference and sequestration of target ligands [79].
- Step 3: Validate binding affinity rigorously. Use techniques like western blot analysis and immunofluorescence imaging to confirm the binding efficacy of your functionalized cytomimetic particles and their ability to outcompete native cellular receptors [79].
Experimental Protocols
Protocol 1: Fabrication and Functionalization of Receptor-Based Cytomimetic Particles
This protocol is adapted from methods used to create ACE2-cytomimetic particles for viral sequestration [79].
Methodology:
- Particle Selection: Use HisPur Ni-NTA magnetic beads or similar as the core particle.
- Receptor Functionalization: Incubate the beads with an excess molar amount of your recombinant, His-tagged protein of interest (e.g., a receptor like rhACE2) by overnight incubation under constant rotation in an appropriate binding buffer.
- Washing: Magnetically separate the functionalized particles and wash thoroughly to remove any unbound protein.
- Control Preparation: Manufacture control particles in the same manner but replace the active protein with an inert protein like Bovine Serum Albumin (BSA) to assess non-specific interactions.
Validation Assay:
- In vitro Binding Test: Combine the functionalized cytomimetic particles with the target ligand (e.g., a viral spike protein) at increasing ratios. Incubate overnight under constant rotation.
- Analysis: Determine the amount of bound ligand versus free-floating ligand using western blotting. A successful functionalization will show high binding efficacy at the expected ratios [79].
Protocol 2: Systematic Design of CytoMimetic Electronic Circuits via NBCF
This protocol outlines the process for designing ultra-low-power analog circuits that emulate biological dynamics [77].
Methodology:
- Model Definition: Start with the coupled, nonlinear biological differential equations that describe the system you wish to emulate (e.g., cellular cycle dynamics, glycolytic oscillations).
- NBCF Application: Use the Nonlinear Bernoulli Cell Formalism (NBCF) to systematically convert the biological differential equations into coupled, nonlinear electrical differential equations.
- Circuit Synthesis: Translate the electrical equations into an ultra-low power log-domain electrical circuit topology. The NBCF provides a framework for this modular synthesis and analysis.
- Simulation & Fabrication: Simulate the circuit dynamics using a standard simulator (e.g., SPICE). Upon successful simulation, proceed to chip fabrication. Proof-of-concept chips have been built in 0.35 μm BiCMOS processes, consuming very low power (e.g., 1.26 μW) [77].
Signaling Pathways & Workflows
Cytomimetic Decoy Sequestration Mechanism
This diagram illustrates the mechanism by which cytomimetic particles act as decoys to protect host cells.
Experimental Workflow for Cytomimetic Circuit Design
This diagram outlines the key steps in the NBCF methodology for creating cytomimetic circuits.
Research Reagent Solutions
Table 2: Essential Materials for Cytomimetic Research
| Item | Function / Explanation | Example / Source |
|---|---|---|
| HisPur Ni-NTA Magnetic Beads | Core particle for facile functionalization of His-tagged recombinant proteins to create cytomimetic decoys. | ThermoFisher Scientific [79] |
| Recombinant Human Receptors | Key functionalizing component (e.g., rhACE2) that confers specific binding affinity to the cytomimetic particle. | R&D Systems [79] |
| Nonlinear Bernoulli Cell Formalism (NBCF) | A systematic, in-house developed synthesis framework for converting biological dynamics into analog electronic circuits. | Academic Theses & Literature [77] |
| Ultra-Low-Power Log-Domain Circuits | The resulting hardware (e.g., 1.26 μW ICs) that physically emulate nonlinear cellular and molecular dynamics. | Custom Fabrication [77] |
| Potassium & Sodium Standards | High-purity salts to prepare buffers and media with physiologically accurate K+ and Na+ concentrations and ratios. | Various Chemical Suppliers [48] |
Conclusion
Accurately mimicking the intracellular environment by optimizing K+ and Na+ levels is not a minor technical adjustment but a fundamental requirement for predictive in vitro research. Moving beyond conventional buffers like PBS to cytomimetic formulations that reflect the high-K+, low-Na+ intracellular reality can dramatically reduce the discrepancy between biochemical and cellular assays, leading to more reliable structure-activity relationships and a higher success rate in drug discovery. Future directions should focus on the development of standardized, organelle-specific cytomimetic buffers and the wider adoption of advanced in-cell validation techniques. Embracing this paradigm shift will bring in vitro models closer to physiological truth, de-risking the pipeline from bench to bedside.
References
- 1. Mature cathepsin L is substantially active in the ionic of the... milieu [https://pubmed.ncbi.nlm.nih.gov/7503566/]
- 2. and Potassium shifts during in vitro isometric muscle... sodium [https://link.springer.com/article/10.1007/BF00583367]
- 3. Physiology, Sodium Potassium Pump - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK537088/]
- 4. Sodium–potassium pump - Wikipedia [https://en.wikipedia.org/wiki/Sodium%E2%80%93potassium_pump]
- 5. Frontiers | The Slow Dynamics of Intracellular Concentration... Sodium [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2017.00085/full]
- 6. activities of Intracellular and sodium potassium [https://pubmed.ncbi.nlm.nih.gov/347946/]
- 7. Active Transport | Biology for Non-Majors I [https://courses.lumenlearning.com/wm-nmbiology1/chapter/reading-active-transport/]
- 8. 2.6 Membrane Transport | AP Biology Notes | TutorChase [https://www.tutorchase.com/notes/ap/biology/2-6-membrane-transport]
- 9. of Mechanisms - AP Bio Study Guide Transport [https://fiveable.me/ap-bio/unit-2/tonicity-osmoregulation/study-guide/CCENUydXNVb7K4P7ikp7]
- 10. Electrolytes - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK541123/]
- 11. The electrogenicity of the Na+/K+-ATPase poses challenges for computation in highly active spiking cells [https://elifesciences.org/reviewed-preprints/103781]
- 12. +/ Na +- K : More than an ATPase Pump - PMC Electrogenic [https://pmc.ncbi.nlm.nih.gov/articles/PMC11172918/]
- 13. The sodium-potassium pump is an information processing element in brain computation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4274886/]
- 14. Preclinical Development of the Na-K-2Cl Co-transporter-1 (NKCC1) Inhibitor ARN23746 for the Treatment of Neurodevelopmental Disorders - PubMed [https://pubmed.ncbi.nlm.nih.gov/36654749/]
- 15. Preclinical Development of the Na-K-2Cl Co-transporter-1 (NKCC1) Inhibitor ARN23746 for the Treatment of Neurodevelopmental Disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9841778/]
- 16. Modulation of the Na , K - ATPase by Ca and intracellular proteins [https://pubmed.ncbi.nlm.nih.gov/2837135/]
- 17. The electrogenicity of the Na +/ K +- ATPase poses challenges for... [https://elifesciences.org/reviewed-preprints/103781v2]
- 18. Toxicological effects of cobalt on common carp: oxidative stress, ionic ... [https://link.springer.com/article/10.1007/s10653-025-02407-x]
- 19. Toxicological effects of cobalt on common carp: oxidative stress, ionic ... [https://pubmed.ncbi.nlm.nih.gov/40035912/]
- 20. How extracellular potassium affects intracellular pool in... sodium [https://pubmed.ncbi.nlm.nih.gov/1332719/]
- 21. Electrolyte Imbalance: Types, Symptoms, Causes & Treatment [https://my.clevelandclinic.org/health/symptoms/24019-electrolyte-imbalance]
- 22. Probing intracellular potassium dynamics in with the... neurons [https://www.nature.com/articles/s41598-024-62993-1?error=cookies_not_supported&code=cf034204-f17b-4d92-b300-ca0326f9817b]
- 23. Nervous system - Sodium-Potassium Pump, Active Transport, Neurotransmission | Britannica [https://www.britannica.com/science/nervous-system/Active-transport-the-sodium-potassium-pump]
- 24. Activity-mediated accumulation of potassium induces a switch in firing pattern and neuronal excitability type | PLOS Computational Biology [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1008510]
- 25. Lidocaine increases intracellular sodium concentration through... [https://pubmed.ncbi.nlm.nih.gov/18420861/]
- 26. The influence of sodium and potassium dynamics on excitability, seizures, and the stability of persistent states: I. Single neuron dynamics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2704057/]
- 27. Establishment of a method to measure the intracellular potassium ion... [https://www.aimspress.com/article/doi/10.3934/Neuroscience.2024018]
- 28. Regulation of intracellular chloride by cotransporters in developing... [https://pubmed.ncbi.nlm.nih.gov/10191302/]
- 29. Comparative Analysis of Biochemical and Cellular Assay Conditions and the Need for a Buffer That Mimics Cytoplasmic Environments - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429910/]
- 30. Transcription and Translation in Cytomimetic Protocells Perform Most Efficiently at Distinct Macromolecular Crowding Conditions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7573978/]
- 31. Changes in intracellular and potassium content of 2-cell... sodium [https://pubmed.ncbi.nlm.nih.gov/16794740/]
- 32. (PDF) Flow Cytometry Method Validation Protocols [https://www.academia.edu/102913540/Flow_Cytometry_Method_Validation_Protocols]
- 33. 5 Recipes for Flow Cytometry Buffers - FluoroFinder [https://fluorofinder.com/flow-cytometry-buffers/]
- 34. Flow Cytometry Troubleshooting Guide: Novus Biologicals [https://www.novusbio.com/support/support-by-application/flow-cytometry/troubleshooting]
- 35. Frontiers | Application of ITC-Based Characterization of... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.01133/full]
- 36. Analyzing Kinetic Binding Data - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK569501/]
- 37. Ligand binding assays at equilibrium: validation and interpretation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3000649/]
- 38. High-throughput screening - Wikipedia [https://en.wikipedia.org/wiki/High-throughput_screening]
- 39. Adaptation of High-Throughput Screening in Drug Discovery—Toxicological Screening Tests - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3269696/]
- 40. Membrane potential: the basis of action potentials | Kenhub [https://www.kenhub.com/en/library/physiology/membrane-potential]
- 41. Potassium Permeability - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/engineering/potassium-permeability]
- 42. Drug Solubility: Importance and Enhancement Techniques - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3399483/]
- 43. Salt formation to improve drug solubility - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0169409X07000816]
- 44. Different Permeability of Potassium Salts across the Blood-Brain Barrier Follows the Hofmeister Series - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3810376/]
- 45. of Organic Salts in Solvent–Antisolvent Mixtures... Solubility [https://pmc.ncbi.nlm.nih.gov/articles/PMC9367008/]
- 46. 3 Methodological Considerations | Dietary Reference Intakes for... [https://nap.nationalacademies.org/read/25353/chapter/6]
- 47. +/ Na +-pump and neurotransmitter membrane receptors | Invertebrate... K [https://link.springer.com/article/10.1007/s10158-018-0221-7]
- 48. Is Your Sodium-Potassium Ratio Off? Why It Matters | Dr. Berg [https://www.drberg.com/blog/your-potassium-sodium-ratio-should-be-4-to-1]
- 49. Relationship and interaction between sodium and potassium [https://pubmed.ncbi.nlm.nih.gov/16772638/]
- 50. Optimal timing for measuring the casual urine Na/K ratio using a single sample: insights from a comparison with 24-h urine samples | Hypertension Research [https://www.nature.com/articles/s41440-024-02039-1]
- 51. Know Your Biomarkers: Sodium Potassium Ratio [https://www.optimaldx.com/blog/sodium-potassium-ratio]
- 52. An X-ray microanalysis study of Locusta Malpighian tubule cell function... [https://pubmed.ncbi.nlm.nih.gov/8203632/]
- 53. Revealing the Origin of Property Discrepancy in KNN-Based Ceramics... [https://pubmed.ncbi.nlm.nih.gov/40270207/]
- 54. Systematic study of the influence of the K / Na on the structure... ratio [https://link.springer.com/article/10.1007/s10854-022-09475-0]
- 55. Connecting the Dots: The Effects of Macromolecular on... Crowding [https://pmc.ncbi.nlm.nih.gov/articles/PMC4269789/]
- 56. Dietary, total body, and intracellular -to- potassium and... sodium ratios [https://pubmed.ncbi.nlm.nih.gov/2224920/]
- 57. Physiological Mechanisms Underlying High Salt Diets... - The Paleo Diet [https://thepaleodiet.com/physiological-mechanisms-underlying-high-salt-diets-cancer/]
- 58. Development of Nano ZnO-Embedded Gelatin/Alginate Bioscaffolds for Potential Skin Tissue Regeneration via Oxidative Stress Modulation and ECM Mimicry - PubMed [https://pubmed.ncbi.nlm.nih.gov/40847847/]
- 59. Electrolyte disturbances: causes and... - The Pharmaceutical Journal [https://pharmaceutical-journal.com/article/ld/electrolyte-disturbances-causes-and-management]
- 60. 10.3: Electrolyte Imbalance - Medicine LibreTexts [https://med-libretexts-org.translate.goog/Bookshelves/Nursing/Medical-Surgical_Nursing_(OpenStax)/10:_Fluid_Electrolyte_and_Acid-Base_Imbalances/10.03:_Electrolyte_Imbalance?_x_tr_sl=en&_x_tr_tl=pt&_x_tr_hl=pt-PT&_x_tr_pto=tc]
- 61. IC50, EC50 and Kd : What is the Difference... - Promega Connections [https://www.promegaconnections.com/ic50-ec50-and-kd-what-is-the-difference-and-why-do-they-matter/]
- 62. How to measure and evaluate binding affinities | eLife [https://elifesciences.org/articles/57264]
- 63. determination from time-resolved experiments on live KD with... cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC8448686/]
- 64. Ions - Sodium and Potassium Explained: Definition, Examples, Practice & Video Lessons [https://www.pearson.com/channels/anp/learn/bruce/nervous-tissue-and-nervous-system/ions-sodium-and-potassium]
- 65. Potassium: From Physiology to Clinical Implications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4947686/]
- 66. (+) and metabolic modulation of Intracellular / Na pump and... Na K [https://pubmed.ncbi.nlm.nih.gov/22773774/]
- 67. Frontiers | Astrocytic and neuronal accumulation of elevated... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2013.00114/full]
- 68. Exposure to Buffer Solution Alters Tendon Hydration and Mechanics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5659756/]
- 69. How to choose and use antibodies | Abcam [https://www.abcam.com/en-us/technical-resources/guides/antibody-basics/how-to-choose-and-use-antibodies]
- 70. Phosphate-buffered saline - Wikipedia [https://en.wikipedia.org/wiki/Phosphate-buffered_saline]
- 71. Probing intracellular potassium dynamics in neurons with the genetically encoded sensor lc-LysM GEPII 1.0 in vitro and in vivo | Scientific Reports [https://www.nature.com/articles/s41598-024-62993-1]
- 72. Guide to Ion Selective | Troubleshooting | Support | Turtle Tough [https://www.turtletoughsensors.com/support/troubleshooting/guide-to-ise]
- 73. - In reveals the first cell observation of endogenous... NMR direct [https://www.nature.com/articles/s41598-025-12791-0?error=cookies_not_supported&code=67c97210-8ab2-4e9b-9467-dc8f0ae4395d]
- 74. Common Problems | UCL Chemistry NMR Instruments [https://www.ucl.ac.uk/nmr/common-problems]
- 75. Applications of In - Cell in Structural Biology and Drug Discovery... NMR [https://pmc.ncbi.nlm.nih.gov/articles/PMC6337603/]
- 76. What medications can affect potassium ? levels [https://www.drugs.com/medical-answers/medications-affect-potassium-levels-3566412/]
- 77. Advanced cytomimetic circuits: design optimisation and fabrication [https://www.semanticscholar.org/paper/Advanced-cytomimetic-circuits%3A-design-optimisation-Houssein/f1e3773fda737c642c447e7927979b3af5cc16de]
- 78. Molecular mimicry as a mechanism of viral immune evasion and autoimmunity | Nature Communications [https://www.nature.com/articles/s41467-024-53658-8]
- 79. ACE2- cytomimetic particles restrict SARS -Cov-2 spike protein binding... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8482554/]